HISTORIC PERSPECTIVE
The successful management of cranio-maxillofacial injuries, as with any traumatic injury, begins with the immediate application of the principles of advanced trauma life support (ATLS). Trauma care, as we currently know it, has evolved from the close association of surgery and casualty management in times of war. Many key concepts, including pre-hospital care, triage, and transport; volume resuscitation; wound management; and critical care, were later refined based on the experience gained during military conflict.
Many of our patients might not have otherwise survived their injuries had it not been for the standards set forth by the American College of Surgeons (ATLS) and for the work of trauma care pioneers like R. Adams Cowley at the University of Maryland. The work of Cowley was vital to the implementation of modern trauma care and the design of the modern trauma unit. His vision led to the development of the first clinical shock trauma unit in the nation ( Figure 1-1 ). He was one of the first to recognize the importance of pre-hospital care in its association with the trauma center, and his “Golden Hour” theory emerged based on the importance of speed and skill in resuscitation and operative intervention. Cowley also developed the first statewide air medical system to ensure rapid transport of critically ill or injured patients to the trauma center ( Figure 1-2 ). Maryland instituted the first statewide emergency medical services (EMS) system, and it, like the Shock Trauma Center, has become a model worldwide.

INTRODUCTION
Death as a result of trauma follows a tri-modal distribution with the first peak occurring at the time of injury, within seconds to minutes. This is typically the result of brain, brain stem, spinal cord, heart, or great vessel injury. Only prevention can effectively decrease death caused by injury in the first peak. The second peak occurs within minutes to hours of injury. ATLS was implemented with this critical period in mind. Fatal or life-threatening injuries commonly encountered in this group include subdural/epidural hematomas, hemothorax/pneumothorax, pelvic fractures, and spleen/liver lacerations. Rapid transport, assessment, and intervention may greatly improve survival in this group. Lastly, the third peak takes place days to weeks after the initial injury. Commonly, mortality in this group is due to sepsis and multi-system organ failure. At this point, outcome is affected by any and all who have provided care prior to this stage.
ASSESSMENT
PRIMARY SURVEY
The initial assessment, also known as the primary survey, calls for immediate identification and management of all life-threatening issues. One must assume that:
- •
There are multiple injuries
- •
The physiologic state of the patient is impaired
- •
The condition of the patient might worsen rapidly
Treatment priorities are based on exam findings, vital signs, and known events surrounding the injury. It is also important to understand that the patient’s most obvious injury might not be his or her most critical injury, and a patient with critical injuries to several different organ systems often presents conflicting priorities in management. Attention is initially directed at the resuscitation of vital functions and treating immediately life-threatening problems following a rapid, yet accurate, initial survey. This survey should take no longer than 5 to 10 minutes and includes:
- •
A—Airway
- •
B—Breathing
- •
C—Circulation
- •
D—Disability
- •
E—Exposure
A more detailed secondary head-to-toe assessment will be performed eventually, followed by the delivery of definitive care for all patient injuries.
AIRWAY
Since the loss of airway kills faster than the inability to breathe, the commonality between all forms of formal life support training is the early establishment of a patent airway. In the injured patient, this comes with the additional task of cervical spine stabilization. Supplemental oxygen should be placed immediately. Inspection of the airway includes a rapid and organized exam of the face, mandible, larynx, and trachea. Special care must be taken to look for foreign bodies and compromising facial fractures or soft tissue injuries. Dependable oxygenation and ventilation must be established while protecting the cervical spine. A careful chin lift, with special attention to the cervical spine, or a jaw thrust is advisable to achieve this task. In the conscious patient, a nasopharyngeal airway generally proves acceptable. Oral airways can evoke a gag response and are generally best left to the unconscious patient.
Verbally communicative patients are not usually at immediate risk of airway loss, although repeated assessments of the patient and his or her airway status must be undertaken because airway loss can be both progressive and recurrent. In unconscious patients or those who present obtunded (from alcohol or drug use) or with severe head injury (Glasgow Coma Scale [GCS] <8), a definitive airway should be placed as soon as possible. Severe thoracic injury can also impair ventilatory effort requiring assisted ventilation. In doing so, one must assume a cervical injury; therefore, appropriate intubation precautions must be taken. Manual in-line cervical immobilization must be maintained for the duration of the intubation, until the airway is secure and a cervical spine collar can be placed.
Maxillofacial trauma presents unique challenges to airway management. The presence of foreign bodies and blood in the airway along with unstable facial fractures can make both bag-mask ventilation and direct laryngoscopy especially difficult. The multiply fractured mandible, sometimes referred to as a “flail mandible,” can result in the alteration of normal support for the muscles of the tongue and hypopharynx or expanding hematoma of the floor of mouth or neck ( Figure 1-3 ). Combative patients who refuse to lay supine may be indicating their inability to manage their secretions or their airway when in the recumbent position.

