▪
WHAT IS PLATELET-RICH AND PLATELET-POOR PLASMA?
The concept of platelet-rich plasma (PRP) or platelet gel represents an autologous centrifuged blood sample composed of intrinsic growth factors intended for regeneration of soft and hard tissue ( Figure 30-1 ). It consists of a concentration of platelets and the seven fundamental protein growth factors evidenced to be actively secreted by platelets to initiate all wound healing processes. Collectively, these growth factors include the three isomers of platelet-derived growth factors (PDGFs) (PDGF-aa, PDGF-bb, and PDGF-ab), two of the numerous transforming growth factors (TGFs) (TGF-β 1 and TGF-β 2 ), vascular endothelial growth factor, and epithelial growth factor. It has been scientifically determined that all of the growth factors have been documented to derive from platelets. Specific growth factors associated with PRP initiate soft tissue healing and bone regeneration. The premise of PRP is based on methods to concentrate autologous platelets for the addition to surgical wounds or grafts, which require the influence of growth factors to support and accelerate healing. The PRP provides approximately a 2.16 increase in the maturation rate and considerably greater density of the final bone-graft product. In addition, soft tissue healing is also substantially improved through the employment of PRP via increasing collagen content, promotion of angiogenesis, and increasing early wound strength. Finally, growth factors found in PRP regulate key cellular processes, such as mitogenesis, chemotaxis, and cell differentiation. PRP simulates the last step of the coagulation cascade, which leads to the formation of a fibrin clot. As a result, the fibrin clot consolidates and adheres to the site of application. The healing characteristics and hemostatic properties of PRP enable it to support tissues and structures in desired configurations. In addition, many other inherent benefits derived from PRP are: (1) biocompatible and biodegradable components prevent the PRP from initiating foreign body reactions, tissue necrosis, or extensive fibrosis; (2) the fibrin clot is absorbed within a few weeks of the wound healing process; (3) PRP has been used in innumerable transplant procedures to include the field of dentistry; and (4) PRP can be attributed to the increased healing of wounds and surgical sites, which is correlated with less postsurgical pain. More importantly, PRP has a measure of safety that relates to its autologous derivation and appears to decrease the risk of transmissible diseases (HIV, Hepatitis B, C, and D, etc.). Finally, some of the other benefits of PRP include its degree of safety, nontoxicity to tissue, ease of preparedness, cost-effectiveness, and promotion of local tissue growth and repair.

Autologous platelet gel is created from the processing and treatment of PRP and possesses two to four times the concentration of platelets. As a comparison, an individual’s normal platelet range is between 150,000 to 350,000 mm . However, PRP or platelet gel concentrate consists of 1,000,000 platelets per cubic millimeter. Therefore, one would conjecture that the capacity for initiating growth and repair in the form of a platelet gel far exceeds the normal platelet capacity. In addition, a natural blood clot contains 95% red blood cells (RBCs), 5% platelets, less than 1% white blood cells, and numerous amounts of fibrin strands. A PRP blood clot contains 4% RBCs, 95% platelets, and 1% white blood cells.
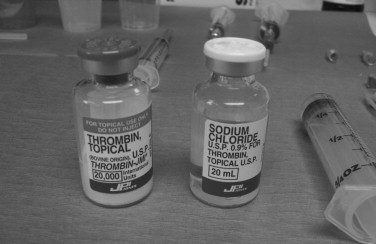
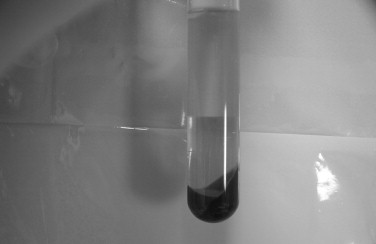
Since 1990 medical science has identified several components in blood that facilitate the natural healing process. The relative use of PRP-like components was initially proposed in 1970 and was identified as fibrin glue. Fibrin glue was formed by active polymerization of fibrinogen with thrombin and calcium. It was originally prepared by using donor plasma; however, because of the low concentration in plasma, the stability and quality of the fibrin glue were low. The use of cryoprecipitate-based fibrin glue yielded far better results. However, in more recent times, the development of fibrin glue has evolved to a more complex biologic material, essential to tissue and bone regeneration. The autologous concentration of PRP requires a centrifugation process for differentiation of cellular components, which is mainly designed to allow the delineation of PRP and platelet-poor plasma (PPP) ( Figure 30-2 ). When PRP is combined with thrombin and calcium chloride, platelet gel is created ( Figure 30-3 ). This product is a rich source of growth factors and has been found to be effective in accelerating significant tissue repair and regeneration. Once again the process is aimed at eliciting the beneficial effects related to the growth factors obtained from PRP. Also as a result of the platelets releasing specific growth factors, the processes of osteogenesis, angiogenesis, and wound healing are activated.
