(1)
Canberra, ACT, Australia
Summary
Successful tooth movement requires a sound knowledge base of the interrelationships between the tooth and periodontium. Prior insults to the tooth and its supporting structures may affect its response and the outcome of treatment. The need for a thorough history, examination and baseline measurements is essential for the medical record, treatment planning and informed consent process. The interrelationships between dental specialities and timely intervention are paramount to achieving a successful outcome.
Clinical Relevance
Orthodontic movement of the teeth will induce some degree of pulpal inflammation. Poorly controlled heavy forces on the teeth, previous history of trauma or ongoing insults such as caries may result in loss of pulp vitality. Combined endodontic–orthodontic treatment planning can benefit the overall tooth prognosis by ensuring optimal endodontic treatment has been undertaken. Endodontically treated teeth can be moved orthodontically just as readily as vital teeth. Traumatised teeth and in particular intrusive luxation injuries may be at greater risk of moderate to severe root resorption. The general dentist, endodontist and orthodontic professional need to ensure from history taking to execution of treatment that sound methodological principles are followed to fulfil treatment objectives ensuring a successful outcome.
17.1 Orthodontic Tooth Movement and Vital Teeth
Orthodontic forces will evoke a biological response within the dental pulp, resulting in some degree of transient pulpal inflammation [1]. What is of clinical significance is whether the response evoked could lead to long-term changes to the vitality of the tooth. The survival of the dental pulp is dependent on the blood vessels that access the interior of the tooth through the apical foramen. Any changes in pulpal blood flow or vascular tissue may have implications to the health of the dental pulp. Use of light forces is thought to reduce damage to the pulp and allow time for repair [2]. In contrast, rapid orthodontic tooth movement and heavy continuous forces are thought to increase the risk of pulpal injury, as undermining resorption allows increasingly large increments of change, leading to alterations in the blood vessels at the peri-apex of the tooth and those entering the tooth apically [3].
Human studies have demonstrated pulp necrosis after various tooth movements such as intrusion [4] and extrusion [5] due to circulatory disturbances in dental pulp. It is generally assumed that pulpal changes and their consequences appear to be more severe with larger orthodontic forces [6], but sound scientific data to support this assumption are lacking. One study found a higher prevalence of loss of pulp vitality and root resorption on previously traumatised teeth undergoing tipping orthodontic movements; however, the sample size was small and heterogenous [7]. With the available evidence, it is not possible to conclude that orthodontic tooth movement of traumatised teeth increases the risk of pulp necrosis. A systematic review was performed to investigate the relationship between orthodontic force level and pulp reaction in human teeth [8]. This relationship, which would seem to be of utmost clinical importance, remains yet to be elucidated.
17.2 Orthodontic Tooth Movement of Endodontically Treated Teeth
A retrospective study examining 45 orthodontic patient records treated with various orthodontic techniques found those teeth that have undergone root canal treatment, including 4 teeth that had undergone peri-radicular surgery, moved as readily as teeth with vital pulps [9]. This presumes that there are no factors that may prevent tooth movement, such as replacement resorption (ankylosis) or injury to the apical periodontal ligament that may limit its remodelling [10].
There are mixed reports of root resorption in endodontically treated teeth subjected to orthodontic tooth movement. Some authors have found increased rates [9] and others have found reduced rates of root resorption [11]. A recent retrospective study, where the adjacent maxillary incisor acted as a control, found no statistical difference between the vital control tooth compared to the root-treated tooth [12].
17.3 Factors Affecting Root Resorption During Orthodontic Tooth Movement
Orthodontically induced inflammatory root resorption (OIIRR), or root resorption (RR), is an unavoidable pathological consequence of orthodontic tooth movement [13]. RR is undesirable because it may affect the viability of a tooth long term; therefore, it is important to identify those factors that may contribute to RR, in an attempt to minimise its effects.
Andreasen defines three types of external root resorption [14]:
1.
Surface resorption, which is a self-limiting process, usually involving small outlining areas followed by spontaneous repair from adjacent intact parts of the periodontal ligament
2.
Inflammatory resorption, where initial root resorption has reached dentinal tubules of an infected necrotic pulpal tissue or an infected leukocyte zone
3.
