-
Outline
![]()
The patient who abuses alcohol or other substances presents significant problems to the practitioner as well as to society. These problems are found in many countries worldwide. Substance abuse–related disorders are common and cause significant social, psychological, and health problems among users and those around them. The substance-abusing patient is more likely to suffer from a variety of oral problems and to present unique challenges that will call on skills and sensitivities that are not typically required of the dental team in the practice of general dentistry.
The focus of this chapter is to discuss ways in which the general dentist and dental team can recognize alcohol and substance abuse in patients, how they can contribute to addiction management support in those patients, and how they can plan and safely carry out the treatment needed to rehabilitate and maintain the oral health of the patient who is actively using, as well as those who are in recovery.
Challenges to the dentist
The dental practitioner will face many frustrations in the management of the patient who abuses alcohol or other substances. Both the active and the recovering user typically bring many fears and some measure of guilt to the dental setting. The recovering user may fear uncontrolled pain or exhibit an underlying anxiety of relapse into substance abuse. The individual may be concerned that he or she will be differently treated and that the dentist will be judgmental about the addiction, as well as about the individual patient’s appearance, oral condition, and/or lack of home care. The active substance user may contrive elaborate fabrications to explain his or her neglected oral health or chronic lateness or missed dental appointments. Such a patient will often deny responsibility for his or her poor oral health and may exhibit argumentative behavior, have difficulty sitting still, and need frequent “bathroom breaks” (behavior exhibited as a cover for drug use during the dental appointment).
Recognition of patient substance abuse
Early identification of substance abuse is important to reduce patient morbidity and, in some cases, mortality. Dentists may see these patients before any other healthcare professionals and thus have an excellent opportunity to assist them in recognizing and confronting a substance abuse problem—but this is no easy task. In such a situation, the dentist can provide substance abuse prevention information, or direct the patient to a substance abuse assessment and treatment center or substance abuse professional. The dental team can also screen for potential liver disease, prolonged bleeding, delayed wound healing, or other systemic conditions potentially harmful to these patients. Dentists can inform patients about tobacco cessation programs and other preventive measures to help reduce the risk of developing oral cancer. These are important opportunities, but they are also a challenge, particularly in the context of a busy dental practice.
The substance-abusing patient, particularly an active user, may not be forthcoming about his or her medical and drug history. It is not unusual for these patients to be defensive, evasive, and untruthful in communicating health-related information to the dentist. If the individual has a history of substance abuse, he or she may be reluctant to divulge the information for fear of loss of medical benefits or insurance coverage, or loss of social position, job, or self-esteem. Some individuals may be in denial and may not recognize or be willing to admit to a having a problem. Others may be well aware of the addiction, but as part of the pattern have adopted an “addiction preservation” mentality and will go to great lengths to hide, rationalize, explain away, or minimize the import of the chemical dependence. Unfortunately, some dentists may also be reluctant to delve into the issue of a patient’s substance abuse, because it may seem too intrusive or because they view the disorder as a moral shortcoming rather than a valid psychiatric disorder. It is imperative that this reluctance and fear on the part of both patient and provider be overcome.
Delivery of dental care
Patients receiving dental treatment while under the influence of alcohol or drugs present an unsafe and difficult working environment for the dental team and can place themselves at high risk for a medical emergency while in the dental office. Patients under the influence of some drugs are difficult to communicate with, may be uncooperative, and often do not follow prescribed therapeutic regimes. Typically, they have poor oral hygiene. They often lack an interest in oral health and are not motivated to receive regular dental care, seeking only relief of pain or infection.
Others may exhibit initial overt enthusiasm for high-quality dental care but soon lose that enthusiasm and fail to follow through with treatment that they have committed to. It is not uncommon for the abusing patient to cancel or break dental appointments or to be frequently tardy. Similarly, such individuals may be erratic or late in paying for dental services. They may present to the dental visit while under the influence—needing to “mellow out” or “get fortified” in preparation for the anxiety-evoking dental visit. Special precautions must be taken when prescribing medications for postsurgical procedures. Analgesics, sedatives, or antibiotics that are likely to cause adverse reactions with alcohol or psychiatric medications should be avoided.