Laryngeal trauma is a rare cause of airway obstruction. This can be particularly difficult to manage because a conventional cricothyroidotomy is not the procedure of choice to secure an airway in this situation, although it may prove necessary in the end. The talking patient provides reassurance of a patent airway, although continued reassessment is necessary. Hoarseness and subcutaneous cervical emphysema should alert one to the possibility of laryngeal fracture, and a palpable fracture confirms the diagnosis. CT scan and endoscopic evaluation can be of value when examination is made difficult by edema or body habitus. Audible breathing, stridor, and absence of breathing signify that obstruction has already occurred and that definitive steps to secure the airway must be taken.
The immediate placement of supplemental oxygen and monitoring with pulse oximetry is critical. Every patient should be rapidly assessed for airway patency and adequacy of ventilation. Once the need to intervene has been determined, the next step is to ascertain which technique and what level of intervention will best suit the patient.
Airway maintenance techniques provide support for the airway to assist the patient in maintaining ventilation or to act as a bridging technique to a definitive airway. The following maneuvers can be applied and modified as the situation mandates:
- •
Chin lift
- •
Jaw thrust
- •
Oropharyngeal airway
- •
Nasopharyngeal airway
- •
Laryngeal mask airway
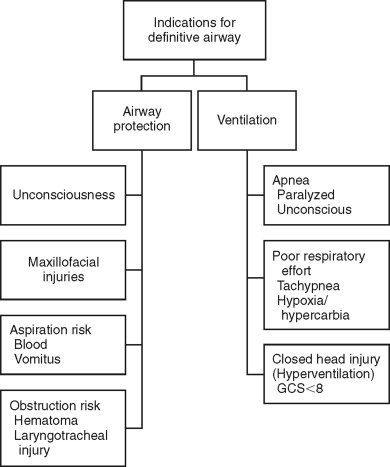
The definitive airway requires that a tube be inserted into the trachea with the cuff inflated to guard against airway obstruction and aspiration in order to provide both supplemental oxygen and assisted ventilation. Definitive airways fall into two main categories: non-surgical and surgical. The decision to provide a definitive airway is based on several criteria observed in the rapid assessment period ( Figure 1-4 ).
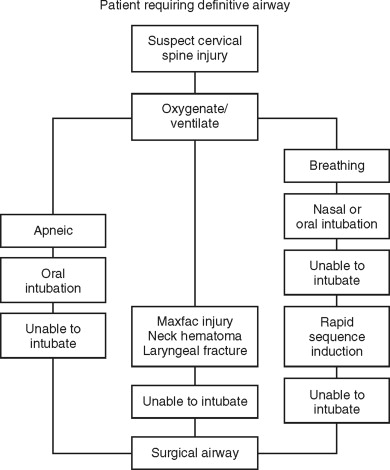
If the decision is made to provide a definitive non-surgical airway, a two-person intubation technique is required: one to provide in-line stabilization of the C-spine, and the other to perform the orotracheal or nasotracheal intubation. Blind nasotracheal intubation is a useful technique when the C-spine is compromised; however, the patient must be spontaneously breathing for this technique to be effective. In addition, when upper or midface and cranial base fractures are suspected, both nasotracheal and nasogastric intubation should be avoided. If the patient is apneic, orotracheal intubation is indicated. Cricoid pressure is helpful to occlude the esophagus and prevent aspiration; in addition, it can provide improved visualization of the vocal cords in the more anteriorly positioned airway. In patients with difficult airways, endotracheal intubation can be further assisted with fiberoptic endoscopic guidance or video laryngoscopy.