Replacement resorption, where bone replaces the resorbed tooth material that leads to ankylosis
Tronstad further subdivides inflammatory resorption, which is seen on the walls of the root canal (internal resorption) and on the external surface of the root (external resorption), into two types [15]:
1.
Transient inflammatory resorption occurs when the stimulation is minimal and for a short period. This defect is usually undetected radiographically and is repaired by a cementum-like tissue.
2.
Progressive inflammatory resorption occurs when stimulation is for a long period.
RR after orthodontic treatment generally takes the form of surface resorption [14] or transient inflammatory resorption [15]. Replacement resorption is rarely if ever seen after orthodontic treatment. Orthodontic forces act similarly on bone and cementum. Due to the greater resistance of cementum to resorption compared to bone, orthodontic forces cause bone resorption, which leads to tooth movement. However, resorption of the cementum and dentine may also occur (see Fig. 17.1) [16].
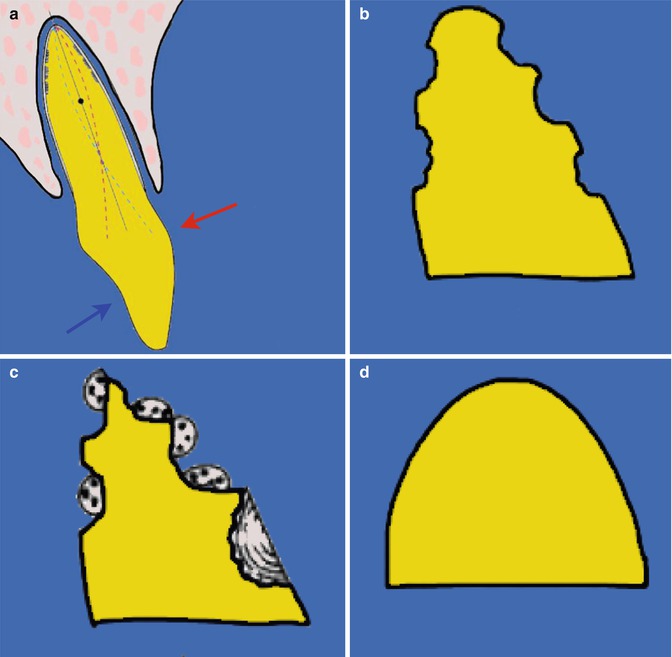
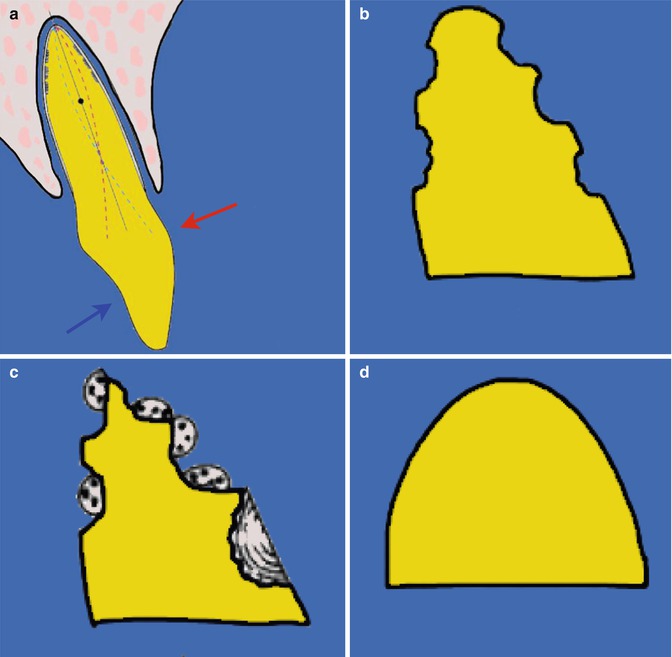
Fig. 17.1
Clinical diagram showing (a) effects of orthodontic tooth movement resulting in (b) root resorption lacunae that if not repaired may cause (c) a sequestration at the apex, (d) which when resorbed results in external apical root resorption (Adapted form Roberts et al. [83])
The Malmgren index utilises a graded scale 0–4, to classify OIIRR as mild (apical RR <2 mm) or moderate (apical RR 2 mm – 1/3 of root length), which is seen in most orthodontic patients [17]. Severe RR (>4 mm or a third of the original root length) is seen in less than 5 % of orthodontically treated teeth [18]. The use of this index was originally described for use with intra-oral radiography, which has inherent limitations due to the two-dimensional representation of a three-dimensional structure (see Fig. 17.2).