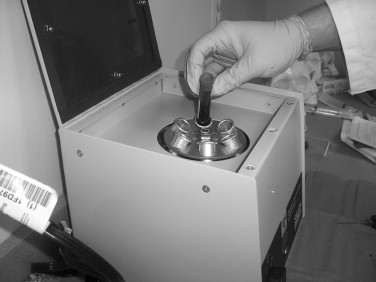
Autologous PPP was first described in 1972. PPP is produced by separating plasma from RBCs using a high spin to pellet platelets with the RBCs ( Figure 30-4 ). Coincidentally, this represents the starting point for production of most blood components. The rationale for the separation of platelets is desirable because they provide an additional source of foreign antigens and microaggregation, which can cause fusion reactions. PPP is acellular in composition and contains fibrinogen, which can be used for soft tissue hemostatic management and wound healing. The intrinsic growth factors are minimal, and PPP’s capacity to initiate regenerative influence is lessened. Upon the completion of the centrifugation process of whole blood to produce PRP, PPP is the least dense layer and comprises 45% of the sample obtained.
It is important to note that platelet counts and growth factor content are usually dependent upon the method or technique used to obtain the PRP. In addition, the donor’s biologic condition may be the determining factor in the composition of PRP and its observed biologic effects. Acknowledging the fact that there are many methods employed to obtain PRP, the ending results seem to conclude with three resultants: PRP, PPP, and RBCs.
▪
WHAT ARE THE BENEFITS OF PRP?
- 1.
“Jump-starts” osteogenesis: By releasing growth factors at a local site, osteoblasts can be enticed to move across a greater distance by creating a scaffold system (fibrin) that will assist in their movement. Because the growth factors are added to the graft at the time of graft replacement (in the platelet gel) instead of being released by the coupled process of resorption and the obligatory replacement, there is approximately a 2-month acceleration in the maturation of the bone graft.
- 2.
Early consolidation of the graft: The increased amount of PDGF in the graft initiates osteocompetent cell activity at an enhanced molecular rate. Many other growth factors assist in graft success and bone regeneration, such as bone morphogenic protein (BMP). The primary response of osteoblasts is activated by BMP. The BMP provided by PRP with the addition of that provided by the initial resorption of bone occurring during the osteophyllic phase (lasts approximately a month) results in earlier maturation of the grafted bone.
- 3.
Speeds of mineralization: Because mineralization of a graft site is a coupled phenomenon, osteogenesis must proceed in such a way that activation and bone formation is greater than resorption. Mineralization of the collagen matrix occurs more rapidly because PDGF is added right from the start in the mineralized bone segment of the graft, instead of released from collagen. As a result, the use of PRP has shown to improve the rate of bone formation by 1.62 to 2.18 times the normal bone healing time.
- 4.
Improves trabecular bone density: It has been reported in the literature that there has been a 15% to 30% improvement in trabecular bone density when PRP factors are added to the graft site.
- 5.
Eliminates the risk of infection or disease: PRP is an autologous process and obviates the concern for disease transmission and allergenicity. More patients are eligible for the procedures because the strict criteria for blood bank donations do not have to be met.
▪
WHAT ARE THE BENEFITS OF PRP?
- 1.
“Jump-starts” osteogenesis: By releasing growth factors at a local site, osteoblasts can be enticed to move across a greater distance by creating a scaffold system (fibrin) that will assist in their movement. Because the growth factors are added to the graft at the time of graft replacement (in the platelet gel) instead of being released by the coupled process of resorption and the obligatory replacement, there is approximately a 2-month acceleration in the maturation of the bone graft.
- 2.
