This case report describes the successful treatment of an adult with lip protrusion and a previously traumatized maxillary central incisor that had experienced replacement root resorption. An extracted premolar was transplanted into the incisor space and retracted orthodontically. Autotransplantation was successful with complete root formation and, combined with orthodontic treatment, provided a satisfying esthetic outcome.
Replacement root resorption is a major complication after replantation of avulsed tooth. Whereas inflammatory external root resorption can be arrested or repaired by appropriate endodontic therapy, replacement resorption is hard to treat. When a large area of the root surface (>4 mm 2 ) is damaged by the avulsion, the tooth is likely to be ankylosed permanently. As a consequence of the ankylosis, the tooth is remodeled in a fashion similar to bone remodeling, with bone gradually replacing the tooth. This process is referred to as replacement root resorption. A delayed replantation might cause ankylosis with subsequent bone substitution followed by loss of the tooth.
Especially when an anterior tooth is ankylosed during the growth period, it results in infraocclusion and causes esthetic issues. Since conventional orthodontic movement of ankylosed teeth is not possible, a surgical procedure such as segmental osteotomy or alveolar bone distraction osteogenesis can be combined during orthodontic treatment. However, in patients with severe replacement resorption, extraction of the tooth is inevitable for orthodontic treatment.
Several reports indicate successful autotransplantation of an orthodontically extracted premolar as a central incisor in growing adolescents before the root is fully formed; this is the best timing for successful autotransplantation and an optimal prognosis of the transplant.
Here, we report on an adult with a traumatized central incisor showing severe replacement resorption who was successfully treated by orthodontics combined with autotransplantation. To relieve crowding and protrusion, we performed autotransplantation of an extracted premolar and achieved proper occlusion by retraction of the anterior teeth, including the transplanted premolar.
Diagnosis and etiology
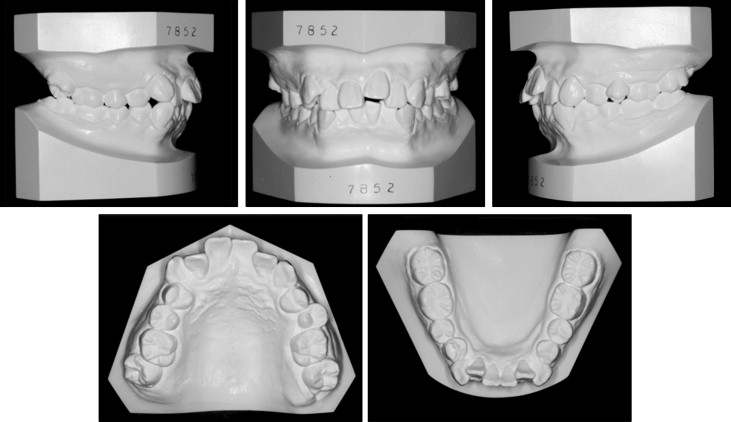
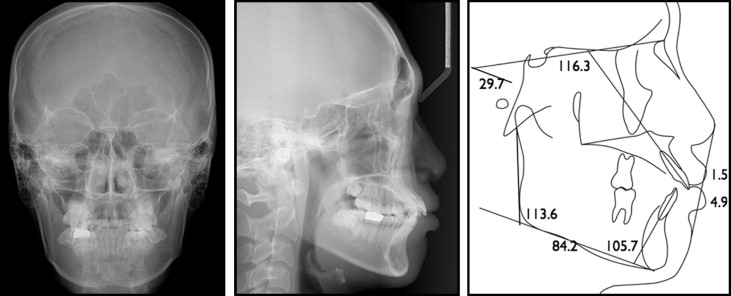
The patient was a 22-year-old man having a chief complaint of crowding. Because of trauma in childhood, the maxillary left central incisor had been avulsed and replanted. The initial intraoral photographs showed that the gingivally positioned incisor was discolored, indicating ankylosis ( Fig 1 ). The panoramic and periapical radiographs confirmed the replacement root resorption of the left central incisor, although proper endodontic treatment had been completed ( Fig 2 ). The patient had moderate crowding with buccoversion of the maxillary right second molar. Molar relationships were Class I on the left side and mild Class II on the right side ( Fig 3 ). The pretreatment facial photographs showed protrusive upper and lower lips, an acute nasolabial angle, and hyperactivity of the mentalis muscle. In the posteroanterior cephalogram, no facial asymmetry was observed. The lateral cephalogram analysis showed a Class I skeletal pattern with a normodivergent profile. Proclination of the maxillary and mandibular incisors (U1 to SN, 116.3°; IMPA, 105.8°) and consequent lip protrusion were noticed ( Fig 4 , Table ).


