This article describes the surgical and orthodontic treatment of a 12-year-old boy with a significant deformity and functional involvement caused by hemifacial microsomia. The left mandibular ramus and condyle were hypoplastic and abnormal in form and location. The lower third of the face was increased, with mandibular retrusion and significant facial asymmetry. He had difficulties in speaking and chewing and problems related to his facial appearance, which caused severe psychosocial disturbances. The patient received orthodontic treatment and temporomandibular joint reconstruction with a costochondral graft on the left side while he was still growing. Three-year follow-up records are presented.
The treatment of dentofacial deformities is challenging to orthodontists and maxillofacial surgeons. Attaining good functional, esthetic, and stable results is even more difficult if the patient is still growing and has associated pathologies such as hemifacial microsomia.
Hemifacial microsomia is the second most common facial birth disorder after cleft lip and palate, with an incidence of 1 in 3500 to 6000 live births. The condition is bilateral in about 10% of these subjects. The cause is unknown, but the pathogenesis seems to be attributable to damage to the stapedial artery, which can cause hematoma formation in the first and second branchial arches, resulting in abnormal growth and malformation of the mandible. Another theory suggests that the death of neural crest cells can result in dysmorphology of the branchial arches that is similar to that found in hemifacial microsomia.
The most important clinical findings in hemifacial microsomia are mandibular malformation with facial asymmetry and microtia. Hypoplasia of the soft tissues, orbital involvement, nerve disorders, and other affected anatomic structures are present with a wide range of variations. Therefore, different modalities of treatment might be needed depending on the age of the patient and the severity of the problems.
The purpose of this article was to describe the treatment of a patient with a severe facial deformity due to hemifacial microsomia. Combined orthodontic treatment and orthognathic surgery with a costochondral graft were performed while the patient was still growing. Three-year follow-up records are shown.
Diagnosis and etiology
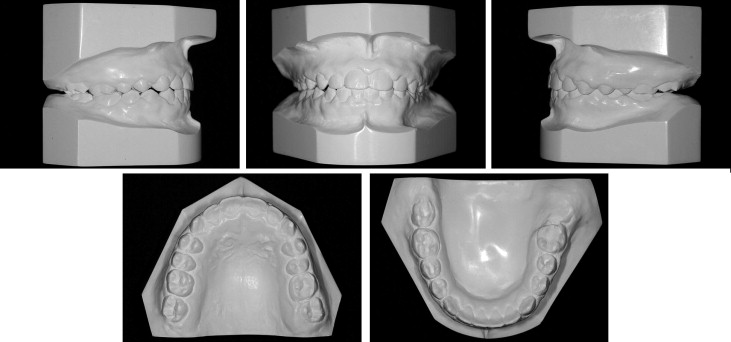
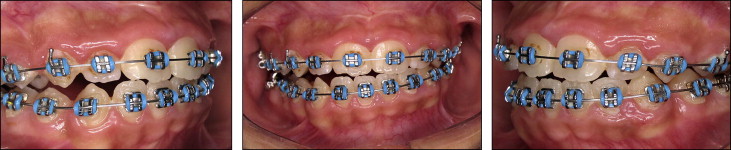
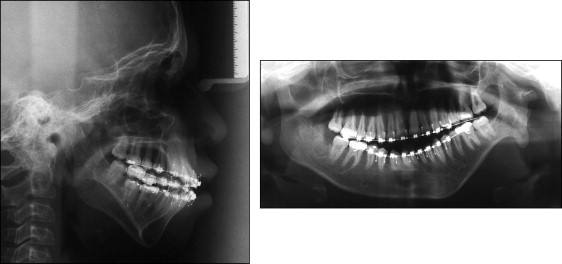
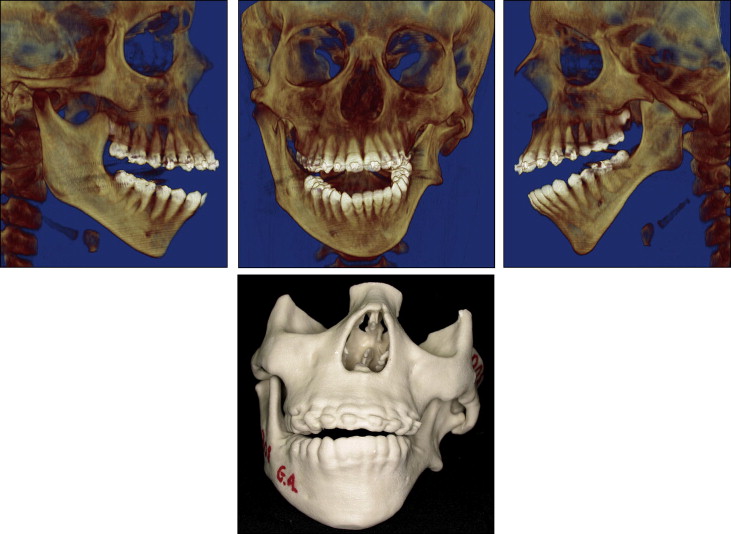
The patient came to the Oral and Maxillofacial Surgery Department of the State University of Rio de Janeiro, Rio de Janeiro, Brazil, with a severe facial deformity with functional and esthetic involvement. He had been seeing an orthodontist since he was 8 years of age, and facial photographs and dental casts from this time were available ( Figs 1 and 2 ). When he came to our institution, he was wearing fixed orthodontic appliances, which were placed when he was 12 years old. His chief complaints were related to his facial appearance and functional problems that were causing severe psychosocial disturbances. Clinical evaluation showed vertical maxillary excess, mandibular retrusion, and significant facial asymmetry with chin deviation to the left side. A marked occlusal cant in the frontal plane was present with tilting of the corners of the mouth. The left external ear was malformed, with a rudimentary auricle ( Fig 3 ). The most noticeable functional problems were difficulties in speaking and chewing, lack of lip seal, mandibular deviation during function, and no reproducible centric occlusion. Intraoral photographs showed a Class I malocclusion with a Class III tendency and a mild, lateral open bite on the right side; both dental midlines were deviated ( Fig 4 ). Tomographic and prototyping examinations showed type II-B hemifacial microsomia with a hypoplastic left mandibular ramus and condyle that were abnormal in form and location, and malformation of the glenoid fossa ( Figs 5 and 6 , Table ).


