Introduction
The aim of this study was to analyze the effects of orthopedic therapy with rapid maxillary expansion (RME) in growing patients affected by osteogenesis imperfecta and treated with bisphosphonates.
Methods
Three boys with osteogenesis imperfecta (mean age, 10.6 years) were treated with RME. They all had treatment with quarterly intravenous infusions of bisphosphonates. They were in either the early or the late mixed dentition and had indications for RME. The expansion screw was activated twice daily until correction of the transverse relationships was achieved. The retention period with the expander in place was 6 months. In 2 Class III patients, RME was associated with the use of a facemask. In all patients, occlusal radiographs were taken at the end of active RME therapy to assess the opening of the midpalatal suture and 1 year after the end of active expansion therapy to evaluate the reossification and reorganization of the midpalatal suture.
Results
In all patients, the opening of the midpalatal suture and the healing with reorganization of the midpalatal suture were documented with the occlusal radiographs. No complications were found after a 1-year follow-up.
Conclusions
In growing patients affected by osteogenesis imperfecta and treated with bisphosphonates, it is possible to perform RME with a standard protocol with no complications after a 1-year follow-up.
Highlights
- •
Three growing boys with osteogenesis imperfecta were taking bisphosphonates.
- •
Their orthodontic treatment included rapid maxillary expansion (RME).
- •
Opening and healing of the midpalatal suture were documented.
- •
No complications associated with RME were found after a 1-year follow-up.
Osteogenesis imperfecta (OI), also called “brittle bone disease,” is a heritable disorder of the connective tissues that can lead to multiple fractures, which in serious cases can also affect the patient’s survival. This disease has an estimated incidence of about 1 in 20,000 to 50,000 births, a number that is often underestimated because less serious cases are misunderstood or diagnosed late. The male-to-female ratio is 1:1, with both dominant and recessive transmissions. Numerous studies have established a correlation between OI and COLIA1 and COLIA2 genes that encode for either chain of type 1 collagen. Since this protein is a major constituent not only of bones but also of other uncalcified tissues, this disease can involve various structures of the body, thus requiring a multispecialized medical approach. Extraskeletal manifestations of OI are represented by blue sclerae, dentinogenesis imperfecta, muscle weakness, hearing loss, and joint laxity. Patients with OI have dentoskeletal Class III malocclusions, anterior and posterior crossbites or open bites, impacted teeth, and craniofacial deformities (triangular face shape, protrusion of both temporal bones, and frontal bone prominence). A recent study by Rizkallah et al on a sample of 49 patients with OI (age range, 5-19 years) showed that malocclusions were significantly more severe in the patients with OI than in a control group with no OI. There was a higher incidence of Class III malocclusion associated with anterior and lateral open bites in patients affected by OI.
Bisphosphonates (BPs) are indicated in the treatment of OI because they inhibit bone resorption by osteoclasts, thus favoring bone formation over resorption during remodeling. A systematic review by Castillo et al showed that most studies confirmed improvements in bone density produced by BPs in patients with OI. Many but not all studies demonstrated reductions in fracture rates and enhanced growth. However, the optimal medication and dosing regimen and the duration of treatment with BPs in pediatric patients have not been elucidated yet. A significant potential side effect of BPs in the adult population is the development of osteonecrosis in the mandible or the maxilla, particularly related to intravenous therapy or high-dose, long-term oral usage. A recent systematic review, however, reported no evidence to support the hypothesis of a causal relationship between BPs and osteonecrosis of the jaw occurring either spontaneously or after dental surgery in children and adolescents with OI.
Quite interestingly, the orthodontic literature lacks case reports of children with OI treated with BPs who could require orthopedic treatment with rapid maxillary expansion (RME). The aim of this article, therefore, was to evaluate treatment with RME in 3 patients with OI who had received BPs.
Material and methods
Three boys (mean age, 10.6 years) were treated at the Unit of Pediatric Dentistry of the Department of Oral and Maxillofacial Sciences in collaboration with the Department of Pediatrics and Pediatric Neuropsychiatry of the Sapienza University of Rome in Italy. They all had a diagnosis of OI and were treated with quarterly intravenous infusions of neridronate (Nerixia, 100 mg; Abiogen Pharma, Pisa, Italy). All patients were in either the early or the late mixed dentition and had indications for RME that was performed with a banded expander with bands on the maxillary permanent first molars. The patients’ parents were instructed to activate the expansion screw twice daily until the desired correction of the transverse problem was achieved. The expander was kept in place for 6 months for retention. According to the instructions of the pediatricians of the Department of Pediatrics and Pediatric Neuropsychiatry, the patients received infusions with neridronate right before starting treatment with RME. After 3 months, the next infusion of neridronate was skipped, and it was resumed after 6 months (approximately at the end of the 6-month retention period with the expander in place). For all patients, occlusal radiographs were taken at the end of active RME therapy to assess the opening of the midpalatal suture and after 1 year from the end of active expansion therapy to evaluate the reossification and reorganization of the midpalatal suture.
