Introduction
The aim of this study was to assess unilateral posterior crossbite, sucking habits, orofacial functions, and otolaryngological findings in the deciduous dentition. These findings would allow us to establish a preventive program for posterior crossbite, based on interceptive treatment at an early stage of dental development. We would determine the predictive value for posterior crossbite development in correlation with the duration of sucking habits.
Methods
Data were collected on 30 children (13 boys, 17 girls) with unilateral posterior crossbite (mean age, 5.5 years; range, 3.6-7.2 years) and 30 children (17 boys, 13 girls) without crossbite (mean age, 5.9 years; range, 5.4-6.7 years), randomly selected from a local kindergarten. Information about each subject’s nutritive and nonnutritive sucking behaviors was collected through parent interviews and questionnaires. An orthodontist and an otolaryngologist clinically examined all the children. Study models were obtained from all children, and dental arch parameters including arch widths in the canine and second deciduous molar regions were measured directly from the models. The data were then compared between the posterior crossbite and the noncrossbite groups.
Results
The results indicated correlations between prolonged pacifier sucking habit ( P = 0.001), short frenulum linguae ( P <0.001), smaller maxillary arch width ( P <0.001), greater mandibular arch width ( P <0.002), and unilateral posterior crossbite. A receiver operating characteristic curve was plotted for the pacifier sucking time. The borderline for the development of posterior crossbite suggested by the receiver operating characteristic curve was 18 months of pacifier sucking duration. The odds ratios between the crossbite and noncrossbite groups were 3.6 (CI = 0.97-13.4) for pacifier habit duration of 18 to 35 months and 21.9 (CI = 3.7-129.4) for pacifier suckers of more than 36 months. No significant correlation between enlarged adenoids and tonsils or impaired nasal breathing and the crossbite was found.
Conclusions
These results suggest that the duration of a pacifier habit and a short frenulum linguae are associated with posterior crossbite at the age of 4 or 5 years because of the low tongue posture in the mouth. Pediatricians and pedodontists should give precise recommendations for enhancing breast feeding and discontinuing pacifier habits at least until the child is 18 months of age. Further studies are also needed to determine more objectively the etiology of tongue posture, swallowing pattern, and the length of the frenulum linguae in children with posterior crossbite.
Today’s emphasis on preventive orthodontic care necessitates rational planning of orthodontic preventive measures among children even in an early stage of dental development. Posterior crossbite is the most prevalent malocclusion in the deciduous dentitions of white children. Without early treatment, it can result in facial asymmetry and temporomandibular disorders in adulthood. Furthermore, the muscular hyperactivity on the crossbite side might have an unfavorable influence on craniofacial growth that can lead to craniofacial asymmetry or temporomandibular joint (TMJ) dysfunction and deviation from normal facial esthetics.
The functional matrix theory of growth and development by Moss presumes that growth of the face occurs as a response to functional needs and neurotrophic influences, and is mediated by the soft tissues in which the jaws are embedded. In this conceptual view, the soft tissues grow, and both bone and cartilage react. The conclusion, based on Moss’s theory, is that the correct functions of the orofacial complex—breathing, swallowing, and chewing—have a major influence on the growth and correct development of face, jaws, and dentition.
In addition to heredity, other factors involved in the etiology of posterior crossbite are nonnutritive sucking habits and impaired nasal breathing caused by, for example, enlarged tonsils and adenoids. In a review of the literature by Allen et al, the following potential etiologic factors for posterior crossbite were given: prolonged retention or premature loss of deciduous teeth, crowding, palatal cleft, genetic control, arch deficiencies, abnormalities in tooth anatomy or eruption sequence, oral digit habits, oral respiration during critical growth periods, and malfunctioning TMJs. Many authors found that pacifier sucking is an important etiologic factor involved in the formation of a posterior crossbite.
Bottle feeding, even among breast-fed children, interfered negatively with orofacial development. Lip competence closure, nasal breathing, resting tongue position in the maxillary arch, and normal maxilla were observed statistically significantly more often in children who used only a cup to drink.