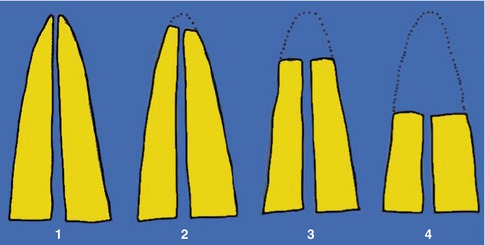
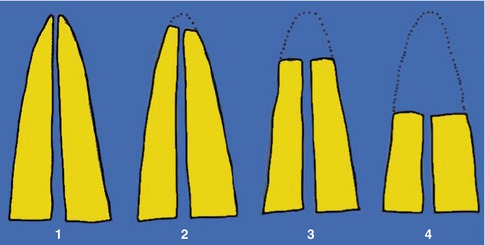
Fig. 17.2
Clinical diagrams demonstrating Malmgren root resorption index for quantitative assessment of root resorption. Note (1) irregular root contour, (2) apical root resorption less than 2 mm of original root length, (3) apical root resorption from 2 mm to one-third of original root length and (4) apical root resorption exceeding one-third of original root length
The aetiological factors of RR are complex and multifactorial. Many variables have been suggested in the literature from individual biological variability, genetic predisposition, root morphology, history of trauma and mechanical factors. Regardless of genetic or treatment-related factors, the maxillary incisors consistently experience more apical RR than any other teeth, followed by the mandibular incisors and first molars [17]. Despite the extensive literature that exists on this topic, there is a lack of consensus on the aetiological factors, in part due to differing study designs, heterogenous and small sample sizes and methods used for assessing root resorption [13, 16, 17].
A systematic review attempted to elucidate the effect of orthodontic treatment on RR [19]. Following review of 144 articles, 13 fulfilled the inclusion criteria. A number of studies included were conducted over a short period of time and thus not representative of a full 18–24-month course of orthodontic treatment. Evidence exists that orthodontic force applied to teeth over a short period can produce resorption lacunae without signs of RR [20]. In addition many studies examined premolars, a tooth which quite often does not experience significant RR. The key findings were that teeth undergoing orthodontic movement had significantly more RR compared to control teeth. Heavy forces produced significantly more RR than those treated with light forces and thermoplastic appliances [21–26]. There was limited evidence that continuous force application produced significantly more RR than discontinuous force application [27], possibly because the pause allows the resorbed cementum to heal and prevents further resorption. The studies examining intrusive force applications found significantly increased RR rates compared with controls [21, 28]. Incisors with clinical signs or patient reports of trauma (but no signs of RR) had the same prevalence of moderate to severe RR as those without trauma [29–31]. There is a lack of high-quality evidence on OIIRR on previously traumatised teeth with pre-existing RR; observational data indicate a greater chance that orthodontic movement will enhance the resorptive process in these teeth [16]. There is no evidence that RR is affected by arch wire sequence or bracket system used and little evidence that unusual tooth morphology plays a role in increased RR. RR associated with orthodontic treatment ceases after active treatment [11].
Although RR is of concern to many general dental practitioners and dental specialists [32], even extensive RR does not appear to affect the functional capacity or the longevity of the teeth. Apical RR has been shown to be less critical on the area of remaining periodontal support than loss of crestal alveolar bone support, with 3 mm of RR approximately equivalent to 1 mm of crestal bone loss. This may explain why tooth loss from apical shortening has not been reported in the literature [33].
Until more high-quality clinical evidence is published, best practice involves thorough patient counselling at the outset of treatment. Clinically, use of light forces is important especially for intrusive movements. Good record keeping including radiographs taken at baseline and after 6–9 months may detect early signs of RR. In cases where RR has been diagnosed, there is some evidence that a 2–3-month pause in treatment with a passive arch wire decreases further RR. If severe resorption is identified, the treatment plan will need to be reassessed with the patient. After treatment, if severe RR is shown on the final radiographs, follow-up radiographic examinations may be indicated until the resorption has stabilised. If it continues, sequential root canal therapy with calcium hydroxide has been shown to be of benefit [34].
