Oculo-facio-cardio-dental (OFCD) syndrome is a rare syndrome characterized by ocular, facial, cardiac, and dental disorders. Only about 20 cases have been reported to date. The most prominent of the various features of this syndrome is canine radiculomegaly. Other features include a long and narrow face, a high nasal bridge, a broad and pointed nose, a bifid nose, ear deformity, cleft palate or submucous cleft palate, maxillary growth retardation, a large gonial angle, open apices, delayed eruption, persistent deciduous teeth, extreme overbite, and constricted maxilla. Orthodontic and prosthodontic treatment has been reported for several patients, but surgical-orthodontic treatment for OFCD has not been reported. An 18-year-old woman with skeletal Class III malocclusion and OFCD syndrome was treated with edgewise appliance therapy combined with orthognathic surgery. We applied a light force during the treatment so as not to induce ankylosis. At the end of the surgical and orthodontic treatments, functional occlusion and an improved facial profile were achieved. After the retention period, stomatognathic function was improved. The results of this treatment suggest that surgical-orthodontic treatment is an effective method for improving skeletal disharmony, facial profile, occlusion, and stomatognathic function in patients with OFCD.
Oculo-facio-cardio-dental (OFCD) syndrome is characterized by ocular, facial, cardiac, and dental disorders, and was first reported by Hayward in 1980. OFCD syndrome is an X-linked dominant trait, and it might be lethal in males. This syndrome is rare, and only 20 cases have been reported to date. Several specific features are observed in skeletal and dental conditions, with canine radiculomegaly the most prominent feature. Additionally, facial and skeletal anomalies, such as a long and narrow face, a high nasal bridge, a broad and pointed nose, a bifid nose, ear deformity, cleft palate or submucous cleft palate, maxillary growth retardation, and a large gonial angle, have been reported. Among the dental anomalies, open apices, delayed eruptions, persistent deciduous teeth, extreme overbite, and a constricted maxilla have been reported. For improvement of these anomalies, orthodontic and prosthodontic treatments have been performed in a few cases. However, surgical orthodontic correction in OFCD patients has not been reported. We had an opportunity to treat a patient with OFCD syndrome with surgical-orthodontic treatment. In this report, we demonstrate and discuss the effectiveness of surgical-orthodontic treatment in this patient.
Diagnosis and etiology
The patient, an 19-year-old woman with chief complaints of severe anterior crossbite and mandibular protrusion, was referred to the orthodontic department of Kagoshima University Hospital in Japan. She was the first-born twin, delivered via a normal delivery with a normal gestational age. Birth weight and height were 2300 g and 44 cm, respectively. The other twin was a boy who exhibited none of her symptoms. The patient also had a younger sister, who had no appreciable disease. Her father had a history of tuberculosis, and her mother had polio. She had congenital cataracts at birth that were followed up at the university hospital. At age 6 years, she had hematuria syndrome, which was also followed up. She had retinal detachment surgery at ages 11 and 13. She had normal intelligence. No DNA sample was obtained.
Her facial profile was concave with chin protrusion and a long lower facial height ( Fig 1 ). The facial photographs showed a slightly asymmetric face, a high nasal bridge, and a broad-tipped nose. The intraoral examination showed an Angle Class III molar relationship with overjet of −5.3 mm, overbite of 13.4 mm, and a constricted maxillary dental arch ( Fig 1 ). Maxillary diastema, abnormal shape of the maxillary central incisors, microdontia in the maxillary right lateral incisor, and a high arched palate were also observed. Enamel dysplasia was also seen in both maxillary central incisors, and the mandibular left central incisor, left canine, and left first premolar. The maxillary dentition was severely crowded, with an arch-length discrepancy of −13.0 mm, but the mandibular dentition was spaced with arch length of +8.5 mm ( Fig 2 ). The Bolton analysis showed an anterior ratio of 64.86% (mean ± SD: 91.37 ± 2.1%) and an overall ratio of 78.9% (mean ± SD: 78.09 ± 2.19%) because of the congenital absence of the mandibular left central incisor and the malformation of several teeth. The panoramic radiograph ( Fig 3 ) confirmed the congenital absence of the left central incisor in the mandibular arch. Both canines and first premolars in both dental arches had excessively long roots, and the apices of these teeth showed delayed closure. The mandibular third molars were developed, but the spaces for their eruption were insufficient.