Depending on the patient’s neurologic status, pharmacologic agents may or may not be required to facilitate intubation. If pharmacologic assistance is required for intubation, a rapid sequence induction is advisable:
- •
Pre-oxygenate
- •
Administer cricoid pressure
- •
Administer 1-2 mg/kg succinylcholine, IV
- •
Intubate
- •
Inflate cuff and confirm tube placement
- •
Release cricoid pressure
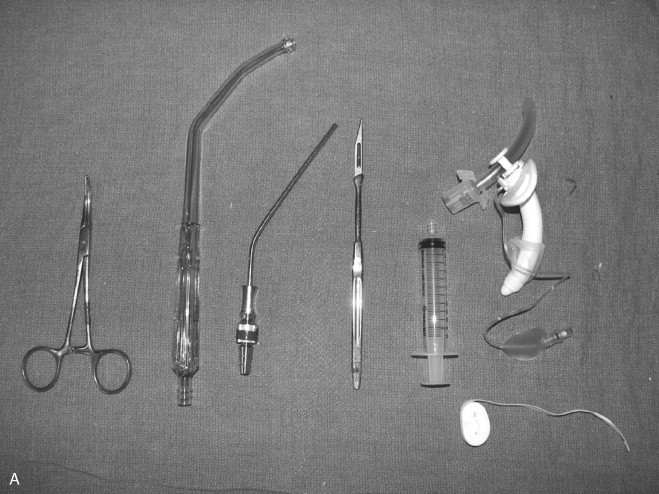
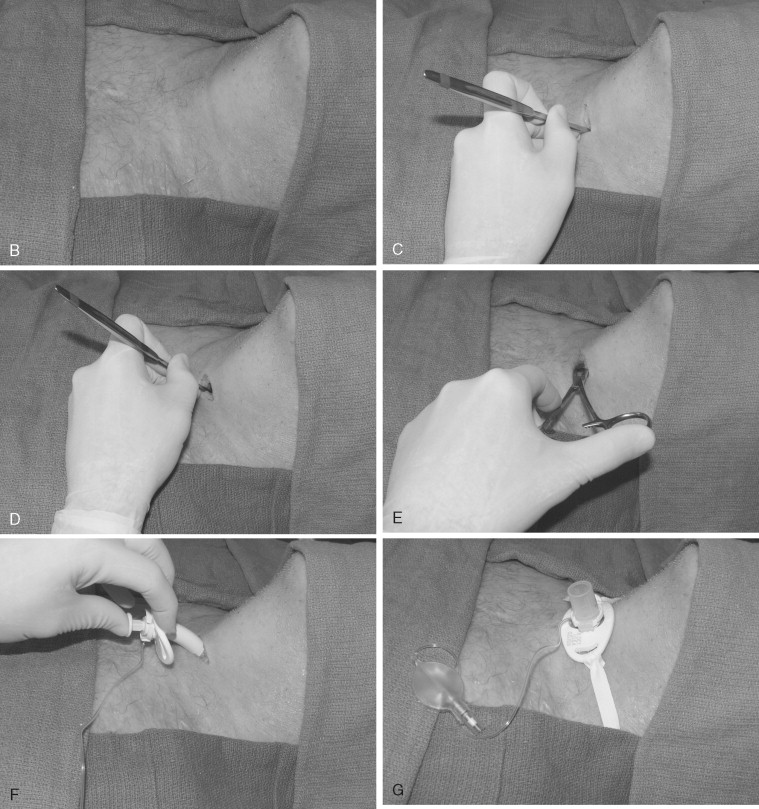
In the event that intubation is unsuccessful, one must be prepared to perform a surgical airway ( Figure 1-5 ). Glottic edema, oropharyngeal hemorrhage, foreign bodies, and laryngeal fractures can all impede the passage of the endotracheal tube through the glottic inlet. Placement of needle cricothyroidotomy can be a useful technique in an emergency situation; however, it is intended for short-term oxygenation only, since it is not an adequate means of gas exchange. The surgical cricothyroidotomy is the preferred means of establishing an emergent airway. It is easier to perform urgently compared with tracheotomy. The cricothyroidotomy is associated with less bleeding, has more readily identifiable surgical landmarks, and is a quicker procedure ( Figure 1-6 ). Needle cricothyroidotomy with jet insufflation can be used as a bridging procedure to improve oxygenation and allow the surgical procedure to be performed in a more orderly fashion.
In the pediatric population, either needle cricothyroidotomy or tracheotomy is the emergency surgical airway of choice, since surgical cricothyroidotomy carries significant risk to the glottis and may result in subglottic stenosis after decannulation.
Key Points
- •
Be prepared to secure an airway in all injured patients.
- •
Treat all patients as though they have a cervical spine injury.
- •
Continuously reassess airway patency; when in doubt, secure the airway.
- •
Avoid prolonged apnea; be prepared to secure a surgical airway.
BREATHING
Once the airway has been found to be patent, the chest and abdomen must be efficiently inspected to ensure adequate respiratory mechanics. The lungs, chest wall, and diaphragm all contribute to normal gas exchange. Injuries to any one of these structures can severely impair the body’s ability to ventilate.
The chest and abdomen must be adequately exposed to allow visual inspection. Obvious open chest wounds should be dealt with immediately. Contusions and hematomas may be an indication of more severe underlying injury. Paradoxical chest wall movements and abdominal breathing may alert the caregiver to chest wall or spinal cord injuries that compromise adequate ventilation. The chest should be auscultated to ensure adequate, bilateral gas flow. Percussion, anteriorly and posteriorly, might reveal air or fluid in the chest. All structures of the chest wall must be palpated, including the sternum, clavicles, and ribs. Palpation might demonstrate tracheal deviation or chest wall crepitus, indicating pneumothorax or rib fractures.
Acute ventilatory compromise can occur with tension pneumothorax, massive hemothorax, flail chest, and open pneumothorax. Urgent treatment is required to avoid significant respiratory compromise. In the tachycardic/tachypneic patient who continues to decline following intubation, suspect a thoracic injury that can be worsened by aggressive ventilation.
Key Points
- •
Ventilation problems in the face of a successful intubation may be due to thoracic trauma.
- •
Adequate exposure and examination of the chest and abdomen may hold the key to the diagnosis of ventilatory problems.