17.4 Management of Endodontic Procedures During Orthodontic Treatment
During orthodontic tooth movement, both retention of a calcium hydroxide dressing in the root canal [35, 36] and obturation of the root canal with a definitive gutta-percha root canal filling prior to orthodontic tooth movement [37] have been recommended. The former recommendation is based on clinical experience and the latter is based on findings from animal studies [38], where no significant difference was found in resorption of the teeth managed by either method.
In cases of external inflammatory root resorption, long-term calcium hydroxide treatment is more effective than short-term treatment in promoting root surface healing with new cementum [39]. An increased risk of cervical root fracture in traumatised immature teeth treated with calcium hydroxide over prolonged periods of time during apexification has been reported [40]. Rosenburg et al. compared the dentine fracture strength of teeth dressed with calcium hydroxide paste and teeth obturated with gutta-percha, finding that the micro-tensile fracture strength of dentine was reduced by 43.9 %. This suggests the clinical use of calcium hydroxide over a prolonged period of time, such as what would be required over a course of orthodontic treatment, should be reviewed [41]. These findings support recommendations of completing definitive root canal therapy prior to a definitive course of orthodontic tooth movement [37], with a well-cleaned and obturated root filling with a good coronal seal [42]. The exceptions are when a calcium hydroxide dressing is required for a longer period, such as in inflammatory resorption, or for apexification in an immature open apex incisor, although a single visit mineral trioxide aggregate is found to be a predictable treatment [43].
Recommendations relating to commencement of orthodontic tooth movement following endodontic intervention are based on clinical judgement and experience rather than being founded on evidence from well-designed studies. The outcome of root canal treatment should be assessed for at least 12 months after completion and subsequently as required. A favourable outcome is indicated by absence of pain, swelling and other symptoms, no sinus tract, no loss of function and radiological evidence of a normal periodontal ligament space around the root [44].
In cases where root canal treatment has been undertaken as a result of pulp necrosis due to caries, orthodontic tooth movement can commence immediately, in the absence of symptoms. Where there has been bone loss, tooth movement should be delayed until there are clinical and radiographic signs of some healing. Where endodontic therapy has been carried out following dental trauma, an interval of 1 year is recommended prior to proceeding with orthodontic treatment to increase the likelihood of complete healing and the absence of ankylosis [36, 37]. An animal model has shown that, although orthodontic forces applied to root-filled teeth delays the peri-apical healing process in comparison to obturated contralateral incisors, it does not prevent it, with a reduced peri-apical radiolucency visible in orthodontically moved teeth [45] (see Sect. 17.8.2). This work suggests that tooth movement may be commenced prior to complete radiographic resolution of peri-apical lesions.
Endodontic procedures needed during orthodontic treatment may prove a challenge from diagnosis to execution of the definitive obturation. Presenting symptoms may be attributable to tooth movement or due to a necrotic pulp. Orthodontic bands and attachments may obscure detection of caries clinically and radiographically as well as prevent an accurate response with electrical and thermal pulp testers. Radiographically changes in response to tooth movement may be misinterpreted as originating from pulpal demise. Coronal access may be hindered in cases with lingual attachments, an increasingly popular appliance with an increasing adult demographic. Apical resorption may hinder working length determination due to destruction of the apical constriction at the cemento-dentinal junction. Electronic apex locators will not be accurate in such cases. Obturation filling material may also extend beyond the tooth where the apical constriction has been lost.
17.5 Orthodontics and Its Role in Trauma
The risks and incidence of dental trauma in children increases with age, from 5 % at age 8 to 11 % by age 12, with boys at greater risk [46]. An increased overjet and lip incompetency will increase the risk [47, 48]. Prevention of trauma forms the first line of treatment with children participating in contact sports advised to wear protective mouth guards. However, it is important to note that most incidences of trauma are sustained doing activities unrelated to sport [35]. Children, who have sustained trauma, particularly at a young age, will often experience repeated episodes of trauma to their teeth [49]. Timely treatment of any malocclusions should be sought, although factors such as dental health and dental development may affect commencement of treatment.
In the event of trauma, management will vary depending on the type of traumatic injury and the stage of root development of the affected tooth.