Case report 1
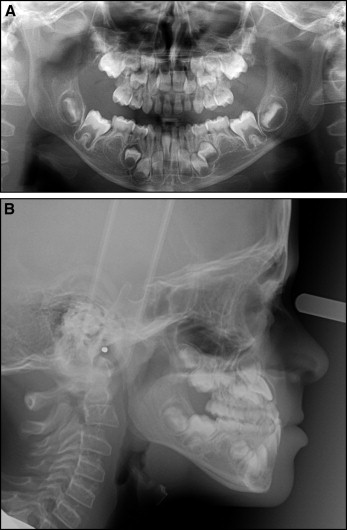
A 7-year-old boy affected by OI with a history of multiple femur fractures, with no blue sclerae, and with mild ligamentous laxity started treatment with neridronate in 2004. At the extraoral clinical examination, the patient showed a Class III flat profile. At the intraoral clinical examination ( Fig 1 ), he was in the early mixed dentition, with no dentinogenesis imperfecta, and had an anterior crossbite and Class III occlusal relationships.

The analysis of the panoramic radiograph ( Fig 2 , A ) showed aplasia of the mandibular left and right second premolars. The pretreatment cephalometric analysis ( Fig 2 ) showed Class III skeletal relationships associated with decreased vertical skeletal relationships. The analysis of the transverse interarch relationships showed a transverse discrepancy of −4 mm. RME was indicated for this patient because a negative interarch discrepancy is often associated with a maxillary skeletal transverse deficiency in Class III patients during the early developmental phases.
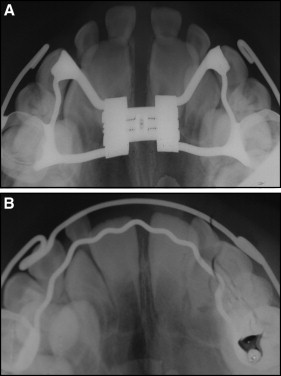
The first phase of treatment consisted of RME with a banded expander that was activated twice daily for 15 days ( Fig 3 , A ). A Delaire facemask was delivered to the patient immediately after RME, and it was applied first using the expander as anchorage and then with a double arch. The elastic traction produced forces of 14 g per side. Orthopedic treatment with the facemask lasted for 1 year. A maxillary Schwarz plate was given to the patient as a retention appliance. The treatment produced favorable changes at both the occlusal ( Fig 4 ) and the skeletal ( Fig 5 ) levels, with an advancement of the maxilla (SNA, +1.9°) leading to improvement in the sagittal skeletal relationships (ANB, +1.9°) ( Table I ). Minor changes (<1°) occurred in the vertical skeletal relationships. The postexpansion occlusal radiograph showed that the opening of the midpalatal suture was completely reossified and reorganized 1 year later ( Fig 3 , B ).


| Pretreatment | Posttreatment | |
|---|---|---|
| SNA | 81.5 | 83.4 |
| SNB | 83.0 | 83.0 |
| ANB | −1.5 | 0.4 |
| N-S-Ar | 112.8 | 117.5 |
| S-Ar-Go | 147.8 | 143.0 |
| Ar-Go-Me | 127.5 | 126.6 |
| Jarabak’s sum | 388.1 | 387.1 |
| FH to GoMe | 28.0 | 27.1 |
| U1 to palatal plane | 110.5 | 127.0 |
| L1 to mandibular plane | 71.5 | 90.2 |
| Interincisal angle | 154.7 | 120.4 |
Case report 1
A 7-year-old boy affected by OI with a history of multiple femur fractures, with no blue sclerae, and with mild ligamentous laxity started treatment with neridronate in 2004. At the extraoral clinical examination, the patient showed a Class III flat profile. At the intraoral clinical examination ( Fig 1 ), he was in the early mixed dentition, with no dentinogenesis imperfecta, and had an anterior crossbite and Class III occlusal relationships.
The analysis of the panoramic radiograph ( Fig 2 , A ) showed aplasia of the mandibular left and right second premolars. The pretreatment cephalometric analysis ( Fig 2 ) showed Class III skeletal relationships associated with decreased vertical skeletal relationships. The analysis of the transverse interarch relationships showed a transverse discrepancy of −4 mm. RME was indicated for this patient because a negative interarch discrepancy is often associated with a maxillary skeletal transverse deficiency in Class III patients during the early developmental phases.