| Measurement | Pretreatment | Posttreatment |
|---|---|---|
| SNA angle (°) | 83.2 | 84.0 |
| SNB angle (°) | 80.3 | 81.8 |
| ANB angle (°) | 2.9 | 2.2 |
| Wits appraisal (mm) | 1.2 | −0.9 |
| SN to mandibular plane (°) | 29.7 | 25.1 |
| Bjork sum (°) | 389.7 | 385.1 |
| Gonial angle (°) | 113.6 | 111.3 |
| Mandibular body length (mm) | 84.2 | 89.1 |
| U1 to SN (°) | 116.3 | 102.9 |
| IMPA (°) | 105.7 | 103.0 |
| Upper lip to Ricketts’ E-line (mm) | 1.5 | −0.8 |
| Lower lip to Ricketts’ E-line (mm) | 4.9 | 1.8 |
Based on these findings, the patient was diagnosed with skeletal Class I bialveolar protrusion with crowding and replacement resorption of the maxillary left central incisor.
Treatment alternatives
Under normal circumstances, extraction of the 4 first premolars would be considered to relieve crowding and to improve lip protrusion. However, because of the replacement resorption, the left central incisor had a hopeless prognosis. Therefore, several treatment options to replace this incisor were discussed.
The first option was to replace the central incisor with a dental implant or a bridge after orthodontic treatment with 4 premolar extractions. Although a dental implant provides an esthetic outcome in terms of tooth morphology, this patient had a vertical alveolar bone defect with varying gingival margins of the central incisor initially. In addition, alveolar bone remodeling and changes in the gingivae after anterior retraction were not predictable. This might have required additional hard-tissue and soft-tissue surgical procedures of the implant site after orthodontic treatment for maximum esthetic results with a longer treatment time.
The second option was to replace the central incisor with autotransplantation of 1 of the extracted premolars and continue conventional orthodontic treatment. In this patient, the maxillary left premolar was chosen based on its crown and root morphology. Computed tomographic images showed that it had a conical single and relatively flat root that would fit the recipient site better than the mandibular premolar. Also, because the mesiodistal length of the central incisor and the buccolingual length of the first premolar were 9.8 and 10.6 mm, respectively, the premolar could replace the central incisor if it was rotated by 90°. This option conserved 1 natural tooth, and leveling and alignment of the transplant would improve the alveolar bone and gingival levels. Because autotransplantation is a part of orthodontic treatment, there was no extension in terms of total treatment time. However, careful monitoring of complications after autotransplantation, such as ankylosis and subsequent replacement resorption and additional tooth reshaping, is mandatory.
The third option was to substitute the central incisor, lateral incisor, and canine with the lateral incisor, canine, and first premolar, respectively, in the maxillary left quadrant with extraction of 3 first premolars in the other quadrants. In this case, additional extractions in the maxillary left quadrant would not be necessary, but further prosthetic requirements and esthetic limitations by the substitution would be raised.
These treatment alternatives were discussed with the patient. The second option with autotransplantation was selected.
Treatment progress
Because the patient showed mild gingival inflammation before treatment, he was referred to the Department of Periodontics for general periodontal treatment. After extraction of the 3 premolars, 0.022-in Roth prescription resin brackets (Esther MB; Tomy International, Tokyo, Japan) were bonded, except for the maxillary left central incisor, and space regaining for the autotransplantation was initiated ( Fig 5 , A ). The maxillary left first premolar (donor tooth, Fig 5 , A ; arrow) was endodontically treated for autotransplantation and was included in the alignment process because preapplication of orthodontic force is considered useful for successful autotransplantation.




