This article provides an overview of common color changes and soft tissue oral nodular abnormalities in children and adolescents. The clinical presentation and treatment options to address these conditions are presented in a concise approach, highlighting key features relevant to the oral health care professional.
Key points
- •
Oral mucosal lesions in children may present as ulcers, color changes, and alterations in size and configuration of oral anatomy.
- •
Leukoedema is a benign white lesion found bilaterally or unilaterally on the buccal or labial mucosa.
- •
Pseudomembranous candidiasis, a common condition in children, is an opportunistic fungal infection caused by Candida albicans , more likely to occur in children who had a recent use of antibiotics, corticosteroids, or extended exposure to pacifier.
- •
Melanotic nevus is an alteration of mucosal color. Nevi may be congenital or develop over the life span and mostly represent deviations of normal anatomy.
- •
Nodular vascular anomalies are currently classified into either benign tumors or vascular malformations based on the clinical presentation and evolution of the lesion and its histopathologic features.
Pediatric soft tissue oral lesions
Oral mucosal lesions in children may present as ulcers, color changes, alterations in size, and configuration of oral anatomy. This article presents a broad overview of oral conditions that affect children, focusing on abnormalities of color and nodular changes. Ulcerative disorders are covered extensively in other readily accessible literature.
Pediatric soft tissue oral lesions
Oral mucosal lesions in children may present as ulcers, color changes, alterations in size, and configuration of oral anatomy. This article presents a broad overview of oral conditions that affect children, focusing on abnormalities of color and nodular changes. Ulcerative disorders are covered extensively in other readily accessible literature.
Mucosal changes (color)
White Lesions
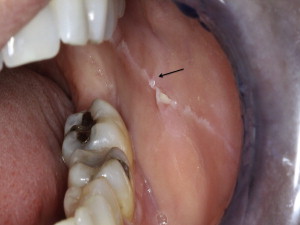
Frictional keratosis (Morsicatio buccarum)
The constant rubbing of the mucosa may cause white patches that can disappear if the causative agent habit is discontinued. Habits causing this finding include traumatic tooth brushing (toothbrush keratosis) and forcefully rubbing the tongue against the teeth (tongue thrust keratosis). The prevalence of frictional keratosis has been reported between 0.26% and 1.89% in children.
Clinical presentation
The condition is observed as a corrugated, gray or white lesion that may be smooth or rough and occasionally irregular with small loose tags of epithelium on the surface. The site of appearance is mostly the buccal mucosa.
Treatment
Removal of intraoral irritants and discontinuation of causative habits usually resolves this lesion.
Leukoedema
Leukoedema is a benign white lesion found bilaterally or unilaterally on the buccal or labial mucosa. The etiology is unknown but associations with tobacco smoking, local irritation, and malocclusion have been made. The prevalence differs in adults depending on the population examined and ranges between 0.96% and 58.00%, with the highest prevalence noted in African Americans.
Clinical presentation
Leukoedema is characterized by a diffuse white opacification that resolves when the mucosa is stretched.
Treatment
No treatment is needed, as this condition is benign.
Linea alba
This condition is a benign finding located on the buccal mucosa across the commissures and extending posteriorly toward the molars. The prevalence is 1.5% in children and up to 5.3% in adolescents.
Clinical presentation
Linea alba presents as a distinct white linear area on the buccal mucosa opposing the plane of occlusion ( Fig. 1 ). Occasionally, it has also been recognized on the lateral border of the tongue.
Treatment
No treatment is needed, as this condition is benign.
Hairy tongue
Hairy tongue is a benign condition that arises from abnormal elongation of the filiform papillae of the tongue (1–12 mm) or the proliferation of bacteria that release pigments on them. This condition may also be caused by intrinsic factors, such as antibiotics (erythromycin), antipsychotics (olanzapine), iron supplements, or radiation therapy. Extrinsic causative factors are primarily related to diet (coffee, tea), poor oral hygiene, mouth washes, or smoking, a concern in adolescent patients. The prevalence of hairy tongue in children is unknown.
Clinical presentation
Papillary elongation gives the appearance of thick, hairylike surface on the dorsal tongue. The condition may present with superficial coating that blunts the hairy appearance ( Fig. 2 ).

Treatment
Good oral hygiene, diet restriction, smoking cessation, or tobacco counseling and brushing with 1% to 2% hydrogen peroxide solution or diluted sodium hypochloride has been suggested.
Pseudomembranous candidiasis
This common condition in children is an opportunistic fungal infection caused by Candida albicans , more likely to occur in children who had a recent use of antibiotics, corticosteroids, or extended exposure to pacifier. It is a hallmark oral finding in children with systemic conditions, such as endocrine disorders, leukemia, chemotherapy, radiation therapy, transplantation, prematurity, and malnutrition. The prevalence is 0.99% to 8.57% in children and 37.00% of infants.
Clinical presentation
This condition is presented as superficial white plaques on the mucous membranes that can be wiped off. These white plaques can be seen on the buccal and labial mucosa, hard and soft palate, tongue, and oropharynx.