CIRCULATION
Hemorrhage resulting from injury is the most common cause of post-injury deaths. Although tachycardia is often the first sign of hypovolemia, it can be caused acutely by pain and anxiety, among other things. Hypotension, on the other hand, should be considered to be due to hypovolemia/hemorrhage in the injured patient until proven otherwise. As with the assessment of the preceding two clinical elements (airway and breathing), rapid and efficient evaluation of the patient’s hemodynamic status is critical in the injured patient. External bleeding is controlled by direct pressure on wounds while the likelihood of hemorrhage into the chest, abdomen, or pelvis is quickly evaluated. Two large-bore peripheral intravenous catheters should be placed at the time of the primary survey to allow resuscitation. If peripheral upper extremity access is inadequate, alternative routes should be sought, including central venous lines in the groin or cutdown of the greater saphenous vein. In children, intraosseous infusion is used as an alternative route if peripheral access cannot be established. Fluid resuscitation begins with a 1000-mL bolus of crystalloid solution for an adult or 20 mL/kg for a child. External hemorrhage should be readily identifiable and quickly controlled. Key markers of hemodynamic status include the patient’s level of consciousness, heart rate, and skin color and should be monitored continuously to measure the patient’s response to therapy.
Extremes of age also carry significant implications in the evaluation and management of hemorrhage. Children have substantial reserve and are able to compensate for shock, even in the face of severe volume depletion. Significant tachycardia of up to 180 beats/minute may be seen. When decompensation finally occurs, it is sudden and often difficult to recover. The geriatric population, on the other hand, has a limited ability to compensate for significant hemorrhage as a result of decreased sensitivity to catecholamines and consequently a blunted tachycardic response. This can be further affected by medications such as beta-adrenergic blockers and calcium channel blockers as well as pacemakers, all of which are commonly seen in this age group. In addition to age, body temperature, pregnancy, athletic conditioning, and medications can greatly influence the response to shock.
Shock is defined as the presence of inadequate organ perfusion and tissue hypoxia resulting in end organ damage. The successful management of shock in the injured patient depends on recognition and identification of the likely cause. Although hemorrhagic shock is most commonly associated with the trauma patient, cardiogenic, neurologic, and septic shock also occur. Volume resuscitation should be the initial intervention, and once the cause of shock has been recognized, necessary adjustments to treatment should be instituted immediately.
Patients often present in shock or with impending shock, and reliance on decreased systolic blood pressure to make the diagnosis leads to delayed recognition and treatment. Earlier indicators of shock include mottled skin and delayed capillary refill; in some cases, tachycardia is the earliest recognizable sign. In the injured state, endogenous catecholamine release results in vasoconstriction of the cutaneous and visceral circulation in favor of the central neurologic, cardiac, and renal systems. Cardiovascular stimulation results in tachycardia, elevated diastolic blood pressure, and a decreased pulse pressure.
Shock in the traumatized patient is usually recognized as either hemorrhagic or non-hemorrhagic. Short of obvious hemorrhagic shock, the etiology can sometimes only be determined after a careful history and examination. Since most shock states will respond briefly to volume resuscitation, insight into the cause may be gained after carefully observing the response to the initial intervention. Additional data can be gathered with invasive monitoring (central venous or pulmonary artery catheters), diagnostic maneuvers (diagnostic peritoneal lavage), and selected imaging studies (computed tomography, ultrasound, plain films).
- •
Hemorrhagic
- •
Non-hemorrhagic
-
Cardiogenic
-
Neurogenic
-
Septic
Hemorrhagic shock classification is based on the percentage of the total blood volume lost acutely, and the determination of which class a patient falls into is made largely based on clinical signs. Treatment, however, should not be based solely on the class of shock, but on the patient’s response to resuscitative efforts ( Table 1-1 ).
- •
Class I hemorrhage is <15% blood loss, and this is roughly the equivalent of donating a unit of blood. There are no changes in blood pressure or heart rate. For healthy patients, the blood volume equilibrates within 24 hours.
- •
Class II hemorrhage is 15-30% blood loss and can lead to tachycardia, tachypnea, and an increase in diastolic blood pressure. This results in a narrowed pulse pressure and is caused by a surge in catecholamines. Urine output may be mildly affected and mental status is usually stable. Resuscitation with crystalloid is recommended.
- •
Class III hemorrhage is 30-40% blood loss. This results in marked tachycardia, tachypnea, decreased pulse pressure, and hypotension. Signs of hypoperfusion will also be evident, including delayed capillary refill, decreased urine output, and mental status changes. Transfusion is required in this patient group.