| Standard | Presurgical | Postsurgical | Posttreatment | |
|---|---|---|---|---|
| SNA angle (°) | 82 | 82.62 | 81.24 | 81.38 |
| SNB angle (°) | 80 | 77.19 | 79.87 | 80.55 |
| ANB angle (°) | 2 | 5.43 | 1.37 | 0.83 |
| FMA (°) | 25 | 34.23 | 28.21 | 28.72 |
| SN-GoGn (°) | 32 | 38.66 | 31.75 | 29.99 |
| 1/NA (°) | 22 | 27.05 | 29.08 | 29.86 |
| 1-NA (mm) | 4 | 5.77 | 4.27 | 5.06 |
| 1/NB (°) | 25 | 34.00 | 27.73 | 29.29 |
| 1-NB (mm) | 4 | 11.57 | 5.48 | 6.22 |
| 1/1 (°) | 131 | 111.20 | 127.05 | 125.94 |
| IMPA (°) | 93 | 91.01 | 92.24 | 92.88 |
Treatment objectives
Surgical and orthodontic treatment objectives were identified. Because the patient had reasonable leveling, alignment, and coordination of the arches, the main objective was to address his chief complaints and improve his self-esteem. The appliances were maintained, and surgery was performed to correct the deformity. The specific objectives of treatment were (1) asymmetry correction, (2) maxillary impaction and leveling, (3) mandibular advancement with left temporomandibular joint reconstruction, (4) overjet and overbite rectification, and (5) lip seal improvement.
Treatment objectives
Surgical and orthodontic treatment objectives were identified. Because the patient had reasonable leveling, alignment, and coordination of the arches, the main objective was to address his chief complaints and improve his self-esteem. The appliances were maintained, and surgery was performed to correct the deformity. The specific objectives of treatment were (1) asymmetry correction, (2) maxillary impaction and leveling, (3) mandibular advancement with left temporomandibular joint reconstruction, (4) overjet and overbite rectification, and (5) lip seal improvement.
Treatment alternatives
The main alternatives to correct this deformity were (1) orthopedic and orthodontic camouflage, (2) distraction osteogenesis (3) temporomandibular joint reconstruction, and (4) orthognathic surgery.
The first alternative is a more conservative approach, indicated for growing patients with minor deformities. However, in this patient, camouflage of the skeletal problem would be limited to occlusal correction without facial esthetic improvement.
Distraction osteogenesis can be useful when extensive lengthening of the mandible is required. However, this therapy has shown a variable rate of recurrence, problems with intraoral and extraoral devices, and lack of long-term follow-up reports. For these reasons, we did not choose distraction osteogenesis for this patient.
Orthognathic surgery is indicated to obtain adequate jaw relationships and facial symmetry when the temporomandibular joint is functional. In more severe cases, temporomandibular joint reconstruction with orthognathic surgery might be necessary and can be accomplished by placing bone grafts or temporomandibular joint prostheses. A costochondral graft is a common method used to reconstruct the ramus-condyle unit, because it has growth potential. The disadvantages of this method are additional donor-site morbidity, risk of graft resorption and infection, and possible asymmetrical mandibular growth. A temporomandibular joint prosthesis is a predictable option for temporomandibular joint reconstruction without donor-site morbidity. However, the financial costs are higher for this treatment, and it is preferably indicated in patients whose growth has been completed.
Considering the severity of the patient’s skeletal deformity, age, chief complaints, and history of psychosocial problems, we chose a treatment plan that entailed orthodontic treatment and orthognathic surgery with temporomandibular joint reconstruction and a costochondral graft.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