Early consolidation of the graft: The increased amount of PDGF in the graft initiates osteocompetent cell activity at an enhanced molecular rate. Many other growth factors assist in graft success and bone regeneration, such as bone morphogenic protein (BMP). The primary response of osteoblasts is activated by BMP. The BMP provided by PRP with the addition of that provided by the initial resorption of bone occurring during the osteophyllic phase (lasts approximately a month) results in earlier maturation of the grafted bone.
- 3.
Speeds of mineralization: Because mineralization of a graft site is a coupled phenomenon, osteogenesis must proceed in such a way that activation and bone formation is greater than resorption. Mineralization of the collagen matrix occurs more rapidly because PDGF is added right from the start in the mineralized bone segment of the graft, instead of released from collagen. As a result, the use of PRP has shown to improve the rate of bone formation by 1.62 to 2.18 times the normal bone healing time.
- 4.
Improves trabecular bone density: It has been reported in the literature that there has been a 15% to 30% improvement in trabecular bone density when PRP factors are added to the graft site.
- 5.
Eliminates the risk of infection or disease: PRP is an autologous process and obviates the concern for disease transmission and allergenicity. More patients are eligible for the procedures because the strict criteria for blood bank donations do not have to be met.
▪
WHAT IS THE ROLE OF PRP IN BONE REGENERATION?
Weibrich et al. revealed that platelet counts and growth factor contents are highly dependent on the technique of processing PRP. Also, the biologic condition of the donor may influence the efficacy of PRP and its biologic effects. To understand how PRP affects bone regeneration, the sequence of regeneration should be made clear.
Platelets are composed of cytoplasmic fragments of megakaryocytes that circulate in the blood. As a result, platelets are responsible for hemostasis and the initiation of regeneration of tissue from trauma episodes. The most integral biologic unit of PRP is the presence of platelets and the platelet’s composition to produce growth factors. Sanchez et al. indicated that the properties of PRP were highly dependent upon the production and release of growth and differentiation factors during platelet activation. The factors assume an integral role in the regulation and stimulation of the wound healing process and the cellular processes of mitogenesis, chemotaxis, and metabolism.
Tsay et al. conveyed that chemotaxis of osteoblast precursors to the site of bone regeneration is directed by specific structural proteins, such as collagen and/or osteocalcin, and growth factors, such as PDGF and TGF-β. This process is then followed by osteoblast proliferation and aggregation. PDGF, TGF-β, fibroblastic growth factor (FGF), insulin-like growth factor (IGF)-I, and IGF-II have all been proven to illustrate stimulation in osteoblastic growth. Osteoblast differentiation is controlled by growth factors, and this interaction allows the formation of mature bone cells from the primitive osteoblastic stage. The growth factors most responsible for facilitating the maturation stage are IGF-I and BMPs.
The previously mentioned growth factors assume an important role in mediating normal bone healing and regeneration. The growth factors inherent to platelets help facilitate regenerative changes in many biologic circumstances. Platelets are responsible for initiation of regeneration of tissue that has been traumatized. During the reparative process, platelets become entrapped in a fibrin clot and degranulate, releasing two primary growth factors: PDGF and TGF-β. PDGF binds to endothelial cells to produce capillary ingrowth, and TGF-β attaches to osteoblasts and stem cells to initiate mitosis and stimulate osteoid production. As a result, growth factors contained and released from PRP should enhance and accelerate soft tissue healing and the process of regenerating bone, thereby emphasizing the importance of the common platelet function in PRP to generate growth factors to mediate healing at a specified site.
According to Tsay et al., growth factors are activated at the appropriate temporal sequence and spatial distribution. As a result, the aforementioned concepts profoundly affect the influence of growth factors related to tissue regeneration.
The function and action of the growth factors are very complex. Each individual growth factor may have a different effect on the same tissues and different responses that are dependent on the specific tissues targeted. Growth factors also interact with one another, consequently forming a cascade of different signal proteins with multiple pathways, which inevitably progress to gene activation and protein production. This enables PRP to differentiate its own actions from recombinant growth factors that are directed toward a single regenerative pathway.
Many bone-grafting procedures concomitantly combine the graft with PRP to attempt to ensure proliferation, vascularization, and incorporation ( Figure 30-5
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