- •
Class IV hemorrhage is loss of >40% blood volume. This is a pre-terminal event. Severe hypotension and tachycardia are accompanied by a narrow pulse pressure. Mental status changes are accompanied by cool pale skin. Urine output is negligible. Emergency surgery to identify and control hemorrhage along with rapid transfusion of multiple units of blood is critical.
| Class | I | II | III | IV |
|---|---|---|---|---|
| Character of hemorrhage | Donated one unit of blood | Uncomplicated | Complicated | Pre-terminal |
| Volumetric blood loss | Up to 750 mL | 750-1500 mL | 1500-2000 mL | >2000 mL |
| % blood loss | <15% | 15-30% | 30-40% | >40% |
| Heart rate | — | ↑ | ↑↑ | ↑↑ |
| Respirations | — | ↑ | ↑↑ | ↑↑ |
| Systolic blood pressure | — | — | ↓ | ↓↓ |
| Pulse pressure | — | ↓ | ↓↓ | ↓↓ * |
| Urine output | — | — | ↓ | ↓↓ |
| Treatment required | None or crystalloid † | Crystalloid resuscitation † | Crystalloid resuscitation † or blood replacement |
|
* Diastolic BP may be unobtainable.
† “3 : 1 rule”: for every 100 mL of blood lost, 300 mL of crystalloid is required for resuscitation.
Significant hemorrhage and hypovolemia result in decreased urinary output as blood flow is diverted from the kidneys in favor of the heart and brain. Placement of a urinary catheter and observation of urine output is critical to monitor a patient’s response to volume replacement therapy. Urine output of 0.5 mL/kg/h is the minimum tolerated, and volume replacement with crystalloid or blood should be initiated to maintain at least this level of urinary output. When pelvic fractures or groin injury have been noted on the primary or secondary survey, a urinary catheter should not be placed until urethral injury has been excluded.
Mental status changes in the trauma patient do not occur until the latter stages of shock. Cerebral autoregulation preserves blood flow to the brain, and hypoperfusion does not occur until the systolic blood pressure falls to 55-60 mm Hg. This may manifest as agitation, confusion, and anxiety. Mental status changes may also be indicative of head injury, spinal trauma, intoxication, hypoxia, or electrolyte disturbance in the acutely injured patient.
Life-threatening hemorrhage can occur as a result of maxillofacial injuries. In one study, approximately 1% of maxillofacial trauma patients suffered from life-threatening hemorrhage as a result of their injuries. Blunt force trauma was the mechanism of injury in the majority of cases and resulted in high-level LeFort injuries. An average of 7 L of crystalloid was required in the resuscitation phase of treatment, and all patients were subsequently treated with interventional embolization. Similarly, neck injuries can result in vascular compromise, and treatment algorithms have been designed to manage them primarily with either surgery or angiographic means.
The treatment of exsanguinating hemorrhagic shock is instituted initially with crystalloid and type O-negative blood. Type-specific blood can usually be provided within 10 minutes and is Rh and ABO compatible. Fully crossmatched blood is favored; however, this process takes an hour in most institutions. This avoids exposure and sensitization to other antibodies and is preferable in the hemodynamically stable patient.
Key Points
- •
Obtain adequate vascular access immediately.
- •
In the traumatized patient, assume shock is hemorrhagic until proven otherwise.
- •
Initiate treatment before the appearance of hypotension.
DISABILITY (NEUROLOGIC STATUS)
After resuscitation has been instituted to treat life-threatening injuries noted in the ABCs, what follows is a rapid neurologic assessment to determine the presence significant injury. A commonly used mnemonic is AVPU:
- •
A—Alert
- •
V—responds to a Verbal stimulus
- •
P—responds to a Painful stimulus
- •
U—Unresponsive
Complete neurologic evaluation is best performed during the secondary survey, since it is less likely to be accurate until the patient has been hemodynamically stabilized. In lieu of “AVPU,” level of consciousness can be measured by the GCS score as well as pupillary response. Movement of extremities is also evaluated and recorded. The GCS assesses three parameters: the response of the eyes, the motor response, and the verbal response of the patient. Sedatives and paralytic agents required for intubation can interfere with GCS scoring and ongoing neurologic reassessment. When the patient is intubated but responsive to the remainder of the GCS examination, the verbal component of the GCS cannot be assessed; this is simply denoted by adding a “T” to the minimum verbal score, indicating intubation (a neurologically normal patient who is intubated is GCS 11T). (See Table 1-2 .)
| Assessment | Score |
|---|---|
| EYE OPENING | |
| Spontaneous | 4 |
| To speech | 3 |
| To pain | 2 |
| None | 1 |
| MOTOR RESPONSE | |
| Follows commands | 6 |
| Localizes pain | 5 |
| Withdraws to pain | 4 |
| Abnormal flexion (decorticate) | 3 |
| Extension (decerebrate) | 2 |
| Flaccidity | 1 |
| VERBAL RESPONSE | |
| Oriented | 5 |
| Confused | 4 |
| Inappropriate words | 3 |
| Incomprehensible sounds | 2 |
| None | 1 |
Key Points
- •
Neurologic deterioration can be sudden and rapid.