Intrusive injuries are crushing by nature and can lead to significant damage to the tooth and its supporting structures. Guidelines on management of intrusion exist [50, 51]. Due to the low occurrence of this type of injury, randomised, controlled trials are not available. Evidence on outcomes has been obtained from retrospective clinical studies. Mild intrusion injuries (0–3 mm) often require a period of observation to allow the tooth to re-erupt. If no change is seen, orthodontic repositioning should commence 2–3 weeks after the injury. Moderate (3–6 mm) to severe (greater than 6 mm) intrusion injuries often require active repositioning, either surgically or orthodontically [52]. There is no clear indication of which option produces improved outcomes, and the chosen method may often come down to availability of local expertise. Due to the higher risk of inflammatory root resorption, secondary to pulpal necrosis in such injuries, endodontic therapy should be instigated 2–3 weeks after the injury when there has been complete root formation. In teeth with immature roots, these teeth need to be monitored closely for loss of vitality. Teeth that have been surgically repositioned will need to be splinted for 1–2 weeks.
Other types of luxation injuries, such as extrusive luxation, may require repositioning and splinting for 1–2 weeks and lateral luxation injuries up to 4 weeks due to the possibility of an associated alveolar injury [53]. If there has been delayed presentation or no tooth mobility exists, orthodontic repositioning is the best option to realign the tooth. Of note is that in traumatic injuries the adjacent teeth may have been subjected to trauma, and therefore these teeth may not be ideal for orthodontic anchorage and consideration needs to be given to appliance design.
Orthodontic management of teeth that have a history of trauma will vary depending on the nature of the original injury. Few studies exist on the sequelae of traumatised teeth undergoing orthodontic treatment. The studies that exist are often based on small numbers with a heterogenous sample of injuries from which conclusions are hard to draw. Recommended observation times prior to instigating orthodontic tooth movement are based on best practice [36, 54].
In cases of root fracture, healing with a hard tissue callus as opposed to connective tissue is important. To achieve healing, splinting times of 4 weeks have been advocated for apical and middle third root fractures and 4 months for fractures of the cervical third [50]. If orthodontic tooth movement is planned in such teeth, in those that have healed with connective tissue, the coronal fragment alone will move and thus the tooth will in effect need to be treated as a tooth with a short root. In such cases, prior to tooth movement, any signs of coronal pulp necrosis need to be treated. It has been recommended to wait 2 years prior to commencing orthodontic treatment in affected teeth [55]; however, in the absence of symptoms, other authors have recommended a shorter period of a year [36].
The success of a replanted tooth following an avulsion injury is strongly dependent on time outside of the mouth. After 60 min, even if stored in a physiological solution or 30 min of dry time, healing is almost always by replacement resorption. Parents and teachers are therefore encouraged to replace the tooth at the site of the incident if at all possible. Once replanted, the tooth is splinted for 7–10 days. Replanted teeth will need to undergo endodontic treatment as soon as feasible in all cases apart from open-apex teeth with a short extra-oral time. Even in the latter case, affected teeth need to be monitored closely for signs of loss of vitality and appropriate endodontic therapy instigated if necessary [56–59]. Orthodontic tooth movement of a replanted tooth is possible if replacement resorption has not occurred. It is recommended to wait a year before commencing tooth movement to allow periodontal healing to occur [36]. In a growing child, healing by replacement resorption becomes apparent with continued vertical alveolar development of the adjacent teeth (see Sect. 17.8.6). In an adult, replacement resorption will be less apparent from the clinical picture and often only detected once orthodontic movement has commenced (see Sect. 17.8.5).
Autotransplantation of teeth in the management of trauma may be suitable if an upper incisor is lost and there is premolar crowding. The ideal donor tooth for an upper incisor site is a lower premolar. The technique is operator sensitive and relies on an atraumatic technique for handling the donor tooth and management of the recipient site. Once transplanted, the tooth is splinted for 7–10 days. Endodontic therapy is instigated in teeth that have closed apices 1–2 weeks post transplantation. Teeth that have open apices or immature roots need to be closely monitored for loss of pulpal vitality. Orthodontic tooth movement can commence once periodontal healing has occurred between 3 and 9 months [60]. Autotransplanted teeth if successful will behave as any other teeth and retain the potential to induce alveolar bone growth. Even in cases where replacement resorption occurs, the transplanted tooth will slowly resorb, maintaining bone in the area for future replacement options.