Open-mouth posture, as a habit or as a result of adeno-tonsillar enlargement or prolonged inflammation of the nasal mucosa associated with allergies or chronic infections, inhibits transverse maxillary growth and leads to a significant increase in the prevalence of posterior crossbite. It is also connected with posterior head posture and facies adenoidea. It seems that, in children with posterior crossbite and those who breathe through their mouth, excessive vertical dimension is associated with deficient transverse dimension; nevertheless, the true relationship between mouth breathing and posterior crossbite is still in question. Lip incompetence plays an important role in the growth and development of the craniofacial complex, although the open-mouth posture does not reflect the mode of breathing.
Children with enlarged tonsils had significantly narrower maxillary arches and a higher prevalence of posterior crossbite; crossbite was also correlated with functional disorders such as open-mouth posture, mouth breathing during sleep, snoring, guttural speech, and dysphagia. Children with enlarged tonsils were found to have a more anterior and inferior position of the tongue and a more inferior position of the hyoid bone than those without enlarged tonsils.
Swallowing pattern progresses from an infantile form, which can persist until 4 years of age, to a mature form. If this does not happen because of obstacles in the mouth that prevent the normal position of the tongue (dummy, finger), the tongue must take a lower position in the anterior part of the mouth. Infantile swallowing pattern is considered a dysfunction because of its association with certain malocclusions.
The development of an occlusion must be considered a result of the interactions between genetically determined developmental factors and several external and internal environmental factors, including orofacial functions. Whereas a close relationship between form and function is recognized by many authors, the degree of interplay is still a matter of conjecture. There has been no report in the literature on interdisciplinary clinical examinations of orofacial functions in the primary dentition period by an orthodontist and otolaryngologist.
Therefore, our aim in this study was to find the association between posterior crossbite, sucking habits, orofacial functions, and otolaryngologic findings in the deciduous dentition period to establish an early preventive program for posterior crossbite at an early stage of dental development.
Material and methods
From the files of the Department of Pedodontics, Dental Policlinic, Kranj, Slovenia, 30 children with posterior crossbite (13 boys, 17 girls; mean age, 5.5 years; range, 3.6-7.2 years) and 30 children without crossbite (17 boys, 13 girls; mean age, 5.9 years; range, 5.4-6.7 years) were randomly selected from the local kindergarten and invited to participate in this study. The research was approved by the Ethics Committee, University of Ljubljana, Medical Faculty, Ljubljana, Slovenia, and the parents were asked to give informed consent for their children to participate in the study.
Information about a subject’s nutritive and nonnutritive sucking behaviors was recorded in the parents’ interview ( Appendix ). Information regarding breast and bottle feeding, pacifier sucking, and allergies was registered in the questionnaire and further discussed by the first author (S.M.).
The durations of breast-feeding and pacifier sucking were categorized by the method described by Warren and Bishara. The duration of breast-feeding was classified into 4 categories: no breast-feeding, breast-feeding less than 6 months, breast-feeding from 6 to 12 months, and breast-feeding more than 12 months. The duration of pacifier sucking was categorized in 4 categories: the habit ceased before 12 months of age, the habit continued at 12 months but ceased by 24 months, the habit continued at 24 months but ceased by 36 months, and the habit continued at 36 months, but ceased by 48 months.
During the clinical examinations, performed by an experienced orthodontist (M.O.) and an otolaryngologist (I.H.B.), the children’s breathing, swallowing, and intraoral status were registered. The mode of breathing was determined with an instrument (Breathing Detector, MKS Elektronski sistemi, Ljubljana, Slovenia) that registers the airflow temperature through the mouth, or nose in subjects with incompetent lip seal, thus distinguishing mouth breathing from incompetent lip seal. Each child was observed in a relaxed position, and incompetent lip closure was noted ( Fig 1 ). If this was not the case, the child’s mode of breathing was registered with a special airflow device that registers the difference in the temperature of the airflow through the mouth, or the nose in those with incompetent lip seal. In open-mouth posture, the breathing detector was placed in front of the mouth, and the light sign or the light signal on the device confirmed that the airflow was coming through the mouth, thus determining improper breathing ( Fig 1 ).