- •
Frequently reevaluate neurologic status.
EXPOSURE/ENVIRONMENTAL CONTROL
The last step in the primary survey is to completely expose the patient and perform a quick head-to-toe examination, which might reveal injuries to the back, perineum, or other areas that are not easily seen in the supine, clothed position. Cutting the clothing off to accomplish this is acceptable. Temperature should be recorded as early as possible in the examination, and careful attention must also be given to maintaining the patient’s body temperature once his or her clothes have been removed. This is accomplished with warm blankets, warming lights, and warmed intravenous fluids. A more thorough head-to-toe examination will be performed in the secondary survey.
Key Points
- •
Identify obvious sites of internal and external hemorrhage (bleeding, fracture, ecchymosis).
- •
Keep the patient warm.
SECONDARY SURVEY
The secondary survey begins after the primary survey is complete and the patient has been stabilized. This survey is a systematic head-to-toe and front-to-back examination and includes a more detailed history. Continuous reassessment of the ABCDEs is carried out during this time.
Consideration should be given to urinary catheter placement, gastric tube placement, additional intravenous lines, arterial monitoring, and central venous access, if they are not in place already.
HISTORY
A thorough history should be obtained from the patient if possible, and if not, the patient, the family, or prehospital personnel. At a minimum, the following information is desirable:
- •
A llergies
- •
M edications
- •
P ast illnesses/pregnancy/operations
- •
L ast meal
- •
E vents/environment related to the injury
MAXILLOFACIAL INJURIES
Maxillofacial injuries occur with some frequency in the acutely traumatized patient. They present several challenges to the emergency department physician and/or trauma surgeon. Most acutely, they can present with airway obstruction from external hemorrhage, expanding closed space hematoma, or foreign body. Facial fractures can make speech poorly intelligible, making neurologic status or level of intoxication difficult to evaluate. Hemorrhage from facial injuries can be significant and difficult to control without a sufficient understanding of the involved anatomy. Even after appropriate hemostatic maneuvers, uncontrolled bleeding may still require interventional angiography for complete control.
With the exception of relatively rare maxillofacial emergencies, management of maxillofacial injuries is generally deferred until all life-threatening injuries have been addressed. The examination, however, can be performed as soon as the patient has been stabilized.
HEAD
This is a general examination of the cranio-maxillofacial skeleton and the overlying soft tissue. The patient should be carefully cleaned of all blood and debris. All soft tissue injuries should be noted at this time as well as any underlying bony injuries. Soft tissue trauma can be characterized as abrasions, contusions, burns, avulsions, and lacerations. All lacerations and avulsions should be checked for depth and involvement of vital structures (nerves, parotid gland/duct, etc.). In addition to all skin-penetrating trauma, the degree of blunt or crush injury to the surrounding tissue should be assessed, since this can significantly impact the results of primary closure or reconstruction. Soft tissue injuries should also be inspected thoroughly for and cleansed of foreign bodies and road debris.
The cranio-maxillofacial skeleton consists of a series of bony buttresses and prominences. They should be examined for steps, discontinuities, movement, and loss of projection. Careful palpation of the cranium, fronto-orbital bandeau, naso-orbital complex, zygomatic articulations, and mandible should be undertaken. In order to fully examine the scalp, cranium, and mandible, the cervical collar may have to be removed and in-line stabilization of the cervical spine maintained.
EYES
A comprehensive examination of the eyes is warranted early, since visual loss can be a devastating consequence of maxillofacial trauma. Up to 40% of midface fractures involve the orbit. Accurate examination can be difficult in the neurologically impaired patient and once substantial edema has set in. Visual acuity is generally checked with a pocket-sized card at about 14 inches distance. If this is not possible, finger counting, motion detection, and light perception are checked. Spectacle hematomas and subconjunctival hemorrhage are recorded, since these often indicate underlying bony fracture. Restriction of eye movement, vertical dystopia, and diplopia should be noted, although these can also occur with significant orbital edema or fracture. Pupillary size, in addition to direct and consensual response, is useful in indicating injuries along specific points of the visual pathways versus direct injury to the iris. Funduscopic examination can indicate elevation in intracranial pressure, retinal detachment, or ischemic injury to the optic nerve. Proptosis suggests hemorrhage within the orbital walls. In combination with a tense globe, ocular pain, decreased visual acuity, and a dilated pupil, it indicates retrobulbar hemorrhage, a surgical emergency requiring operative decompression with a lateral canthotomy and cantholysis. Blood in the anterior chamber of the eye, known as a hyphema, requires treatment and may delay surgical intervention for bony orbital injuries. All medial lid injuries through the lid margin must be examined for damage to the canalicular system and lateral upper lid injuries for involvement of the lacrimal gland. Finally, a ruptured globe must be ruled out in all patients with blunt or penetrating orbital trauma. Suspicion of globe injury should prompt ophthalmologic consultation.
