3 Postnatal growth of the craniofacial region
The adult skull is composed of twenty-eight individual bones and represents one of the most complex regions of the body. The skull bones either develop from a cartilaginous template, ossify directly from membrane, or are composite, being formed following contributions from both mechanisms (Fig. 3.1). Growth of this region therefore represents a combination of endochondral and periosteal modes of osteogenesis.

Figure 3.1 Human fetus at around 20 weeks of embryonic development, stained with Alizarin red and cleared.
Courtesy of the Gordon Museum, King’s College London.
An understanding of the mechanisms underlying craniofacial growth is important for the orthodontist:
General growth of the body
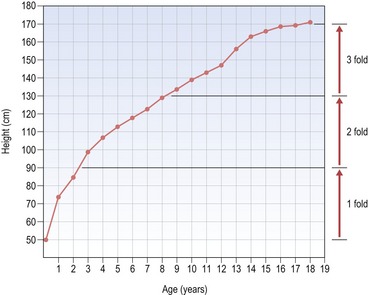
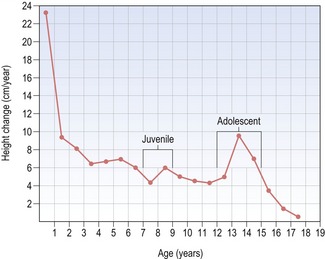
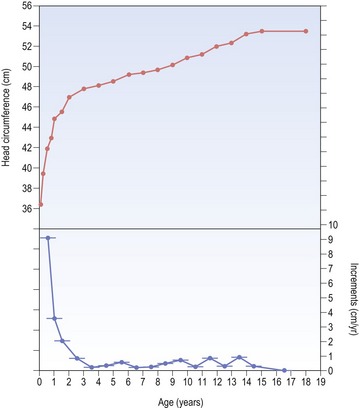
A simple plot of height versus age (or height-distance curve) for either males or females reveals a relatively smooth and constant increase that occurs from birth to the late teenage years and results in an approximate threefold increase in height (Fig. 3.2). However, the height versus age curve does not demonstrate the dynamic changes in growth rate or velocity that occur from birth to adulthood. To do this, an incremental plot of height change, or a height–velocity curve is required, which shows three general phases in the growth curve (Fig. 3.3):
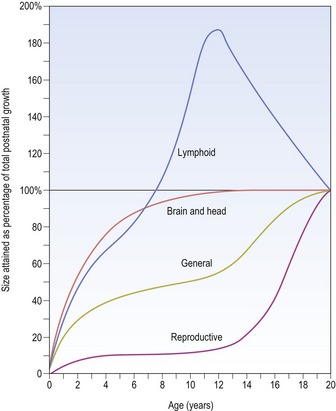
In contrast, other body tissues demonstrate quite different patterns of growth in comparison to height. For example, the central nervous system is well developed at birth and grows rapidly during the early years of life, being essentially complete by approximately 10 years of age; whilst the reproductive organs do not begin to increase in size until puberty (Fig. 3.4).
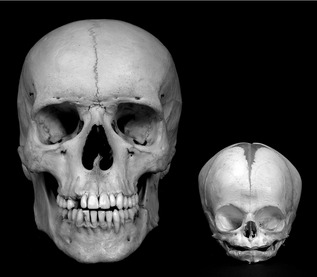
The skull at birth
One of the most striking features of a newborn child is the large size of the head in relation to the rest of the body (Fig. 3.5). This is because at birth, the cranial vault is approximately two-thirds of its final dimension, due to extensive prenatal growth and development of the brain. However, despite this large size the skull of the neonate differs significantly from that of an adult (Fig. 3.6):
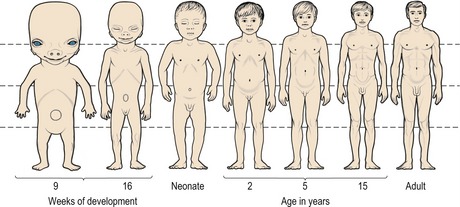
Figure 3.5 Changes in body proportions from the fifth month postconception to maturity.
Note the large size of the head in relation to the rest of the body at birth.
Redrawn from Medawar PB (1945), The shape of the human being as a function of time. Proc R Soc Lond 132:133–141.