Treatment
Treatment usually includes gentian violet or topical nystatin for infants, and nystatin (topical) or topical clotrimazole for older children. Systemic fluconazole, ketoconazole, or itraconazole may be used for children who are at risk of developing systemic infection or are intolerant to topical therapy.
White sponge nevus
White sponge nevus is a benign asymptomatic condition due to an autosomal dominant inheritance. Lesions clinically present as bilateral white plaques that are thickened, spongy, and folded. The buccal mucosa is the most frequent site but the condition also may be seen on the labial mucosa, floor of the mouth, and gingiva. They are usually present at birth or in early childhood and may occasionally develop in adolescence. The prevalence is 1.54%.
Clinical presentation
White, raised, folded unilateral or bilateral tissue on tongue or buccal mucosa. The tissue cannot be removed. The differential diagnosis may include leukoplakia, chemical burns, trauma, tobacco, and Candida infections.
Treatment
No treatment is necessary unless masticatory function is compromised.
Red and/or white lesions
Petechiae, Purpura, Ecchymosis
These red lesions are commonly caused by trauma affecting the underlying vasculature. They are frequently a sign of bleeding disorders, such as thrombocytopenia or hemophilia, and may occasionally be associated with leukemia and anemia. The prevalence of vascular lesions is 1.89% to 8.39% in children and may be up to 42.8% in children with systemic disease.
Clinical presentation
The lesions are predominantly seen on the lips, tongue, hard palate, and gingiva and are classified as follows:
- •
Petechiae: pinpoint hemorrhages
- •
Purpura: 2-mm to 2-cm hemorrhages
- •
Ecchymosis: >2 cm hemorrhages
Treatment
Treatment includes the initial investigation of the source of the trauma to rule out child abuse. All other lesions associated with medical conditions or medications must be referred for further medical workup.
Erythematous Candidiasis
The etiology of the symptomatic form is often linked to vitamin B12 and folate deficiency, as well as recent antibiotic or steroid therapy. The asymptomatic form is characterized by chronic erythema of tissues covered by prostheses, such as dentures and retainers. Lesions are commonly seen on the palate and occasionally on the mandibular tissue. The prevalence in children is unknown. It is presumed to be lower than the prevalence of pseudomembranous candidiasis.
Clinical presentation
Red macular lesions that are usually asymptomatic or occasionally symptomatic with a burning sensation on the tongue or mouth and a bright red appearance.
Treatment
See pseudomembranous candidiasis.
Angular Chelitis
This disorder is a chronic inflammation of the skin and labial mucosa at the corners of the mouth. The etiology may be due to nutritional deficiencies (riboflavin, folate), anemia (iron deficiency) allergy, infections, physical irritation, low socioeconomic status, and bruxism. The prevalence is 3% in children and 9% in adolescents.
Clinical presentation
Angular chelitis is characterized by the presence of painful cracking, fissuring, and erythema on bilateral commissures. Hemorrhage may be a concomitant finding.
Treatment
See pseudomembranous candidiasis.
Erythema Migrans (Benign Migratory Glossitis)
Also known as geographic tongue, erythema migrans is a benign condition affecting the dorsum of the tongue. The etiology is unknown, but studies have suggested an association with atopy, psoriasis, and fissured tongue and included a genetic linkage between the 2 conditions. Geographic tongue is also more prevalent in allergic patients. Prevalence ranges between 0.37% and 14.3% in pediatric patients depending on the populations examined and may be up to 40.6% in children with systemic disease.
Clinical presentation
Clinically, benign migratory glossitis appears as a well-configured maplike appearance due to the well-defined depapillated erythematous regions that are surrounded by white borders ( Fig. 3 ).

Treatment
No treatment is necessary, other than reassurance. In adults, zinc, topical anesthetics, steroid gels, and antihistamine mouth rinses have been suggested for symptomatic cases.
Median Rhomboid Glossitis
This particular fungal infection has predisposing factors, such as Candida infections, and immunosuppressive diseases, such as diabetes. Other risk factors reported in the literature, but have inconsistent results include age, smoking, and removable prostheses. Prevalence in pediatric patients has been reported between 0% and 1.23%.
Clinical presentation
The condition presents as a well-circumscribed central papillary atrophy of the tongue, typically located in the midline on the dorsum of the tongue anterior to the circumvallate papillae ( Fig. 4 ). The surface of the lesion is smooth and glossy and is asymptomatic in most patients; however, pain, irritation, and pruritus have been reported. Tongue lesions may occasionally present with palatal inflammations or kissing lesions that are considered a marker for HIV infection.

Treatment
Because this is an asymptomatic lesion, treatment is not indicated. However, the lesion often responds to antifungal treatment with nystatin, fluconazole, or clotrimazole as a suspension or oral troches.