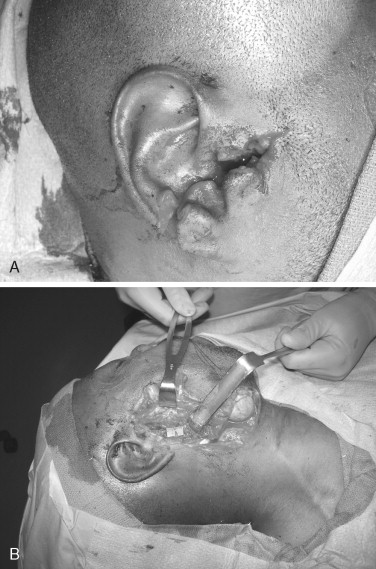
EARS
Auricular hematoma should be diagnosed and treated rapidly in order to avoid “cauliflower ear.” The mastoids should be inspected for ecchymosis or Battle’s sign, which along with hemotympanum and CSF otorrhea indicate cranial base fracture. Laceration of the external auditory canal may alert one to the possibility of condylar injury of the mandible.
NOSE/NERVES
Nasal deformity and mobility should be noted. The saddle nose deformity and broadening of the nasal dorsum are markers for structural nasal injury. Furthermore, an increase in the intercanthal distance indicates a naso-orbital-ethmoid injury. Impaired ability to move air through the nose may indicate bony or cartilaginous injury. Both septal fracture and hematoma can cause nasal obstruction. Septal hematomas must be diagnosed and evacuated early to prevent septal cartilaginous necrosis and thus subsequent nasal collapse. Epistaxis can be brisk and difficult to control. It may simply be the result of a mucosal tear or a result of direct injury to one of the terminal branches of the ethmoid or maxillary arteries. Epistaxis is usually managed by various forms of nasal packing; however, direct cautery and rarely transarterial embolization is necessary. The presence of cerebrospinal fluid (CSF) rhinorrhea should be noted in the upright patient; however, when recumbent, it may be more apparent in the nasopharynx. Nasal/nasopharyngeal CSF leak should alert the examiner to an anterior cranial base fracture and warn against the placement of a nasotracheal or nasopharyngeal tube. The presence of CSF can be verified by a halo test at the bedside or by the β 2 transferrin assay.
The main divisions of the trigeminal nerve should be checked for anesthesia or paresthesia. Injury to these nerves may herald an underlying fracture such as those to the mandible or orbitozygomatic complex, and the corneal reflex (V1) is important in the evaluation of brainstem injury. The continuity of the facial nerve should be verified by examination when possible in the awake and cooperative patient.
THROAT (ORAL CAVITY)
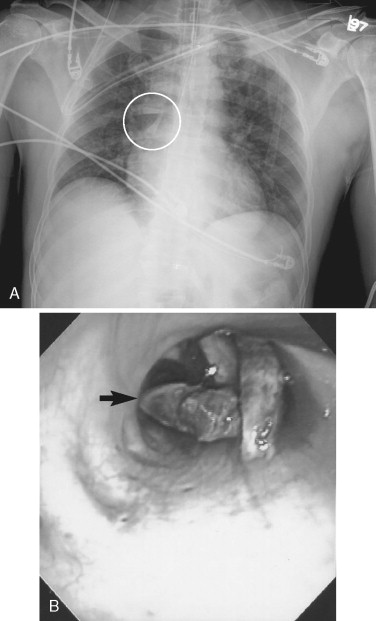
The occlusion should be evaluated and any missing teeth accounted for. Aspiration and ingestion of teeth can be ruled out with plain films of the chest and abdomen ( Figure 1-7 ). Loose dentures can partially occlude the airway. Steps and mobility in the occlusion are indicators of dentoalveolar or jaw fractures. Gingival-mucosal tears and hematomas can also signify jaw fractures and can lead to airway embarrassment in the case of substantial hemorrhage. Lateral open bites suggest mandible fractures or temporomandibular joint effusion/hemarthrosis. The dental midlines should be inspected. Anterior open bites or “gagged open” bites may indicate LeFort (I, II, or III) fracture. This can be verified by grasping the anterior maxillary teeth with one hand and the forehead or the zygomatico-frontal sutures with the other and checking for mobility.
CT scans and plain films can be used to confirm clinical findings and reveal occult injury. The use of multiple views and 3D reconstructions can help to characterize fractures and simplify difficult diagnoses. The addition of contrast to CT scans can help to detail soft tissue and vascular injury.
NECK
The neck is a collection of vital structures including major respiratory, vascular, and neural conduits. The superficial tissues of the neck offer little anatomic protection from injury. Severe neck injuries can result from penetrating or blunt trauma and may present an immediate threat to life as a result of airway compromise or hemorrhage. Because of the potential of injury to the airway or major blood vessels, aggressive evaluation and treatment of the neck are required to optimize outcome.
