In over 90% of cases, peri-implantitis is caused by poor diagnosis, poor planning, improper treatments, improper implant position, and inexperience of treating dentists.
Treatments for peri-implantitis have been largely ineffective and disappointing. Therefore, it is best to prevent peri-implantitis by eliminating factors that cause it. Factors that contribute to peri-implantitis may be divided into three categories: dentist-induced, patient-related, and the unknowns. In our experience, over 80% of peri-implantitis cases were iatrogenic and attributable to dentist-induced causes while about 15% were linked to patient-related factors. About 5% of cases seem to have occurred with no known causes. Since practically all of the dentist-induced and most of the patient-related factors are controllable, one can conclude that about 95% of all peri-implantitis cases may be completely preventable.
Dentist-Induced Peri-Implantitis
Let’s first define what we mean by ‘dentist’. It refers to anyone with a dental degree who may be a general dentist, prosthodontist, endodontist, implantologist, or a trained dental implant surgeon which includes oral surgeons and periodontists. Hence, dentist-induced peri-implantitis is not limited to any particular type of dentist. Additionally, being an oral surgeon or a periodontist does not necessarily reflect proficiency in implant surgery. A number of surgeons in both specialties focus on other types of treatments and do not perform dental implant surgery primarily in their practice.
A large percentage of patients with peri-implantitis can be linked to improper treatment and techniques by the treating dentists. Implant dentistry requires precision work-up, comprehensive diagnostics and planning, full understanding of its healing biology, and close collaboration between a skilled team including a surgeon and a restorative dentist. Most cases of peri-implantitis can be prevented when such principles are followed. However, due to ongoing trends of general practitioners performing surgical procedures without proper training, there is an overall increase in the incidence of dental implant complications. A recent report published by the American Dental Association (ADA) concluded that implant survival and success rates in general dental practices was lower than those reported in studies conducted in academic and specialty settings (1).
Key factors in preventing dental implant complications
1.Choosing the right team of dentists consisting of a surgeon and restorative dentist working as a team
2.Comprehensive examination and diagnostics consisting of full mouth series of X-rays, cone beam CT scan, study models, photos, and video
3.Collaborative treatment planning & proper staging
4.Following evidence-based and biologically-driven materials and techniques
Let’s take a look at the key contributing dentist-induced factors in peri-implantitis:
1.Placement of implant in insufficient bone
Placement of a dental implant where there is insufficient bone is a failure in diagnosis and planning, resulting not only in implant surface exposure and peri-implantitis, but also aesthetic and functional complications (Fig 4). This can be easily prevented by proper pre-surgical diagnostic imaging using CBCT and bone augmentation to develop the necessary dimension for implant placement. At least 1.5 – 2.0 mm of bone width surrounding the implant is required for long-term stability and support.
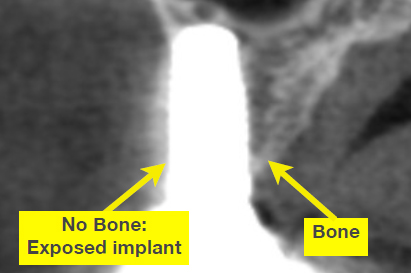
Fig 4 Implant is shown in a cross section of a CT scan: The selected implant was too wide and placed in insufficient bone resulting in exposed implant surface.
2.Poor positioning or alignment of the implant
A dental implant aligned poorly outside the confines of the bone will have insufficient bone coverage and result in tissue recession and exposed implant surface (Fig 5, 6, 7). Plaque adherence to the implants rough surface causes inflammation leading to pain, swelling, and infection. This can be avoided by making sure there is adequate bone for implant support, use of a surgical guide during implant placement, understanding of bite relationships, use of computer-assisted planning, and precise implant alignment during placement.

Fig 5 A poorly aligned dental implant positioned too far out resulting in gum recession and inflammation
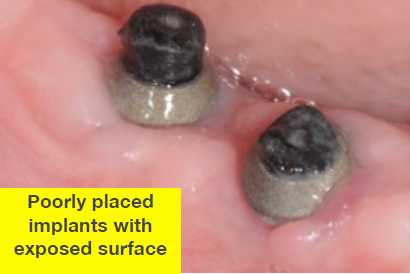
Fig 6 Two implants placed not deeply enough within bone; The surface of the implant is now exposed and causing inflammation
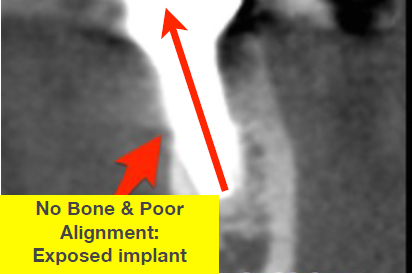
Fig 7 Shown in a cross section of a CT scan, this implant was placed off axis and misaligned with underlying bone which resulted in implant surface exposure and bone loss
3.Placement of the wrong implant size
Dental implants come in various lengths and diameters. The surgeon must select an appropriate implant size based on its location, type of bone, available bone, type of restoration, and proximity of vital structures such as nerves and sinus areas. A minimum 1.5 to 2.0 mm of bone coverage over an implant is required for proper coverage, integration, and gum tissue attachment. Therefore, if there is 7 mm width of bone, a maximum 4 mm diameter implant may be selected allowing a minimum of 1.5 mm of bone coverage on each side. If the implant selected is too wide, there will be insufficient bone and exposure of the implant surface which can easily harbor plaque and bacteria. The clinician must use CBCT to accurately measure the available width and height of bone and select the appropriate implant dimension that provides proper support, proper coverage with healthy bone and gum tissue, and proper aesthetic results.

4.Poor surgical implant placement technique
Traumatic surgical technique and poor management of bone and gum tissue during implant placement can easily cause irreversible tissue damage and loss of tissue vitality. Tissue damage can lead to gum and bone recession resulting in implant surface exposure and inflammation. Some examples of traumatic surgical techniques are excessive speed of the surgical drill and bone “burning” during site preparation, tearing of the gum tissue flap, and excessive forces during implant placement that can fracture the bone. Proper tissue management requires in-depth surgical skills and a thorough understanding of tissue biology and healing that are only mastered by trained surgeons. Also, poor implant handling and contamination during placement can cause infection.
5.Immediate implant placement in sites with periodontal disease or existing infection
Immediate implant placement refers to the placement of a dental implant at the time a tooth is extracted. There are basic guidelines for immediate implant placement that must be followed to achieve optimal results. One of those guidelines is absence of active infection from gum disease or abscess affecting the tooth being extracted and the site of the immediate implant placement. The bacterial contamination of a periodontally involved or infected tooth can make placement of an immediate implant a high risk for developing inflammation, peri-implantitis, infection, and ultimate failure (Fig 8a-c
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