Brown-black lesions
Physiologic Pigmentation
This pigmentation is the most common form of diffuse and bilateral pigmentation that arises from the increased production of melanin in dark-skinned populations (Middle Eastern, African American, and occasionally Asians). In general, conditions that increase the prevalence of this pigmentation are race/ethnicity, increased age, smoking, pregnancy, endocrine syndromes, and hormonal changes. Atypical cases have been reported in newborns. Peutz-Jeghers syndrome is an autosomal dominant trait that is associated with multiple intraoral and perioral pigmentations, most of which do not require treatment and involute after the first decade of life. However, the early establishment of a diagnosis is critical for a gastroenterology workup for intestinal polyps and hamartomas that have a 2% to 3% tendency for malignant transformation. Addison disease or adrenal insufficiency is an autoimmune disease resulting in insufficient secretion of glucocorticoids and mineralocorticoids. Initial symptoms include diffuse bronzing of the skin and mucous membranes. In the oral cavity, the pigmentation is commonly located on the gingiva, tongue, buccal mucosa, and hard palate. Occasionally, isolated macules maybe present. Oral surfaces frequently exposed to trauma may develop the pigmentation more frequently. The prevalence of oral pigmentation in children is 13.5% with an onset in the first/second decades.
Clinical presentation
The pigmentation is commonly found on the attached gingiva. Occasionally, the buccal mucosa, palate, and lips, as well as the dorsal surface of the tongue are affected.
Treatment
Treatment is not required. Intraoral pigments associated with Peutz-Jeghers syndrome require monitoring and evaluation by a gastroenterologist for the development of mucosal gastric malignancies.
Amalgam Tattoo/Graphite
This disorder occurs as sequelae of surgical oral interventions or removal of amalgam restorations. The prevalence in children is 1.3%.
Clinical presentation
Amalgam tattoo is a localized flat blue-gray solitary or multiple lesions of variable sizes and shapes (0.1–2.0 cm). It is commonly found on the attached and alveolar mucosa next to teeth restored with amalgam, and may be occasionally seen dispersed in the buccal mucosa or the floor of the mouth. Graphite pigmentation is a common finding in the anterior palatal area in children due to trauma. It appears clinically as an ill- defined flat gray/black pigmentation.
Treatment
No biopsy is indicated in most cases unless a confirmation of amalgam is needed when the patient’s medical history suggests susceptibility to dermatologic malignancy.
Melanotic Nevus
Melanotic nevus is an alteration of mucosal color. Nevi may be congenital or develop over the life span and mostly represent deviations of normal anatomy. It is important to mention the histologic classification of nevi, as it may impact lesion prognosis:
- 1.
Junctional: proliferation of the nevus cells at the tips of the rete pegs that are close to the surface and are confined in the epithelium.
- 2.
Compound: proliferation of nevus cell into the epithelium and connective tissue.
- 3.
Intradermal/intramucosal: nevus cells are located in the lamina propria and do not contact the basement membrane. These lesions are dome shaped, typically light brown in color and are commonly seen on the gingiva, and labial and buccal mucosa.
- 4.
Blue nevi: proliferation of spindle cells within the deep connective tissue and remotely from the surface epithelium. This lesion is commonly seen on the hard palate. They are further classified into atypical blue nevus, locally aggressive blue nevus, and congenital giant melanotic nevus with nodular growth.
- 5.
Other melanotic nevi include the combined nevus and the Spitz nevus, which may be located on the palate or tongue.
- 6.
The congenital melanotic nevi with large nodules.
The prevalence of oral nevi in children is unknown, and published figures include older patients.
Clinical presentation
Melanotic nevi present as localized brown, blue, gray, black, or colorless macule or papule and rarely polypoid that range from 0.1 to 3.0 cm ( Fig. 5 ). The nevi are commonly located on the hard palate, buccal mucosa, and gingiva at 41.0%, 12.0%, and 11.5% respectively.
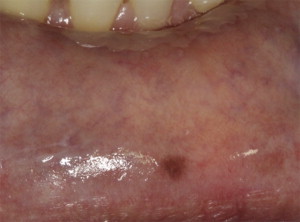
Treatment
Treatment includes excisional biopsy to rule out mucosal melanoma, especially if the lesion is located in the palate. Transformation of pigmented nevi to melanoma is not well documented in the literature.
Soft Tissue Nodules
Most reports establish that 90% to 98% of soft tissue biopsies in children are diagnosed as benign. These benign lesions can be divided into 2 categories according to their etiology: inflammatory/reactive lesions and benign neoplasms. Malignancies are uncommon in children; however, because when they occur they cannot be clinically distinguished from benign lesions, these must be biopsied to establish a definitive diagnosis.
Inflammatory/reactive lesions
Mucocele (mucous extravasation phenomenon)
A mucocele is a lesion that results from the extravasation of mucous into the connective tissue of the oral mucosa secondary to the rupture of a minor salivary gland duct. The prevalence of mucoceles in children has been reported between 0.04% and 1.00%.
Clinical presentation
Mucoceles appear most frequently as slightly bluish nodules measuring smaller than 1.5 cm, most of which have a history of increasing and decreasing in size. On palpation, they can be fluctuant or firm. If the extravasated mucous is located in the deeper connective tissue, they may appear as pink nodules. The most common location is the lower labial mucosa, which is a site that is frequently traumatized by biting. Other common locations include the floor of the mouth, ventral tongue, and buccal mucosa ( Fig. 6 ).