There are inherent dangers when patients mix alcohol with other central nervous system (CNS) depressants, such as narcotics, sedatives, or benzodiazepines. Taken together, these substances have an additive effect that may have lethal consequences. The dentist must caution their patients against taking these medications together.
Behavioral/compliance issues
Behavioral problems exhibited by the abusing patient (aggressiveness, belligerence, melancholia, euphoria) can arise because of one or more possible causes or may be a direct effect, side effect, or residual effect of the substance being ingested. Some antisocial behaviors may be a manifestation of a delayed effect, rebound, flashbacks, or withdrawal symptoms. Some defensive, secretive, manipulative, or excusatory behavior may be part of a conscious or unconscious effort at self-rationalization or self-denial. Some patients also become remarkably adept at becoming the “con artist” in a dual effort to hide the addiction and simultaneously maintain the appearance of a normal lifestyle with the accompanying benefits of social acceptance and the appearance of success.
Behavioral problems in the office can be a major disruption. Patients may have untoward reactions to treatment or become belligerent. Less dramatic, but just as detrimental, is the abusing patient who becomes distant, remote, unemotional, and disengaged. This behavior can be a direct effect of the abused substance, a side effect of therapeutic medications, or an otherwise induced mental depression—a secondary effect of the substance abuse.
Many behavioral changes can be evoked by substance use, and these may become apparent at any time during the course of treatment. The dentist should be alert to the possibility of behavioral anomalies at any initial examination visit. Patients who regularly ingest ethanol and other mind-altering substances, either alone or in combination, may exhibit the following:
- •
Denial, avoidance behaviors (cancel, break appointments, be frequently tardy)
- •
Noncompliance with oral hygiene measures and other instructions
- •
Lowered pain threshold and increased dental, gingival, and oral sensitivity
- •
Anxiety, fidgeting, excitation, nervousness
- •
CNS depression, lethargy, altered affect, and loss of motivation
- •
Gagging and inappropriate behaviors in the operatory
- •
Unrealistic expectations about the nature and extent of treatment
- •
Diminished ability to tolerate and/or willingness to pay for treatment
Challenges to the dentist
The dental practitioner will face many frustrations in the management of the patient who abuses alcohol or other substances. Both the active and the recovering user typically bring many fears and some measure of guilt to the dental setting. The recovering user may fear uncontrolled pain or exhibit an underlying anxiety of relapse into substance abuse. The individual may be concerned that he or she will be differently treated and that the dentist will be judgmental about the addiction, as well as about the individual patient’s appearance, oral condition, and/or lack of home care. The active substance user may contrive elaborate fabrications to explain his or her neglected oral health or chronic lateness or missed dental appointments. Such a patient will often deny responsibility for his or her poor oral health and may exhibit argumentative behavior, have difficulty sitting still, and need frequent “bathroom breaks” (behavior exhibited as a cover for drug use during the dental appointment).
Recognition of patient substance abuse
Early identification of substance abuse is important to reduce patient morbidity and, in some cases, mortality. Dentists may see these patients before any other healthcare professionals and thus have an excellent opportunity to assist them in recognizing and confronting a substance abuse problem—but this is no easy task. In such a situation, the dentist can provide substance abuse prevention information, or direct the patient to a substance abuse assessment and treatment center or substance abuse professional. The dental team can also screen for potential liver disease, prolonged bleeding, delayed wound healing, or other systemic conditions potentially harmful to these patients. Dentists can inform patients about tobacco cessation programs and other preventive measures to help reduce the risk of developing oral cancer. These are important opportunities, but they are also a challenge, particularly in the context of a busy dental practice.
The substance-abusing patient, particularly an active user, may not be forthcoming about his or her medical and drug history. It is not unusual for these patients to be defensive, evasive, and untruthful in communicating health-related information to the dentist. If the individual has a history of substance abuse, he or she may be reluctant to divulge the information for fear of loss of medical benefits or insurance coverage, or loss of social position, job, or self-esteem. Some individuals may be in denial and may not recognize or be willing to admit to a having a problem. Others may be well aware of the addiction, but as part of the pattern have adopted an “addiction preservation” mentality and will go to great lengths to hide, rationalize, explain away, or minimize the import of the chemical dependence. Unfortunately, some dentists may also be reluctant to delve into the issue of a patient’s substance abuse, because it may seem too intrusive or because they view the disorder as a moral shortcoming rather than a valid psychiatric disorder. It is imperative that this reluctance and fear on the part of both patient and provider be overcome.
Delivery of dental care
Patients receiving dental treatment while under the influence of alcohol or drugs present an unsafe and difficult working environment for the dental team and can place themselves at high risk for a medical emergency while in the dental office. Patients under the influence of some drugs are difficult to communicate with, may be uncooperative, and often do not follow prescribed therapeutic regimes. Typically, they have poor oral hygiene. They often lack an interest in oral health and are not motivated to receive regular dental care, seeking only relief of pain or infection.
Others may exhibit initial overt enthusiasm for high-quality dental care but soon lose that enthusiasm and fail to follow through with treatment that they have committed to. It is not uncommon for the abusing patient to cancel or break dental appointments or to be frequently tardy. Similarly, such individuals may be erratic or late in paying for dental services. They may present to the dental visit while under the influence—needing to “mellow out” or “get fortified” in preparation for the anxiety-evoking dental visit. Special precautions must be taken when prescribing medications for postsurgical procedures. Analgesics, sedatives, or antibiotics that are likely to cause adverse reactions with alcohol or psychiatric medications should be avoided.
There are inherent dangers when patients mix alcohol with other central nervous system (CNS) depressants, such as narcotics, sedatives, or benzodiazepines. Taken together, these substances have an additive effect that may have lethal consequences. The dentist must caution their patients against taking these medications together.
Behavioral/compliance issues
Behavioral problems exhibited by the abusing patient (aggressiveness, belligerence, melancholia, euphoria) can arise because of one or more possible causes or may be a direct effect, side effect, or residual effect of the substance being ingested. Some antisocial behaviors may be a manifestation of a delayed effect, rebound, flashbacks, or withdrawal symptoms. Some defensive, secretive, manipulative, or excusatory behavior may be part of a conscious or unconscious effort at self-rationalization or self-denial. Some patients also become remarkably adept at becoming the “con artist” in a dual effort to hide the addiction and simultaneously maintain the appearance of a normal lifestyle with the accompanying benefits of social acceptance and the appearance of success.
Behavioral problems in the office can be a major disruption. Patients may have untoward reactions to treatment or become belligerent. Less dramatic, but just as detrimental, is the abusing patient who becomes distant, remote, unemotional, and disengaged. This behavior can be a direct effect of the abused substance, a side effect of therapeutic medications, or an otherwise induced mental depression—a secondary effect of the substance abuse.
Many behavioral changes can be evoked by substance use, and these may become apparent at any time during the course of treatment. The dentist should be alert to the possibility of behavioral anomalies at any initial examination visit. Patients who regularly ingest ethanol and other mind-altering substances, either alone or in combination, may exhibit the following:
- •
Denial, avoidance behaviors (cancel, break appointments, be frequently tardy)
- •
Noncompliance with oral hygiene measures and other instructions
- •
Lowered pain threshold and increased dental, gingival, and oral sensitivity
- •
Anxiety, fidgeting, excitation, nervousness
- •
CNS depression, lethargy, altered affect, and loss of motivation
- •
Gagging and inappropriate behaviors in the operatory
- •
Unrealistic expectations about the nature and extent of treatment
- •
Diminished ability to tolerate and/or willingness to pay for treatment
Patient assessment (signs and symptoms of substance abuse)
Obtaining the patient’s health history
Obtaining a thorough medical and oral health history is an essential first step before initiating comprehensive dental treatment for any patient. The history has particular relevance and importance for the substance-abusing patient. The history is essential in eliciting information about any associated health problems that the patient might have—problems that leave the patient susceptible to a host of different medical emergency problems. Evaluation of the health history can help divulge psychosocial complications of the addiction, any or all of which may require modifications to dental treatment. The history can also help the dental team to identify any comorbid conditions, side effects of the abused substances, or any potential adverse drug interactions.
The importance of establishing a trusting relationship with the patient, and doing so as quickly as possible, cannot be overemphasized. The stigma associated with alcoholism and other forms of substance abuse may cause the patient to fail to disclose a history of substance use and abuse. For the abuser, it is easy to find reasons to deny the abuse patterns, and, in the mind of the abuser, there are potential risks associated with divulging such a condition. It is important for the practitioner to reaffirm to the patient the confidentiality of the interview and of the findings. Similarly, it is important to explain to the patient why questions related to substance use and abuse are relevant and necessary to the practice of dentistry. In an environment of mutual trust and confidentiality, most substance using and abusing patients will be forthcoming. The goal is to obtain complete and accurate information so that dental care can be delivered in a safe manner and in a way that is in the patient’s best short- and long-term interests.
The methods for obtaining an oral and medical health history are similar to those used with other adult comprehensive care patients (see Chapter 1 ). The patient should be treated with respect, and questions should be expressed in an objective, nonjudgmental manner. The patient should be sitting upright facing the interviewer. Making eye contact is important to reinforce the idea that the dentist is primarily interested in the patient’s oral health and overall well-being. The dentist should be aware of the patient’s demeanor and body language throughout the interview process. When asked a difficult question, the patient may exhibit diminished eye contact and/or a defensive posture, possibly signaling an avoidance response. If the patient’s answers are vague or an effort seems to be being made to circumvent answering the questions, it may be a sign of denial of a substance abuse problem. The practitioner must also be aware that an anxious patient, or a patient with psychological problems and/or who feels falsely accused, may appear to be similarly defensive and less than forthcoming with historical information.
The patient should be asked about the type, frequency, and amount of alcohol consumption or recreational drugs, and the use of any prescription or nonprescription pharmaceuticals. Particular notice should be taken of any off-label drug uses—and an evaluation made as to whether those uses are medically plausible. If in doubt, the dentist should consult with the patient’s physician or pharmacist. The dentist should also be alert to what would seem to be unusually high dosages of any mind-altering substances. At this point, the dentist cannot assume that the patient is a substance abuser simply because he or she is using a medication for an atypical reason or taking a higher-than-normal amount of a mind-altering drug. For example, many individuals who suffer from chronic, acutely painful conditions use high doses of morphine or methadone for legitimate and medically appropriate reasons. Any current or past history of tobacco use should also be recorded. For individuals who have smoked cigarettes, a pack-year history is a useful way to capture and record that information (see Chapter 1 ).
A positive response to any of the initial substance-related queries on the health history questionnaire (or to any related initial trigger questions on the open-ended medical history) should be pursued with additional open-ended questions to determine whether an abuse problem exists, whether consultation with another healthcare provider is warranted, and/or whether any modification to the dental plan of care is needed. If not initially reported, the dentist should clarify the type of drug, quantity, frequency, most recent time of use, and pattern of use. Follow-up questions relating to a family history of substance abuse and the consequences of that abuse may be appropriate as well. With the patient’s permission, additional useful information about types of substance abuse, amount of use, and the behavioral effects and level of control of the addiction can often be obtained from family members, loved ones, and friends.
A careful review of the patient’s health history may reveal risk indicators or conditions associated with the development of alcoholism or other forms of substance abuse. Signs that may indicate a problem include chronic headaches, history of low pain threshold, seizures, insomnia, anxiety, irritability, stomach problems, repeated motor vehicle accidents, and unexplained injuries or visits to hospital emergency rooms. There are also several medical conditions which, if reported on the patient’s health history, may suggest substance abuse—particularly alcoholism. Although these conditions are not pathognomonic, taken collectively and in light of positive responses to some of the previous questions, they should raise questions as to a significant substance abuse problem. These conditions are
- •
Prolonged bleeding (normal values for bleeding time is usually between 1 and 9 minutes; in most cases of wisdom teeth extraction, bleeding usually stops after 6 to 12 hours). ,
- •
Bruising
- •
Anemia
- •
Altered immune response
- •
Hypertension
The following findings from the oral health history may also be indicative of a substance abuse problem:
- •
Recurring episodes of ill-diagnosed oral pain
- •
Asking for specific (narcotic) analgesics
- •
Patient’s requesting sedation before the dentist has even examined the patient
- •
History of recurrent decay due lack of proper brushing and flossing
- •
Disaffection and poor experience with multiple care providers
Some other behaviors indicative of substance abuse may be revealed in the history or may become apparent at subsequent appointments:
- •
Noncompliance with prescribed therapy
- •
Tardiness or failure to show for appointments
- •
Emotional fluctuations
- •
Constant excessive movement or inability to sit still, crying without reason, or other behavior that cannot be explained by other causes (such as psychological disorders, as discussed in Chapter 15 )
Head, face, and neck—intraoral/extraoral examination
Although the process of performing an extraoral and intraoral soft tissue examination on the patient with known, suspected, or potential substance abuse is the same as for any other patient, this portion of the examination often provides valuable clues for the dental team as to whether there is an abuse problem and the nature and severity of the problem, as well as the specific oral pathologies that will need to be addressed in the course of dental treatment ( Table 13-1 ). Some of these clues may be evident when the patient first enters the operatory, or they may emerge (or reemerge) at subsequent visits. Does the individual exhibit a staggering or halting gait? Slurred speech? Does the individual make eye contact? Does he or she have a wasted appearance? Is he or she lethargic, with unclean clothing and hair, and exhibiting body and breath odors?
| Clinical Finding | Associated Substance |
|---|---|
| Jaundice of skin, mucosa, sclera | Alcohol |
| Chronic rhinitis | Powder cocaine |
| Nasal septal defects | Powder cocaine |
| Facial/lip burns | Crack cocaine/methamphetamine |
| Dilated pupils | Stimulants/hallucinogens/inhalants |
| Constricted pupils | Narcotics/opiates |
| Venipuncture sites/needle tracks | Heroin |
| Stained fingers | Marijuana/tobacco |
| Excessive thirst | Methamphetamine |
| Unusual dental decay patterns | Methamphetamine |
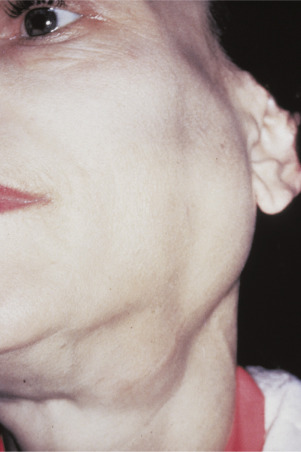
During the extraoral examination, the dentist should look for dermatologic conditions, palmar or facial erythema, spider angiomas, or peripheral edema. Is the patient’s skin, mucosa, or the sclera of the eyes jaundiced? Are there any inflammatory nasal mucosal changes, such as chronic rhinitis, nasal septal defects (powder cocaine), facial or lip burns (crack cocaine), dilated or constricted pupils, red eyes, venipuncture sites (needle tracks), stained fingers (marijuana and tobacco users), excessive thirst, or unusual decay patterns? Other important findings include hypertension, tachycardia, or other cardiovascular disorders. Relevant extraoral findings may include hand tremor, bloated appearance, baggy eyes or puffy facial features, excessive perspiration, bilateral swelling of parotid glands ( Figure 13-1 ), red or ruddy complexion, and telangiectasias.
Common intraoral findings include dry lips, angular cheilitis, persistent oral ulceration or infection, enlarged salivary glands (sialadenosis), dry mouth, or candidiasis. The mucosa may exhibit an anemic pallor. Intraoral signs of an associated coagulopathy often include petechiae, purpura, and ecchymosis. Mucosal bruising, erosion, and ulceration are not uncommon. The patient may exhibit glossitis, or gingival bleeding. Many substance-abusing patients exhibit signs of poor oral hygiene with accompanying gingivitis, periodontitis, and root caries. The teeth may show evidence of erosion, bruxism, cervical notching, and/or attrition.
Substance users often also use tobacco. With tobacco use, there may be nicotine patches, smoker’s keratosis, snuff pouch, or nicotine stomatitis. Alcohol and tobacco are major contributing factors in the pathogenesis of oral cancer. Consequently, it is imperative that thorough intraoral examinations are conducted in these patients for the detection of premalignant or malignant lesions. While carrying out the examination, the dentist has an opportunity to inform the patient about the effects of alcohol, tobacco, and other substances on the oral cavity, and do some further investigative work in oral cancer prevention. If the patient exhibits signs of tobacco use, it is incumbent on the dentist to educate the individual about the health risks of tobacco, including its harmful effects on the oral structures and its relationship to heart disease, hypertension, and lung cancer. ,
Effects of inappropriate drug use and their implications
Unpredictable drug metabolism
Patients may have unpredictable drug metabolism, so an understanding of all medications and their interactions is imperative. In mild to moderate alcoholic liver disease, significant enzyme action results in increased tolerance of local anesthetics, sedative and hypnotic drugs, and general anesthesia. Larger than normal doses of medications may be required to achieve the desired results. In individuals with significant liver damage, drug metabolism will be markedly diminished. For those patients who are more likely to take larger doses of medication to achieve the desired effect, this can result in the ingestion of a potentially lethal dose of the drug.
Often patients will use combinations of tobacco products, alcohol, prescription drugs, and other mind-altering substances. These may have simultaneously additive, synergistic, or conflicting pharmacologic effects. Unpredictable and variable euphoric, depressive, hallucinogenic, and sedative effects may result. Even more disturbing for the dentist or healthcare worker is the potential for highly unpredictable and extremely variable systemic effects. Many combinations of licit and illicit substances result in a dangerous cocktail that, when ingested, will be difficult for medical personnel to treat effectively, and that may have potentially life-threatening consequences.
If alcoholic hepatitis or cirrhosis is present, the dentist should generally reduce normal dosages of all drugs that are metabolized in the liver or avoid their use altogether. Aspirin should be avoided before any surgical procedures in patients with liver dysfunction or thrombocytopenia because of the potential for bleeding. Acetaminophen should be used with caution in patients with impaired liver function, because granulocytopenia and anemia may be intensified. If acetaminophen is used in conjunction with alcohol, severe hepatocellular disease with potentially fatal consequences may occur.
Ketoconazole should not be prescribed if patients are taking antacids, phenytoin, cimetidine, or rifampin, as it can be synergistic with other hepatotoxins. When ingested with alcohol, this reaction mimics the effect of disulfiram (Antabuse). When both alcohol and disulfiram are present in the circulation at the same time, the normal metabolic pathway of ethanol is disrupted by inhibiting aldehyde dehydrogenase. This action results in increased blood levels of acetaldehyde, a toxic substance that makes the patient violently ill, usually causing nausea, vomiting, sweating, and diarrhea. ,
Infectious diseases, infective endocarditis, and nutritional deficiencies
Patients who have a history of intravenous (IV) drug use are at risk for infectious diseases, such as hepatitis B or C, human immunodeficiency virus (HIV) infections, and infective endocarditis. Patients who are known to be IV drug users and who have not had a cardiac evaluation should be referred to a physician for an evaluation and echocardiogram, with the objective of determining their risk status for endocarditis. If the patient is determined to be at risk for endocarditis, then it is appropriate to provide prophylaxis with antibiotics before dental treatment if significant bleeding is anticipated. Substance-abusing patients are vulnerable to sexually transmitted diseases (STDs) because of both their altered immune response and their high-risk behaviors. Patients with alcohol and other substance abuse problems often sacrifice balanced nutritional intake for the sake of maintaining their addictions. Craving to feed their “habit,” limited discretionary money (beyond the cost of the habit), and altered mental judgment all contribute to poor nutrition. Folic acid and thiamine deficiencies are common. As a result of poor dietary habits, anemia and malnutrition may occur with the attendant problems of a depressed immune response; poor wound healing, and persistent local or systemic infection.
Substance-abusing patients in general and patients with alcoholism in particular are also more prone to develop fulminant systemic infection. It has been recognized that bacterial infections are more serious in patients with alcoholic liver disease—sometimes with fatal consequences. The dentist must be cognizant of the fact that oral surgical procedures, sites of oral infection or trauma, and periodontal diseases may all function as a nidus of infection and possible source of septicemia. The use of topical antimicrobials before oral surgery, scaling, or other invasive procedures is prudent in the substance-dependent patient. For high-risk patients—for example, those with confirmed compromised immune systems—systemic antibiotics may also be warranted. In general, however, in the absence of ongoing infection, studies have not shown that systemic antibiotic prophylaxis is warranted before invasive dental procedures.
Psychological issues
Substance-abusing patients may develop profound psychological effects, including cognitive impairment, anxiety disorders, antisocial behavior, and affective disorders. In severe cases, permanent neurologic damage may occur, and these patients may develop alcohol amnestic disorder, rendering them unable to recall previously known material or learn new material. Patients may also have alcohol-related blackouts, and some individuals may develop dementia and/or severe personality changes. In such cases, professional psychiatric support is required and the dental treatment plan may need to be significantly curtailed.
Alcohol abuse–related disorders
Alcohol, when consumed in moderation, is recognized to have cardiovascular and other health benefits. Light to moderate alcohol consumption (one drink daily for women and one or two drinks daily for men) is associated with cardioprotective benefits. The concentration of alcohol in a beverage is usually stated as the percentage of alcohol by volume (ABV; the number of milliliters of pure ethanol in 100 mL of beverage) or as proof . In the United States, a standard drink contains 0.6 ounces (18 mL) of alcohol. This is approximately the amount of alcohol in a 12-ounce (350 mL) glass of beer (5% ABV), a 5-ounce (150 mL) glass of wine (12% ABV), or a 1.5-ounce (44 mL) glass of a 40% ABV (80 proof) “hard” liquor or spirits. In the United States, proof is twice the percentage of alcohol by volume at 60 degrees Fahrenheit (e.g., 80 proof = 40% ABV).
Research shows that individuals who drink moderately may be less likely to develop an alcohol use disorder (AUD). The definition of “moderate” differs for men and women. Moderate alcohol consumption for men has been defined as no more than four drinks on any single day and no more than 14 drinks per week. For women, no more than three drinks on any single day and no more than seven drinks per week is held to be moderate consumption. To stay at low risk for AUDs, individuals must keep within both the single-day and weekly limits.
An individual who has consumed one or two alcoholic drinks often feels more energetic and outgoing. This stimulating effect is actually a disinhibiting of personality. Instead of functioning as a stimulant, alcohol is actually a CNS depressant. Alcohol consumption slows normal brain function, with the sedating effect increasing with increasing amounts of alcohol. In higher doses, alcohol can become a general anesthetic. Tranquilizers and sedatives are also CNS depressants.
A healthy dental patient who consumes a limited amount of alcohol typically presents no limitation or contraindications to dental treatment. Patients who use alcohol to excess, or patients who often use mind-altering substances, however, may have problems accepting, receiving, or completing dental treatment. Significant behavioral and medical issues can arise with the substance-abusing patient and may necessitate significant modification to the dental treatment plan. In some cases, treatment may need to be deferred, limited in complexity, or sequenced differently than for the normal patient.
Prevalence of alcohol abuse.
Excessive use of alcohol (defined as use that causes damage to health) results in the death of 2.5 million people annually worldwide, causes illness and injury to millions more, and increasingly affects younger generations of drinkers in developing countries. In the United States, alcohol is the most commonly used addictive substance, and its abuse has been identified as the number-one drug problem. It is estimated that 17.6 million people, or one in every 12 adults, meet the diagnostic criteria for AUD. Several million more engage in risky drinking patterns that could lead to alcohol problems.
The National Institute on Alcohol Abuse and Alcoholism reports that more than one-half of all adults have a family history of alcoholism or problem drinking, and that more than seven million children live in a household in which at least one parent is dependent or has abused alcohol. AUD can be found in individuals of any race, gender, age, or socioeconomic group. , Approximately 88,000 deaths are attributable to excessive alcohol use each year in the United States, making excessive alcohol use the third-leading lifestyle-related cause of death. , Excessive alcohol use may reduce an individual’s life expectancy by up to 30 years. In 2006, more than 1.2 million emergency room visits and 2.7 million physician office visits in the United States were attributed to excessive drinking. In total, alcohol alone or in combination with other drugs, such as benzodiazepines, is estimated to be responsible for more overdose deaths in the United States than any other agent. Alcohol is the world’s third-largest risk factor for disease burden; it is the leading risk factor in the Western Pacific and the Americas and the second largest in Europe.
Approximately one-half of all individuals who are diagnosed with alcohol abuse or dependence have additional psychiatric illnesses. These patients are said to have a “dual diagnosis.” Additional illnesses may include anxiety, bipolar, antisocial personality, or major depressive disorders. Although these patients are treated for and receive psychiatric medications for their diagnoses, they are unlikely to abstain from alcohol use and are at greater risk for experiencing alcohol-associated morbidity and mortality. It is common for alcoholics to have multiple addictions, which may include abuse of, or dependence on, other substances such as cocaine and nicotine.
AUD is often associated with problems similar to those associated with other abused substances (e.g., cannabis, cocaine, heroin, amphetamines, sedatives, hypnotics, or anxiolytics). Alcohol may be used to alleviate the unwanted effects of other abused substances or to substitute for them when they are not available. Symptoms such as behavior problems, depression, anxiety, and insomnia frequently accompany heavy drinking and sometimes precede it. Once a pattern of repetitive and intense use develops, individuals with AUD may devote substantial periods of time to obtaining and consuming alcoholic beverages.
Owing to the extremely unpleasant symptoms experienced during withdrawal, individuals may continue to consume alcohol despite adverse consequences, simply to avoid or relieve withdrawal symptoms. Some withdrawal symptoms (e.g., sleep problems) can persist at lower intensities for months and may contribute to relapse. ![]() See Diagnostic Criteria for Alcohol-Related Disorders.
See Diagnostic Criteria for Alcohol-Related Disorders.
Pathophysiology of high alcohol use.
Repeated intake of high doses of alcohol may affect nearly every organ system and, in particular, the gastrointestinal tract, cardiovascular system, and central and peripheral nervous systems. Gastrointestinal effects include gastritis, stomach or duodenal ulcers, and, in approximately 15% of individuals who use alcohol heavily, cirrhosis and/or pancreatitis. Alcohol abusers experience an increased rate of cancer of the esophagus, stomach, and other parts of the gastrointestinal tract.
Excessive alcohol ingestion may also damage cardiac muscle tissue, affecting myocardial contractility with resulting cardiomyopathy and congestive heart failure. These factors, along with marked increases in levels of triglycerides and low-density lipoprotein cholesterol, contribute to an elevated risk of heart disease. A common problem is development of low-grade hypertension that, in combination with increased levels of cholesterol, fosters an elevated risk of cerebrovascular and coronary artery disease.
Peripheral neuropathy may also be seen in individuals who use alcohol heavily as evidenced by muscular weakness, paresthesias, and decreased peripheral sensation. More persistent CNS effects include degenerative changes in the cerebellum, cognitive deficits, and severe memory impairment. These effects are related to the direct effects of alcohol or associated trauma and to vitamin deficiencies, particularly the B vitamins, including thiamine.
Alcohol abuse frequently results in inadequate nutritional intake. Because alcohol ingestion often accounts for one-half of the daily caloric intake, it displaces dietary proteins, minerals, and trace elements such as magnesium and zinc. To compound this problem, chronic alcohol ingestion also causes malabsorption of folic acid, B-complex vitamins; thiamine (B1), riboflavin (B2), pyridoxine (B6), extrinsic factor (B12), and vitamins D, E, and K.
Alcohol abuse has a deleterious effect on neural development. Acetylcholine and dopamine receptors are damaged, leading to motor and sensory disturbances. In the CNS, neuronal cell death and atrophy of several regions of the brain occur. Clinically, these anatomic changes correlate with deficits in judgment and decision-making ability, reduced attention span, short-term memory loss, reduced emotional stability, and impaired coordination.
Any alcohol-dependent individual may develop these psychological conditions, along with concomitant cognitive impairment. In severe cases, neurologic damage may be permanent, predisposing the individual to alcohol amnestic disorder, which prevents the recall of previously known material and impairs the ability to learn and process new information. Alcoholic individuals have a propensity to develop depression due to the CNS effects from long-term alcohol abuse and may have alcohol-related blackouts or develop dementia and severe personality changes.
Other adverse effects of long-term alcohol abuse include impairment of the liver’s ability to produce coagulation factors and metabolize medications, impairment of white blood cells’ chemotactic abilities, and impairment of the bone marrow’s production of platelets. The first changes in alcoholic liver disease are fatty infiltration of hepatocytes. The hepatocytes become engorged with fatty lobules, creating enlargement of the liver. This process is usually reversible. , Prolonged alcohol abuse leads to fatty liver, alcoholic hepatitis, and cirrhosis.
Alcoholic hepatitis, a more serious form of liver disease, is characterized by a widespread inflammatory condition and cellular destruction. This condition may be irreversible, leading to necrosis, sometimes resulting in death if the damage is widespread. The clinical presentation of alcoholic hepatitis includes nausea, vomiting, anorexia, malaise, weight loss, and fever. ,
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