The major anatomic subdivisions of the neck are the anterior and posterior triangles. The majority of significant structures are located in the anterior triangle, including the trachea and the carotid sheath. The practitioner must consider both the vertical and horizontal level of injury in the evaluation of neck injuries. When the horizontal vector of a penetrating injury is considered, both the platysma and sternocleidomastoid muscles are important landmarks. The vertical neck is divided into three zones beginning at the thoracic inlet. Zone I constitutes the area from the sternal notch to the cricoid cartilage. Zone II covers the area from the cricoid cartilage to the angle of the mandible. Zone III is perhaps the most difficult to access acutely and extends from the angle of the mandible to the cranial base. Zone I injuries carry the highest incidence of mortality, whereas zone II injuries are the most straightforward to manage surgically.
Clinical signs of penetrating neck injury include hemorrhage, expanding hematoma, air movement through the wound with breathing, subcutaneous crepitus, voice changes, dysphagia, and odynophagia ( Figure 1-8 ). Preoperative work-up in patients with obvious injuries is minimal. Patients with penetrating injuries deep to the platysma in zone II are generally taken directly to surgery for exploration, whereas patients with injuries in zone I and zone III should undergo preoperative computed tomography angiography or angiography, if possible, to rule out significant vascular injury. The advantage of conventional angiography in this algorithm includes the ability to both diagnose and intervene should a vascular injury mandate embolization for hemorrhage control.
Aerodigestive tract injuries can be worked up before surgery or at the time of exploration. Neck injuries that do not mandate surgical exploration may require that the aerodigestive tract be worked up with a combination of bronchoscopy, upper endoscopy, or esophagram to exclude injury. Blunt trauma to the neck can result in laryngeal injury, which is sometimes difficult to assess via direct laryngoscopy, especially in the intubated patient. CT and endoscopy of the neck are commonly used to assess the larynx in blunt injury.
Any patient with head or facial trauma is presumed to have a cervical spine injury (C-spine) until proven otherwise. The neck and spine should be completely immobilized until an appropriate examination can be performed and the correct x-rays taken. The examination includes palpation along the dorsal neck and spine. Any obvious deviation in the vertebral column is noted. Flexion/extension views of the C-spine may be required to identify injury in the neurologically intact patient with pain or tenderness. Other specialized views like swimmers and open mouth odontoid are sometimes necessary. CT scan can be used whenever there is any question about the completeness or accuracy of a plain film. If the patient is unconscious or has distracting injuries with normal bony anatomy of the C-spine, MRI is used to exclude ligamentous injury.
NEUROLOGIC
The GCS should be reevaluated at this time, and a more detailed neurologic exam performed. In addition to level of consciousness, a thorough motor and sensory examination should be performed to include sensation, strength, proprioception, reflexes, tone, and coordination. Every attempt should be made to localize neurologic injury when present and a neurosurgery consult obtained when appropriate. The bulk of neurologic injuries come in the form of concussions, spinal injuries, diffuse axonal injury, epidural and subdural hematomas, and hypoxia/ischemia. CT scan of the head and spine may help to further support physical findings and define the extent of the injury.
CHEST
Immediately life-threatening injuries to the chest are commonly identified in the primary survey. Any thoracic injuries requiring treatment during the primary survey should be reassessed and a search for occult injuries completed. Chest x-ray is performed as part of either the primary or secondary survey, and this may show bony injury, hemothorax or pneumothorax, or widening of the mediastinum. Additional studies may be required to further delineate chest injury, such as echocardiogram, contrast radiography or CT scan, aortogram, or upper endoscopy.
- •
Ultrasonography—aortic disruption, pericardial effusion/cardiac tamponade, cardiac contusion, diaphragmatic injury
- •
Aortography—aortic dissection or disruption
- •
Contrast radiography or CT—esophageal injury, diaphragmatic injury, tracheobronchial injury
- •
Endoscopy—esophageal injury
ABDOMEN
In any patient who has unexplained hypotension following traumatic injury, an abdominal injury must be suspected. Initially, the diagnosis of an acute abdomen is more important than localizing the injury. At that time, a surgeon must be involved to assist in resuscitation and definitive treatment. The three regions of the abdomen to be assessed include the intrathoracic, the retroperitoneal, and the pelvic portion.
Visual inspection may alert one to seat belt strap marks, tire treads, or flank ecchymosis. Fractures to the lower ribs should raise suspicion of liver or spleen injury. A rigid, tense abdomen may indicate a bleed or hollow viscus injury. Obvious evidence of an abdominal injury such as peritonitis, hypotension, or evisceration will lead to exploratory laparotomy; however, in the hemodynamically stable patient, other studies may be useful in the localization of the injury. Diagnostic peritoneal lavage and FAST (focused assessment with sonography for trauma) are safe and sensitive tests that can be performed in the trauma resuscitation unit. CT scanning is very specific but requires patient transport and is therefore more suitable for the more stable patient.
PERINEUM/RECTUM/VAGINA
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