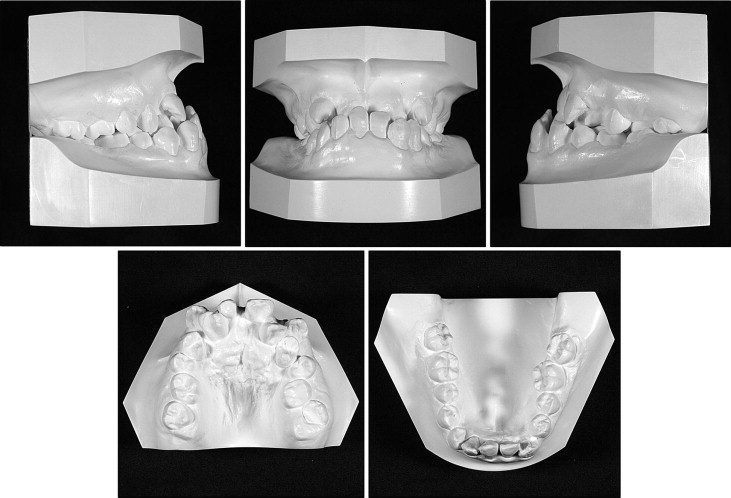
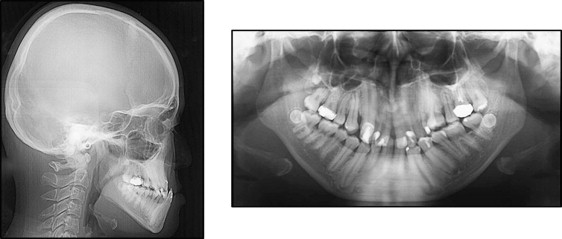
The lateral cephalometric analysis ( Fig 3 , Table ) showed a skeletal Class III jaw relationship with severe mandibular protrusion (ANB, −3.4°; SNB, 85.4°). The mandibular plane to Frankfort horizontal plane angle and the gonial angle were within a range of +1 SD of the Japanese normative mean. The maxillary and mandibular incisors exhibited lingual inclination (U1-FH, 107.0°; L1-FH, 73.5°).
| Measurement | Pretreatment (19 y 2 mo) | Posttreatment (22 y 2 mo) | Two-year postretention (26 y 2 mo) | Normative value ∗ | |
|---|---|---|---|---|---|
| Mean | SD | ||||
| Angular measurements (°) | |||||
| ANB | −3.4 | 3.3 | 3.2 | 2.8 | 2.4 |
| SNA | 82.0 | 82.0 | 82.1 | 80.8 | 3.6 |
| SNB | 85.4 | 78.7 | 78.9 | 77.9 | 4.5 |
| MP-FH | 31.7 | 39.0 | 36.9 | 30.5 | 3.6 |
| Gonial angle | 130.2 | 141.8 | 135.1 | 122.1 | 5.3 |
| U1-FH | 107.0 | 117.7 | 111.9 | 112.3 | 8.3 |
| L1-FH | 73.5 | 63.5 | 61.6 | 56.0 | 8.1 |
| Linear measurements (mm) | |||||
| Ar-Go | 50.6 | 43.4 | 48.6 | 47.3 | 3.3 |
| Go-Me | 77.1 | 68.6 | 68.5 | 71.4 | 4.1 |
| Overjet | −5.3 | 3.8 | 3.1 | 1.0 | 1.5 |
| Overbite | 13.4 | 0.5 | 0.6 | 1.0 | 1.5 |
| U1-A-Pog | 0.7 | 7.7 | 6.3 | 5.0 | 1.5 |
| L1-A-Pog | 8.5 | 3.9 | 3.8 | 3.0 | 1.5 |
| Subnasale-Gn | 80.0 | 71.0 | 71.0 | 72.0 | 6.0 |
| G-Sn/Sn-MeS † | 0.9 | 1.0 | 0.9 | 1.2 | 1.0 |
| Upper lip to E-line | −5.1 | −1.9 | −1.1 | −3.0 | 1.0 |
| Lower lip to E-line | 3.7 | 0.8 | 0.9 | −0.1 | 2.5 |
∗ Means and standard deviations of normally developed Japanese female adults
The soft-tissue analysis showed that the upper lip was 5.1 mm behind and the lower lip was 3.7 mm forward relative to the E-line, with a lower facial height ratio of 0.9 in G-Sn/Sn-soft tissue menton at the resting position.