To assess the swallowing pattern, we used the method suggested by Melsen et al. This was carried out while the child was swallowing saliva or small amounts of water. First, the mandibular movements and the perioral muscle contractions were observed during swallowing. Then, the examiners palpated the temporalis and masseter muscles while the child produced an unconscious swallow, since this can deviate from a swallow on command. Normal swallowing pattern was characterized by tooth contact and activity of the masseter muscles. If muscle contraction was not registered, an atypical swallowing pattern was recorded. Each child swallowed for 3 times, and the consensus opinion about swallowing pattern was accepted.
During the intraoral examination, posterior crossbite, midline deviation, and transverse buccal relationships were recorded, and alginate impressions of the maxillary and mandibular arches were obtained for both groups of children.
The otolaryngologist’s clinical examination was performed while the child was sitting on a chair in a relaxed position. The otolaryngologist examined the tympanic membrane (normal or retracted), nasal mucosa (normal or edematous), possible deviation of the nasal septum, sizes of tonsils and adenoids (small, the tonsils were covered with the arcus palatoglossus; medium, the tonsils were just above the arcus palatoglossus; large, the tonsils were narrowing the isthmus faucium), and objective nasal breathing (possible, obstructed). With the children in a relaxed position we also noted whether the lips were competent. If this was not the case, the child’s breathing was determined with the instrument that registers the difference in airflow temperature through the mouth, or nose in subjects with incompetent lip seal, thus distinguishing mouth breathing from incompetent lip seal ( Fig 1 ). The tongue position (normal or on the mouth floor), length of the frenulum linguae (normal, clinically assessed with lifting the tongue upward to contact the maxillary central incisors; short, could not contact the maxillary central incisors and was obviously short [ Fig 2 ]), motor skills of the tongue (mobility of the tongue: normal or slow) and lips (assessed during speech: in resting position: closed, slightly open, or incompetent), activity of the mentalis muscles, and lip competence (in relaxed closed mouth position: normal, no muscle activity; incompetent, contraction of mentalis muscle observed), and length of the upper lip (normal, short) were also assessed.

To evaluate the dental arches, alginate impressions were poured in hard blue stone, with the casts subsequently trimmed and articulated.
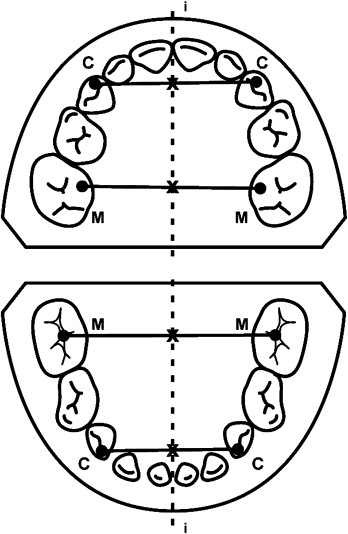
The study casts were analyzed by 1 examiner (S.M.). The relationships of the deciduous canines and second molars, anterior and posterior crossbites, and midline deviations were recorded. Measurements were obtained directly from the casts in millimeters, with calipers accurate to 0.05 mm (Mitutoyo, Tokyo, Japan). The following dental arch parameters were measured: intercanine arch widths from cusp to cusp in the both jaws, intermolar arch widths between the mesiopalatal cusps of the second deciduous molars in the maxilla, and between the central fossae of the second deciduous molars in the mandible ( Fig 3 ), as described by Thilander and Lennartsson.
Statistical analysis
Data from the questionnaires, otolaryngologic examinations, and dental arch examinations were analyzed with the SPSS for Windows statistical program (version 15.0, SPSS, Chicago, Ill). The data from the crossbite and noncrossbite groups of children were compared regarding various parameters with univariate analysis of variance (ANOVA), independent samples t test, and Mann-Whitney test. The chi-square test was used to compare categorical (attributive) variables between the 2 groups. The Spearman correlation coefficient was used to confirm the relationship between pacifier sucking times and dental arch widths. Statistical significance was predetermined at P <0.05.