Rapid growth of the cranial vault continues for the first year after birth, but this progressively decreases during the next two years and remains at a low level until adulthood (Fig. 3.7). However, by 5 years of age around 90% of the adult cranial dimension has been attained. Significantly, the dimensions of the cranium are not affected by the pubertal growth spurt.
Mechanisms of craniofacial bone growth
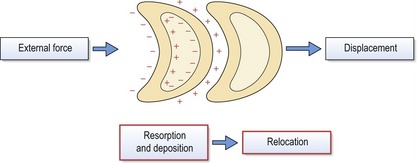
It is clear from the direct comparison of different skull bones that postnatal growth of the craniofacial region does not result from a simple proportional enlargement of each individual bony element (Fig. 3.8). Endochondral bone growth occurs through cartilaginous replacement, whilst intramembranous bones grow as a result of periosteal remodelling. The complexity and diversity of the skull arises because the constituent bones enlarge differentially, in both a temporal and spatial manner (Fig. 3.9). The basic mechanisms underlying growth of the craniofacial region reflect this and produce:
Theories of craniofacial growth
Several theories that attempt to explain the mechanisms controlling postnatal growth of the craniofacial skeleton have been proposed. These theories have placed varying degrees of emphasis upon the role of genetic and environmental factors, or the significance of different tissues within this region; some being based upon experimental and biological observation and others having a more theoretical basis (Carlson, 2005).
The sutural theory
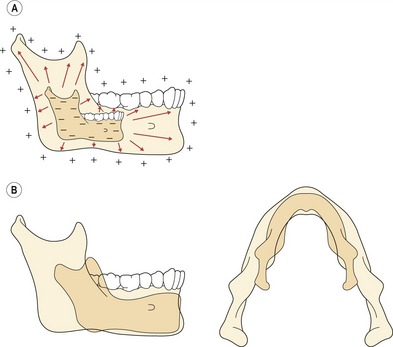
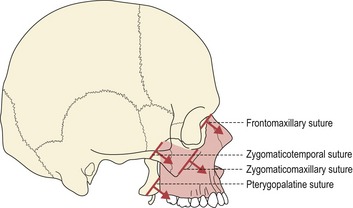
The sutural theory was largely the work of two anatomists, Joseph Weinmann and Harry Sicher, who suggested that primary growth of the craniofacial skeleton was genetically regulated, being controlled within the sutures and cartilages. Importantly, within this model, the sutures had an equivalent role to cartilage in being able to generate a tissue-separating force. For the cranial vault and maxillary complex, sutural growth was regarded as being the prime mediator of bony expansion and, in the case of the maxilla, downward and forward displacement relative to the anterior cranial base (Fig. 3.10).
The cartilaginous theory
In direct contrast to the sutural theory another anatomist, James Scott, suggested that sutures simply represented a continuation of the periosteum and endosteum of the craniofacial bones, in modified regions at their points of intersection. Growth in these regions should therefore be considered as periosteal in nature, being permissive rather than producing a tissue-separating force. Scott suggested that the bones abutting a suture could only be separated by the growth of an associated organ, such as the brain in the case of the cranial vault. Within this theory, great emphasis was placed upon the role of cartilage in producing the driving force of craniofacial growth: in particular, the nasal septal cartilage generating a downward and forward displacement of the maxillary complex, synchondroses elongating the cranial base and the condylar cartilage directing downward and forward growth of the mandible (Scott, 1953; 1954; “>1956).
The functional matrix theory
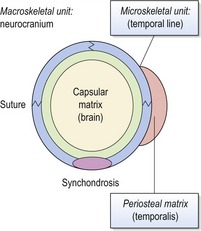
The functional matrix theory of Melvin Moss describes bone growth within the craniofacial skeleton as being influenced primarily by function (Moss and Salentijn, 1969). In contrast to both the sutural and cartilaginous theories, this theory does not assume that growth of the skull is genetically determined. Indeed, this theory suggests that genes play no major role in determining postnatal growth of the craniofacial region.
Skeletal units are also further subdivided into:
Each skeletal unit does not necessarily represent an individual bone within the skull, some bones being composed of several microskeletal units or several bones uniting together to function as a single cranial component or macroskeletal unit. In general, the periosteal matrices primarily determine growth of microskeletal units, influencing the size and shape of bones; whilst macroskeletal growth is influenced more by the capsular matrices, producing displacement of cranial regions, such as the nasomaxillary complex or cranial vault (Fig. 3.11).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses