-
Chapter outline
-
Rationale for Including a Maintenance Phase in the Treatment Plan
-
Issues Typically Included in the Maintenance Phase
![]()
After completion of definitive phase therapy, there will be remaining issues that must be addressed and previously rendered treatment that must be reevaluated. Some of these concerns will need attention for as long as the dentist-patient therapeutic relationship exists. In addition to their importance to patient care, good maintenance phase plans provide the patient-specific elements essential to the development of an organized, practice-wide system of periodic care that serves as the backbone of a successful and productive dental practice.
Although this aspect of the treatment plan may seem less important at the outset, the maintenance phase represents a critical component of any complex treatment plan. In many cases, the long-term success or failure of the plan depends on it. As this chapter unfolds, it will become clear why the dentist should discuss long-term periodic care with the comprehensive care patient. Furthermore, the rationale for initiating this discussion at the time that the original treatment plan is presented will also become apparent.
Prevention of future problems is, of course, the guiding principle of the maintenance phase. The astute practitioner works throughout all phases of treatment to educate the patient in strategies for maintaining a healthy oral condition and preventing future oral disease. Certain aspects of a systemic phase may include activities that are preventive in nature. The acute phase may include treatment that has the effect of preventing disease progression. The disease control phase, by its nature, is preventive in orientation, and numerous references to preventive therapies are made in Chapter 9 . Nevertheless, significant patient education and the reinforcement of earlier oral homecare instruction will occur primarily during maintenance phase visits. For that reason, preventive concepts and preventive therapy are emphasized in this chapter. The reader is reminded that it would be shortsighted and inappropriate for the practitioner to make prevention primarily the responsibility of the hygienist and to address it solely in the maintenance phase. Prevention must be the responsibility of the entire dental team and must be carried out throughout the treatment process.
The maintenance phase must be flexible and individualized, with timing and content specifically tailored to each patient’s needs. Although formulated at the treatment planning stage, it will have been modified during the disease control and definitive treatment phases and will take its final form at the posttreatment assessment, which is discussed in the following section. The dentist implements maintenance phase care through the periodic visit (discussed in section, Recall Visit ). The terms periodic visit or recare visit are used interchangeably with recall visit. The American Dental Association (ADA)–sanctioned procedure coding system uses the designation periodic oral evaluation . Consistent with that perspective, the terms periodic examination and periodic visit are used in this text.
Posttreatment assessment
The posttreatment assessment is a dedicated, structured appointment scheduled at the conclusion of the disease control phase of treatment, if the original plan includes disease control, and at the conclusion of the definitive phase. The purposes of the assessment are to evaluate the patient’s response to treatment, comprehensively assess current oral health status, determine any new treatment needs, and develop a specific plan for future treatment. If accomplished during the first periodic evaluation and visit, the posttreatment assessment will include oral health instruction, selected scaling as needed, and oral prophylaxis.
Most colleges of dentistry have developed a formalized process for the clinical examination that will be made when the patient is about to exit the patient care program. The following discussion uses one such system as an example. Because each practice or institution will have unique needs, the decision regarding development of a posttreatment assessment protocol will be made on an individual basis. Whatever mechanism the dentist decides on, the emphasis will be on the importance of engaging the patient in a comprehensive reevaluation and reassessment at the conclusion of the disease control phase of treatment and/or at the conclusion of the entire plan of care. Many practitioners prefer not to formalize this process, declining to take the time to develop a specific protocol or form for recording findings. Certainly the current standard of care in practice does not dictate a mandatory posttreatment assessment protocol. The standard of care does require, however, that patients be provided maintenance services and continuity of care. In that context, the concepts described here should have application to any practice. Each practitioner is encouraged to incorporate some type of patient maintenance program into the office policy manual and to implement use of that program with each patient. The information included here can be used as a guide for that purpose.
Objectives for the posttreatment assessment
The purpose and intent of the posttreatment assessment is to enable the practitioner to evaluate the following:
- •
The patient’s current oral condition
- •
Outcomes of treatment rendered by the dental team
- •
The patient’s satisfaction with the care that has been provided
- •
Present and future treatment needs of the patient
The posttreatment assessment provides a foundation for planning any additional treatment and maintenance therapy that the patient will need.
Elements of the posttreatment assessment
Items to be included in the posttreatment assessment and recorded in the patient record will vary with the nature and scope of the dental practice, the individual patient profile, and the patient’s need. Typical elements in a posttreatment assessment include the following:
- •
Update of the general health history and review of systems
- •
Recording vital signs
- •
A head/face/neck examination to reassess any previously diagnosed conditions and to determine whether any new oral pathology is present
- •
Updating radiographs according to the practice or institutional protocol and the patient’s individual need
- •
Evaluation of the alignment of the teeth and jaws, the occlusion, the temporomandibular joint, and the patient’s ability to speak, chew, and function
- •
Assessment of all periapical areas, with particular focus on teeth that have received root canal therapy
- •
Comprehensive periodontal assessment and periodontal risk assessment
- •
Evaluate adherence to homecare advisories, reinforce oral homecare instructions
- •
Evaluation of all existing restorations and prostheses
- •
Comprehensive caries diagnosis and caries risk assessment
- •
Statement describing the patient’s satisfaction (or dissatisfaction) with the treatment rendered; were all the patient’s expectations met?
- •
Summary of the patient’s response to treatment; was the patient adherent with attendance and professional recommendations?
- •
Description of any remaining restorative needs and how those needs will be addressed
- •
Specific plan to address any other ongoing or emerging issues that will need future attention
- •
Provide preventive and therapeutic product recommendations
- •
Establish an appropriate recall interval
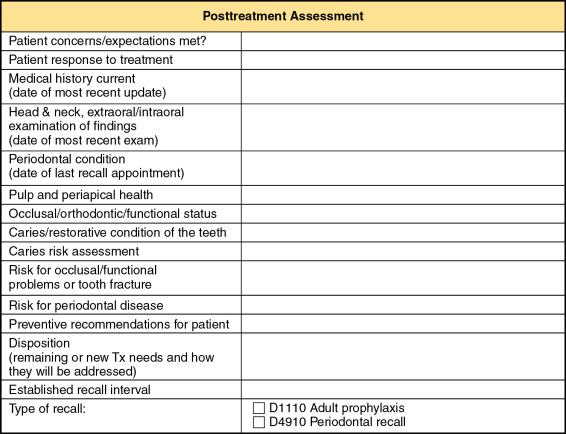
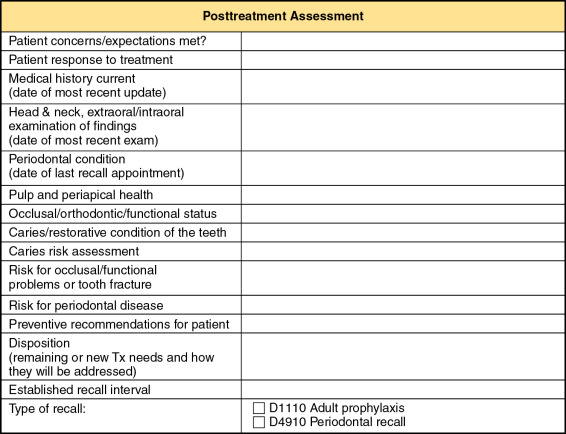
Documenting the posttreatment assessment
The posttreatment assessment may be documented in the progress notes in a narrative or bullet format, with or without a predetermined outline to guide the process. If the practice has multiple providers, a common outline or format should be developed for consistency and efficiency. In an institutional setting, it is usually advantageous to develop a form specifically for that purpose ( Figure 11-1 ).
Posttreatment assessment
The posttreatment assessment is a dedicated, structured appointment scheduled at the conclusion of the disease control phase of treatment, if the original plan includes disease control, and at the conclusion of the definitive phase. The purposes of the assessment are to evaluate the patient’s response to treatment, comprehensively assess current oral health status, determine any new treatment needs, and develop a specific plan for future treatment. If accomplished during the first periodic evaluation and visit, the posttreatment assessment will include oral health instruction, selected scaling as needed, and oral prophylaxis.
Most colleges of dentistry have developed a formalized process for the clinical examination that will be made when the patient is about to exit the patient care program. The following discussion uses one such system as an example. Because each practice or institution will have unique needs, the decision regarding development of a posttreatment assessment protocol will be made on an individual basis. Whatever mechanism the dentist decides on, the emphasis will be on the importance of engaging the patient in a comprehensive reevaluation and reassessment at the conclusion of the disease control phase of treatment and/or at the conclusion of the entire plan of care. Many practitioners prefer not to formalize this process, declining to take the time to develop a specific protocol or form for recording findings. Certainly the current standard of care in practice does not dictate a mandatory posttreatment assessment protocol. The standard of care does require, however, that patients be provided maintenance services and continuity of care. In that context, the concepts described here should have application to any practice. Each practitioner is encouraged to incorporate some type of patient maintenance program into the office policy manual and to implement use of that program with each patient. The information included here can be used as a guide for that purpose.
Objectives for the posttreatment assessment
The purpose and intent of the posttreatment assessment is to enable the practitioner to evaluate the following:
- •
The patient’s current oral condition
- •
Outcomes of treatment rendered by the dental team
- •
The patient’s satisfaction with the care that has been provided
- •
Present and future treatment needs of the patient
The posttreatment assessment provides a foundation for planning any additional treatment and maintenance therapy that the patient will need.
Elements of the posttreatment assessment
Items to be included in the posttreatment assessment and recorded in the patient record will vary with the nature and scope of the dental practice, the individual patient profile, and the patient’s need. Typical elements in a posttreatment assessment include the following:
- •
Update of the general health history and review of systems
- •
Recording vital signs
- •
A head/face/neck examination to reassess any previously diagnosed conditions and to determine whether any new oral pathology is present
- •
Updating radiographs according to the practice or institutional protocol and the patient’s individual need
- •
Evaluation of the alignment of the teeth and jaws, the occlusion, the temporomandibular joint, and the patient’s ability to speak, chew, and function
- •
Assessment of all periapical areas, with particular focus on teeth that have received root canal therapy
- •
Comprehensive periodontal assessment and periodontal risk assessment
- •
Evaluate adherence to homecare advisories, reinforce oral homecare instructions
- •
Evaluation of all existing restorations and prostheses
- •
Comprehensive caries diagnosis and caries risk assessment
- •
Statement describing the patient’s satisfaction (or dissatisfaction) with the treatment rendered; were all the patient’s expectations met?
- •
Summary of the patient’s response to treatment; was the patient adherent with attendance and professional recommendations?
- •
Description of any remaining restorative needs and how those needs will be addressed
- •
Specific plan to address any other ongoing or emerging issues that will need future attention
- •
Provide preventive and therapeutic product recommendations
- •
Establish an appropriate recall interval
Documenting the posttreatment assessment
The posttreatment assessment may be documented in the progress notes in a narrative or bullet format, with or without a predetermined outline to guide the process. If the practice has multiple providers, a common outline or format should be developed for consistency and efficiency. In an institutional setting, it is usually advantageous to develop a form specifically for that purpose ( Figure 11-1 ).
Rationale for including a maintenance phase in the treatment plan
The primary purpose of the maintenance phase is to ensure long-term oral health, optimum function, and favorable esthetics for the patient. In the maintenance phase, continuing systemic issues can be managed, disease control measures can be reevaluated and strengthened, and restorations and prostheses can be repaired, cleaned, polished, recontoured, or relined as needed. Success or failure of previous treatment must be reassessed and any necessary additional treatment planned. Multiple benefits derive from a comprehensive and strategically crafted plan for the maintenance phase. These benefits can be clustered into three categories: (1) issues that remain unresolved at the close of the definitive phase of treatment, (2) patient-based issues, and (3) practice management issues.
Address ongoing patient needs
Follow-up of untreated diagnoses
At the conclusion of the definitive treatment phase, previously diagnosed but untreated conditions may require reevaluation. These might include reactive soft tissue lesions, asymptomatic chronic bone lesions, defective but not problematic restorations, or teeth with incipient carious lesions. The maintenance phase provides an ideal time to reassess these issues, discuss them with the patient, and develop consensus on how to manage them going forward.
Monitoring chronic conditions that can affect oral health
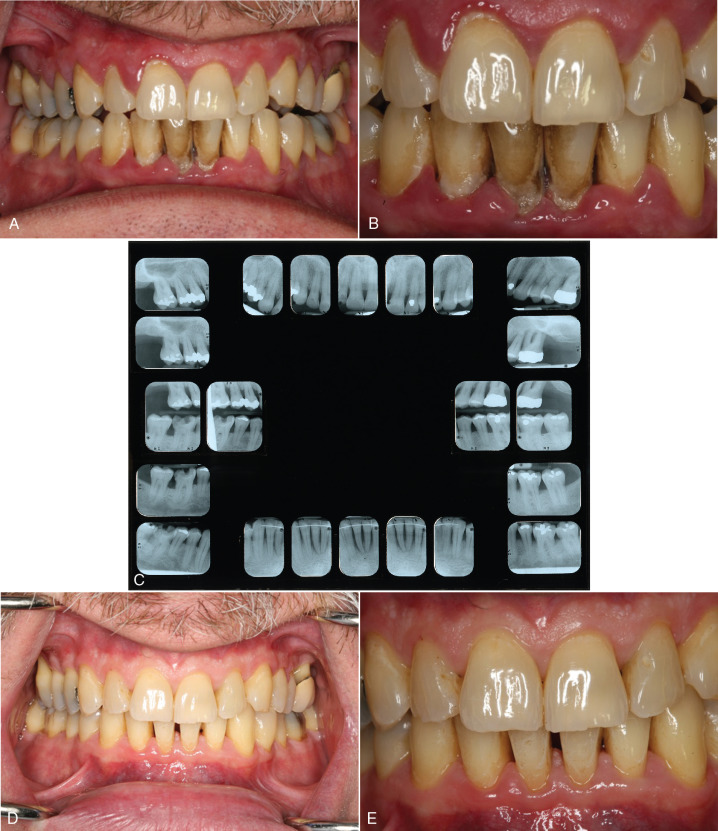
Patients may have systemic diseases that influence plans for or the delivery of dental treatment (e.g., diabetes), systemic diseases with significant oral manifestations (e.g., Sjögren’s syndrome , or chronic oral diseases (e.g., periodontal disease). The maintenance phase provides an opportunity to reassess such chronic conditions, determine whether new intervention or retreatment is warranted, and address any new sequelae or related conditions that may have arisen since the last appointment ( Figure 11-2 ).
Revisiting elective treatment issues
Earlier in the course of treatment, patients may have raised dental concerns or aspirations that for various reasons (e.g., time, finances, anxiety) they chose to defer. Similarly, the patient may have earlier declined certain elective treatments that the dentist recommended, such as removal of asymptomatic third molars or replacement of missing teeth. The maintenance phase provides an ideal opportunity to revisit these issues.
Patient centered benefits
Rapport building
Patients return to their dentist for periodic care for many reasons beyond the obvious recommended scaling and oral prophylaxis. The importance of the professional trust and faith that patients place in their dental team and the personal security obtained from the relationship should not be underestimated or taken for granted. Consciously or unconsciously, most patients have a strong expectation that their dentist is diligently looking out for their best interests and will do what is best to promote and ensure their oral health. Periodic visits do much to cement the relationship and fulfill the patient’s expectations.
Patient education
The maintenance phase serves as an effective instrument to educate and motivate the patient, and helps maintain the patient’s awareness of the importance of continuing attention to oral health. As the dentist plans the maintenance phase and shares that information with the patient, the patient has the opportunity to learn about the nature and importance of this aspect of the plan of care and to raise questions about it. As the dentist explains the need for maintenance therapy and the ways in which the periodic visits form an integrated part of the overall plan of care, the patient comes to appreciate the ways in which this phase of treatment will affect his or her future oral health.
More specifically, discussing the maintenance phase helps educate the patient about the details of care provided during the periodic visits and the patient’s own contribution to maintaining a healthy oral condition. This is the ideal opportunity to inform the patient about oral homecare practices that will help preserve restorations and prostheses, maintain a disease-free environment, and prevent future problems. Oral healthcare suggestions may be given to the patient orally or in written form (e.g., using pamphlets or audiovisual materials), or both.
Writing the maintenance phase into the treatment plan reminds the patient of its presence and importance each time he or she picks up a copy of the plan of care. It also reminds the patient of specific tasks and expectations that are his or her responsibility. That knowledge becomes a powerful tool for the dentist in ongoing efforts to instill in the patient a sense of responsibility and confirming to the patient the value of maintaining a long-term therapeutic relationship.
Emphasis on individualized care
Although patients may be unsophisticated in their understanding of dental disease or the finer elements of dental treatment, they quickly develop a sense of how a dental practice functions and share that information with their friends and neighbors. Patients may more easily characterize office policy concerning periodic visits than the dentist can. Is the standard simply a routine “6 months’ checkup and cleaning”? Or is there an individually planned interval with a specified structure tailored to the needs of the individual patient? In the all-too-common first situation, patients may gain the impression that production, rather than individualized patient care, is the motivating influence.
Individualized patient care communicates the fact that the dentist focuses treatment on each individual patient, targeting specific needs by using risk assessment, social and dental history, and other data that can affect oral health. Taking time to carefully create individualized recommendations shows the patient that the dental team is invested in each patient’s personal and oral health and instills a greater level of trust and respect. The benefits to the patient include more meaningful homecare routines and treatment recommendations that provide a foundation for a more successful outcome. Additionally, by tailoring treatment and preventive recommendations to the needs of each individual, rather than relying on a single lock-step approach, the patient gains a sense of ownership and responsibility for his or her own care and will be more likely to be adherent to professional recommendations.
Health promotion and disease prevention
Because the well-constructed maintenance phase places the emphasis on promoting and sustaining optimal oral health and function, rather than on restoration and reconstruction resulting from past disease, this phase makes clear the role of dentistry as a healthcare profession. This approach encourages the patient to adopt a regular schedule for visiting the dentist, rather than simply waiting for a problem to develop.
Anticipating further treatment needs
A thoughtful, comprehensive maintenance phase plan includes any issues that can realistically be expected to require reevaluation, reconsideration, or retreatment in the future. Specific notes, such as “reevaluate tooth #29 with poor periodontal prognosis” or “reassess patient need and/or desire for crown on tooth #19 with compromised cusp integrity” confirm that the patient has been alerted to potential risks and hazards and clearly puts the responsibility for accepting the consequences of deferring treatment on the patient rather than the dentist. A casual review of the original treatment plan (or progress note if recorded there) can facilitate bringing the issue to the patient’s attention again.
Without a clearly articulated maintenance phase, the patient may assume that any new problems that arise are, at least in part, the responsibility of the dentist. The tooth with longstanding severe periodontitis that must now be extracted, or the tooth with a large amalgam restoration that now fractures, are examples. Recording these potential problems in the treatment plan and calling them to the patient’s attention at the outset of the maintenance phase minimizes the opportunity for future misunderstanding, mistrust, or conflict.
Taking the time to develop and carry out a comprehensive and individualized maintenance phase for each patient ensures good patient care and can provide enormous benefits to the dentist, staff, and practice.
Practice management benefits
Professional competence
Collectively, the entire patient record—if it includes a comprehensive, accurate, and complete database, diagnosis, plan of care, and consent—provides excellent evidence of professional competence. A thorough, well-written maintenance phase, although not indispensable in this regard, certainly contributes to a positive view of professional competence and may help discourage a disgruntled patient from pursuing litigation.
Efficient delivery of care
A well-written maintenance phase plan of care can be used as an effective tool to alert office staff, dental assistants, hygienists, and the dentist to the particular systemic or oral health issues or other concerns that should be addressed during periodic visits. Awareness of such issues and concerns at the outset makes the visit more focused, efficient, and personalized. The patient’s individual needs can be addressed immediately, without requiring the dentist to sort through the chart, looking at multiple progress notes to reconstruct the history. With a recorded plan, the entire staff approaches the periodic visit proactively and efficiently.
Reducing patient emergencies
An informed patient who expects and anticipates problems is more likely to take preventive action before a crisis develops, less likely to need emergency care, more apt to have a realistic understanding of a problem (and be able to discuss it rationally), and more apt to accept recommended treatment. For the dentist and the staff, this translates into fewer interruptions, less anxiety for the patient, reduced staff stress, and smoother patient flow. Such a practice usually provides a more patient-friendly and rewarding setting in which to work.
Partnering with patients
The maintenance plan encourages the patient to become a partner in the long-term management of his or her oral health, rather than simply a consumer of dental goods and services. The maintenance phase, by design and necessity, engages the patient in the process. Although many patients remain quite comfortable in the conventional model of dental care, in which the dentist makes all the decisions, such an approach places all the responsibility for the success of treatment on the shoulders of the dentist, fostering an overly dependent patient-dentist relationship. The maintenance phase provides an effective way to appropriately delineate roles and responsibilities for maintaining the patient’s long-term oral health.
Issues typically included in the maintenance phase
To list all the items that could be included in the maintenance phase would be a large undertaking. To give the reader a realistic perspective on this issue, the authors suggest the following categories that might be included. Although not all inclusive, the list is representative and may serve as a menu or template from which each practitioner may begin to develop a selection list appropriate for his or her own practice. Although no individual patient would be expected to require attention to all of the areas listed here, it can be anticipated that most patients will need several.
General health considerations
Specify all items from the systemic phase that will require follow-up, reevaluation, or intervention as part of the patient’s long-term care. Examples include physician consultation in the presence of chronic life-threatening disease, such as liver cancer, premedication for anxiety or infective endocarditis, reevaluation of previously diagnosed hypertension or other chronic conditions, and treatment modification because of an immunocompromising condition, such as rheumatoid arthritis.
Oral homecare instructions
Oral homecare instructions play a vital role in the long-term success of a patient’s oral health and the overall success of the maintenance phase. As an integral aspect of the individualized patent care plan, homecare instructions should be thoughtfully developed and based on the status of the dentition, the history of restorations, any periodontal or caries risk, and the anticipated level of patient adherence. Take into account areas that may be susceptible to trapping plaque, such as open contacts, extensive restorative work, and periodontal defects. The dentist must consider oral physiotherapy aids specific to the patient’s needs, such as an end-tuft brush for a third molar area or a floss threader for bridgework. Additional preventive and therapeutic agents, such as prescription-level dentifrices and antibacterial mouth rinses, should be considered and recommended as needed. Document all recommendations and instructions made to the patient, including any prescribed oral physiotherapy aids, materials, and techniques, and the advisable frequency of visits. If particular attention is necessary in specific areas, possibly with adjunctive aids such as floss threaders or proximal brushes, this should be noted as well ( Figure 11-3 and Table 11-1 ). Documentation should also include patient questions about the oral homecare instructions, particularly if the issues need to be revisited.

| Oral Physiotherapy Aid | Indications for Use |
|---|---|
| Dental floss and tape | Proximal surfaces |
| Tufted dental floss | Wide embrasure spaces, orthodontic appliances, abutments, under pontics |
| Floss holder | Patients with limited dexterity |
| Floss threader | Orthodontic appliances, under fixed prostheses |
| Interdental brush | Wide embrasure spaces, orthodontic appliances, fixed prostheses, dental implants, periodontal splints, space maintainers, exposed furcations |
| End-tuft brush | Fixed prostheses, wide embrasure spaces, distal surfaces of most posterior teeth |
| Interdental rubber tip | Gingival margin, embrasure spaces, exposed furcations |
| Toothpick (with holder) | Gingival margin, orthodontic appliances, exposed furcations |
Oral prophylaxis
Specify frequency, any areas that need special attention, and any particular products, instruments, or techniques to be used by the dental team. The appropriate type of recall appointment should also be determined. If a patient has had a diagnosis of and initial therapy for periodontal disease, then the appropriate type of recall appointment would be a periodontal maintenance visit. Otherwise, for the patient seeking preventive care, the recall would be designated as an adult prophylaxis. Also, it should be noted if the patient has a particular preference or objection to specific agents, such as a flavored prophy paste or any element in the armamentaria, such as the air-powder polisher.
Caries control
This aspect of the maintenance phase plan is a continuation of the caries management plan described at length in Chapter 9
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