In conclusion, orthodontic repositioning is useful in the immediate management of traumatically displaced teeth. Orthodontic tooth movement is possible on previously traumatised teeth. Certain injuries such as intrusive luxation and avulsion may be at higher risk of negative sequelae, such as inflammatory root resorption and ankylosis. Good clinical and radiographic records are essential to obtain informed consent as well as a lengthy discussion with the patient and family regarding the possible outcomes.
17.6 Effect of Orthognathic Surgery on Pulp Vitality
Orthognathic surgery is used to alter the underlying skeletal pattern in individuals with dento-facial deformity or malocclusions resulting from trauma to the maxillo-mandibular complex. An adequate blood supply to mobilised dento-osseous segments is crucial for the success of any orthognathic intervention. Furthermore, this blood supply is vital for the preservation of a healthy pulp and periodontium [61–63].
The laser Doppler flowmeter (LDF) has been used to evaluate changes in blood flow through non-invasive measurement methods and to investigate vascular changes associated with orthognathic surgery [64, 65]. The Le Fort I osteotomy technique is frequently employed for altering the maxillary spatial position. During this procedure, the posterior superior alveolar vessels are transected with the palatal pedicle then becoming the primary source of blood supply to the maxilla [61, 63]. Studies have suggested that ischaemic episodes in mobilised maxillary segments may occur for a brief period after surgery. This ischaemic period is thought to be responsible for potential negative sequelae, such as degenerative pulpal changes [66]. A bilateral, sagittal split osteotomy does not interfere with the collateral blood supply and risk of severing the inferior alveolar artery is small. Consequently, pulpal changes may be less likely in mandibular osteotomies compared to maxillary procedures [62].
Human studies using LDF have demonstrated a pulpal hypervascular period occurring immediately after a Le Fort I osteotomy. This is then followed by a statistically significant reduction in the perfusion of the pulp, which has still not recovered 4–6 months after surgery. However, a high variability of individual blood flow patterns was found [67, 68]. Literature looking at segmental osteotomies has found similar findings [69].
A hypervascular episode may be of significance to the dental pulp because of its enclosure in a rigid shell of hard tissues, leading to a possible increase in tissue pressure and ultimately pulpal injury or death. During the informed consent process, it may be beneficial to inform patients planned for a Le Fort I osteotomy that there may be a small risk of loss of vitality and discolouration of the maxillary incisor teeth resulting in a need for root canal therapy.
17.7 Orthodontics to Aid Restorative Procedures
Orthodontic extrusion or forced eruption of a tooth is based on sound orthodontic and osteophysiologic principles [70, 71]. Ingber demonstrated that the teeth could be erupted for crown lengthening, altering gingival margins and levelling osseous defects. As teeth are extruded using light forces, both the bone and gingiva migrate coronally [72, 73]. Eruptive tooth movements result in stretching of the gingival and periodontal ligament fibres with a consequent coronal shift of the bone at the base of the defect as the tooth moves occlusally [74, 75].
Teeth with deep carious margins requiring endodontic treatment, fractured tooth margins below crestal bone, isolated vertical periodontal defects, lateral root perforation and unusual coronal access are some situations that may benefit from forced eruption [76]. The benefits of extrusion are to allow a sound tissue margin for restoration and ensure the maintenance of the biological width. In extruding the tooth for subsequent restoration, it is important to ensure sufficient root length remains within the bone, leaving a minimum 1:1 crown–root ratio. Forced eruption is increasingly been used for implant site development in teeth with poor prognosis with associated periodontal and osseous defects, enhancing both hard and soft tissue defects [77–79]. Dento-alveolar ankylosis is a frequent complication after replantation and may not be amenable to orthodontic extrusion. Decoronation of ankylosed teeth in infra-position has been clinically proven to preserve alveolar width and rebuild lost vertical bone of the alveolar ridge in growing individuals, re-establishing ideal alveolar conditions prior to implant insertion once growth has stopped. The predictable success of decoronation also strongly supports the indication for replantation of avulsed teeth in children even when the extra-alveolar conditions indicate that healing might be compromised by ankylosis [80–82].
17.8 Clinical Cases
17.8.1 Avulsion: Immediate Replantation Adult
A 25-year-old soldier was referred for management of his class 2 division 1 occlusion. There was a history of trauma to the upper left central incisor, resulting in an uncomplicated crown fracture, which was restored. The upper right central incisor (tooth 11) was avulsed following the initial orthodontic assessment appointment during a physical training session. This tooth was stored in milk and replanted within 30 min and underwent root canal treatment 3 days later.