Receiver operating characteristic (ROC) curve was used to evaluate the influence of pacifier sucking time in months on the development of posterior crossbite, as determined by the area under the curve.
Results
Comparisons of various parameters from the questionnaire regarding nutritive and nonnutritive sucking behaviors between the posterior crossbite and the noncrossbite groups of children showed no statistically significant differences for the durations of breast-feeding and bottle feeding ( Table I ). However, a statistically significant difference was found between the 2 groups in the duration of pacifier habit ( P = 0.001, Table I ).
| Sucking habit | Crossbite group Mean (SD) | Control group Mean (SD) | P value |
|---|---|---|---|
| Breast-feeding | 6.65 (5.29) | 8.96 (6.30) | 0.162 |
| Bottle feeding | 19.70 (11.91) | 14.64 (13.30) | 0.092 |
| Pacifier | 27.35 (14.04) | 16.36 (13.33) | 0.001 |
The otolaryngologic findings ( Table II ) showed no statistically significant differences between the 2 groups regarding the tympanic membrane and nasal mucosa, shape of the nasal septum, nasal patency, sizes of tonsils and adenoids, objective nasal mode of breathing, tongue position, motor skills of tongue and lips, resting position of the lips, activity of the mentalis muscles and lip competence, length of the upper lip, and atypical swallowing pattern.
| Parameter | Crossbite group | Noncrossbite group | P value |
|---|---|---|---|
| Presence of an allergy | 5 (13.5%) | 3 (12.5%) | 0.91 |
| Short length of the frenulum linguae | 10 (37%) | 0 (0%) | <0.001 |
| Retracted tympanic membrane | 17 (61%) | 16 (59%) | 0.10 |
| Edematous nasal mucosa | 19 (68%) | 20 (74%) | 0.62 |
| Deviation of the nasal septum | 1 (4%) | 4 (16%) | 0.13 |
| Large tonsils and adenoids | 12 (43%) | 13 (48%) | 0.70 |
| Impaired nasal breathing | 5 (18%) | 6 (27%) | 0.054 |
| Nasal infection | 4 (14%) | 7 (32%) | 0.054 |
| Mouth floor tongue position | 15 (56%) | 17 (65%) | 0.53 |
| Normal motor skills of tongue | 25 (93%) | 27 (100%) | 0.15 |
| Normal motor skills of lips | 26 (96%) | 24 (89%) | 0.30 |
| Slightly open resting position of the lips (lip competence) | 14 (52%) | 16 (62%) | 0.48 |
| Active mentalis muscles | 17 (63%) | 12 (46%) | 0.22 |
| Short length of the upper lip | 20 (74%) | 22 (81%) | 0.52 |
| Atypical swallowing pattern | 6 (22%) | 2 (8%) | 0.14 |
The only functional sign that was statistically significantly different between the posterior crossbite and the noncrossbite groups was the length of the frenulum linguae (only crossbite patients had a short frenulum linguae; P <0.001, Table II ).
Regarding dental arch parameters ( Table III ), in the crossbite group, the maxillary arch was smaller than expected with regard to age, sex, and size of the children in the intercanine ( P =0.002) and intermolar ( P <0.001) regions, and the mandibular arch was larger than expected with regard to age, sex, and size of the children ( P = 0.001 for intercanine and P = 0.002 for intermolar arch widths). No children with the pacifier habit had digit habits.
| Measurement | Crossbite group Mean (SD) | Noncrossbite group Mean (SD) | P value ∗ | |
|---|---|---|---|---|
| Maxillary arch widths (mm) | Intercanine | 26.69 (2.08) | 29.14 (1.79) | 0.002 |
| Intermolar | 31.73 (2.27) | 34.62 (1.88) | <0.001 | |
| Mandibular arch widths (mm) | Intercanine | 23.75 (1.36) | 23.26 (1.43) | 0.001 |
| Intermolar | 34.51 (1.90) | 34.06 (1.57) | 0.002 | |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