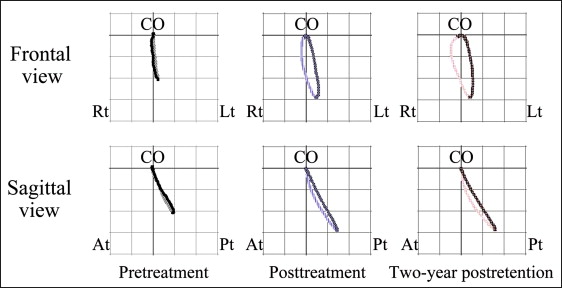
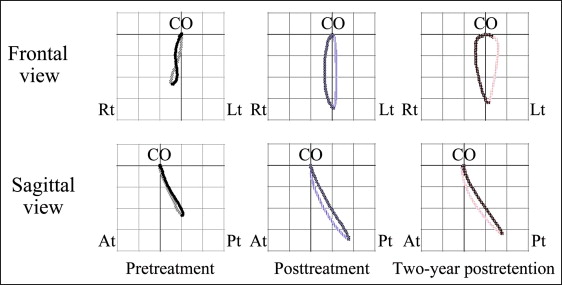
The jaw movement during gummy jelly chewing was examined by an optoelectric jaw-tracking system with 6 degrees of freedom; it consisted of a head frame, light-emitting diodes, charge-coupled device cameras, and a personal computer (Gnathohexagraph System; Ono Sokki, Kanagawa, Japan). In a 25-cycle hard gummy jelly chewing test on each side, the mean path of the chewing trajectory was measured in the frontal and sagittal views. During left-side chewing, the frontal view had a reversed pattern in the mean path of the jaw movement trajectories, and a chopping pattern was seen in the sagittal view ( Fig 4 ). During right-side chewing, the mean path of the chewing trajectory described a figure 8 in the frontal view, with a chopping pattern tendency in the sagittal view ( Fig 5 ).
Occlusal force and occlusal contact area were also examined by using an occlusal force recording system (Dental Prescale & Occluser; Fuji Film, Tokyo, Japan). The maximum occlusal force was lower (247 N) and the occlusal contact area was narrower (4.5 mm 2 ) than those of normal subjects.
The mandibular growth spurt had already taken place, according to the hand-wrist radiograph.
In addition to the congenital cataracts and retinal detachment mentioned in the medical history, she had glaucoma and microphthalmia. These were followed up by the department of ophthalmology at the university hospital.
Mitral valve regurgitation was observed; however, a medical checkup showed no problems that would prevent her from undergoing surgery. Additionally, a slight unilateral hearing impairment and radioulnar synostosis of the left arm were observed.
This patient was diagnosed as having an Angle Class III malocclusion with a skeletal Class III jaw-base relationship, a high mandibular plane angle, an anterior crossbite, severe crowding, a congenital absence of the mandibular central incisor, radiculomegaly of the canines and the first premolars, and OFCD syndrome.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