On examination there was a severe skeletal 2 pattern, an incompetent lip pattern, a 12-mm overjet and class 2 buccal segments.
The patient was counselled on the possibility of ankylosis of the upper right central incisor (tooth 11). The treatment plan involved combined orthodontics and orthognathic surgery to address the dental and skeletal pattern. The patient commenced pre-surgical orthodontics and tooth 11 was bypassed initially. Active tooth movement of tooth 11 was commenced 6 months after replantation following establishment of periodontal healing, similar to management of transplanted teeth [59]. This was in contrast to best practice which recommends a 12-month monitoring period [36]. The patient had no clinical symptoms, and the immediate replantation and endodontic therapy indicated a more favourable prognosis for this tooth. Good movement of tooth 11 was achieved with no associated pathology evident (Fig. 17.3).
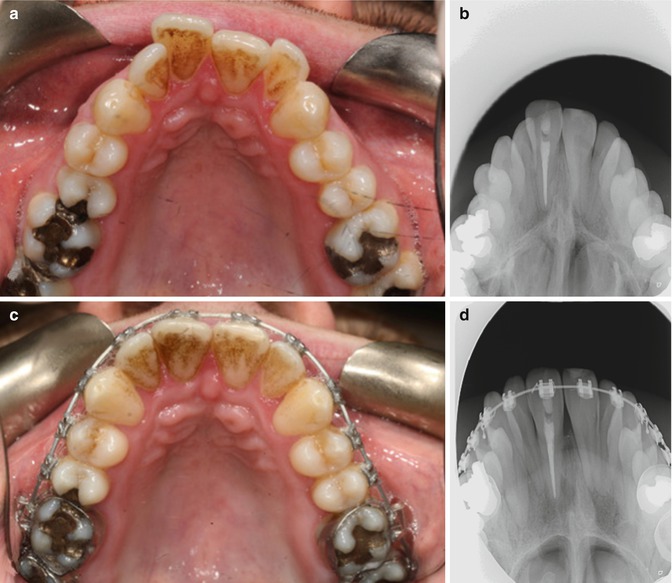
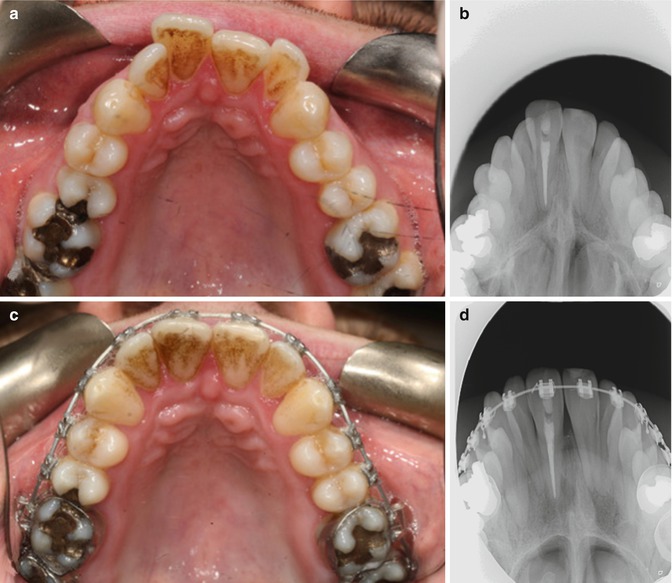
Fig. 17.3
Clinical photographs and radiographs showing (a) pre-treatment intra-oral view and (b) occlusal radiograph demonstrating no pre-existing peri-apical pathosis associated with tooth 11. (c, d) Six months post commencement of pre-surgical orthodontics
17.8.2 Avulsion: Immediate Replantation Adult
A 26-year-old naval sailor was referred for management of his class 2 division 1 occlusion. There was a history of trauma to both upper central incisors 4 years previously, resulting in avulsion of the upper left central incisor (tooth 21) and subluxation and a complicated crown fracture of the upper right central incisor (tooth 11). The avulsed tooth was stored in saliva and replanted within 60 min. Both upper central incisors underwent root canal treatment within a few days.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


