and Jasdeep Kaur1
(1)
Earth and Life Sciences Vrije Universiteit Amsterdam and ILEWG, Amsterdam, The Netherlands
2.1 Introduction
2.4.1 Age Estimation
2.4.3 Stature
2.4.4 Heredity
2.4.8 Bite Marks
2.4.9 Facial Reconstruction
2.5 Conclusions
Abstract
Forensic odontology is defined as a specialized branch of odontology that studies the role of orodental features in the legal professions. This chapter focuses on the use of the human orodental and surrounding structures to allow the identification of living and deceased individuals.
2.1 Introduction
Forensic odontology is a specialized branch of dentistry that studies the proper handling and examination of orodental evidence as well as the evaluation and presentation of orodental findings in the interests of justice and for medicolegal purposes. Dental identification is an establishment of the individuality of a person either dead or living. Dental identification may be required in living persons in the case of absconding criminals, soldiers, missing persons, impostors, escaped prisoners, etc. Identification may be essential where unclaimed dead bodies are found, when bodies are decomposed beyond recognition, and when grossly mutilated bodies or skeletal remains are found. The use of the unique features of the human dentition to aid in personal identification is well established within forensic odontology. The typical comparative dental identification utilizes postmortem and antemortem dental records to determine positive and negative identification, although in a number of cases, the identification of the individual is unknown because antemortem records cannot be found. In such a case, a dental profile of the individual is developed to aid in searching for the individual’s identity by dental indicators of age, ethnicity, habits, professional status, and gender.
2.2 Common Reasons for Identification
Verifying the identity of the deceased is not only important for the family and relatives of the deceased from an emotional standpoint, but it is also a medicolegal requirement. Dental identification of human beings is an important tool in criminal investigations, for social rituals such as burial, and for the identification of individuals missing for prolonged periods. Identification plays an important role in civil cases like insurance claims, matrimonial disputes, property disputes, impersonation, and the issuance of passports and various licenses (Pretty and Addy 2002). The common reasons for identification are as follows (Pretty and Sweet 2001):
-
Marriage: Individuals from many religious backgrounds cannot remarry unless their partners have been confirmed dead.
-
Criminal: Classical forensic investigations into a homicide cannot begin until the victim has been positively identified.
-
Closure: The identification of individuals missing for prolonged periods can bring sorrowful relief to family members.
-
Monetary: The payment of life insurances and other government or private benefits relies upon positive confirmation of death.
-
Burial: Many religions necessitate that a positive identification be made before burial in sacred sites.
-
Social: Society’s duty to preserve human rights and dignity beyond life begins with the basic principle of an identity.
2.3 Dental Identification
Dental identification is very vital tool because teeth may be the only body part that remains intact. Teeth are the hardest substance in the body and can endure extremely adverse conditions (Table 2.1), including high temperatures up to 1,600°C (Andersen et al. 1995). Teeth are the components of the body that often survive severe fires because of their highly resistant composition (Fig. 2.1) and they are protected by the soft and hard tissues of the face and other materials (Delattre 2000). The macroscopic color of unrestored teeth varies depending on the temperature rise and time of application, from a natural color to black, brown, blue, gray, white, and, finally, pink (Endris and Berrsche 1985). The prismatic structure of the enamel was difficult to identify above 1,100°C, while the dentin tubules were identifiable at 1,150°C (Merlati et al. 2004). Dental restorations and prostheses are also extremely durable and can aid in identification (Rφtzscher et al. 2004). It has been reported that glass ionomers were decomposed at 200°C, while the compomers and three different composite materials were deeply altered at 200–500°C (Robinson et al. 1998). A macroscopic observation could identify composite fillings up to 800°C and amalgam fillings up to 1,000°C (Savio et al. 2006). Each dentition is unique to an individual (Pretty and Sweet 2001). The human adult dentition typically consists of 32 teeth, each with five surfaces, thus providing 160 possibilities for individual variations in surface anatomy and dental restorations in configuration, size, shape, material, and wear patterns (Fig. 2.2). This does not even take into account, and is not limited to, such factors as decay, missing and extra teeth, alignment of the dental arches, individual tooth positioning, and prosthetic appliances.


Table 2.1
Effect of heat on human teeth
|
Temperature (°C)
|
Result
|
|---|---|
|
100
|
Whiter to resemble mottled teeth
|
|
Enamel rods dentive altered and root light yellow
|
|
|
200
|
Crown and root orange
|
|
300
|
Crown yellow brown, root destroyed, cracks in enamel and root dark brown
|
|
400
|
Multidirectional cracks in black-brown crown
|
|
500
|
Crown and root grayish-white; multiple cracks and enamel exfoliates
|
|
150
|
No alteration
|
|
175
|
Longitudinal fissures in incisors and canines
|
|
215
|
Carbonization of pulp
|
|
250–300 fibers
|
Centrilobular destruction of enamel and carbonization of tome
|
|
400
|
Crown of healthy teeth split
|
|
800
|
Reduction in volume of root and carbonization of dentin
|
|
1,100
|
Dentin and enamel retain their narrow canals tome fibers
|
|
640
|
Heat of household furnace
|
|
915
|
Silver amalgam may reach this temperature intact
|
|
915–1,090
|
Gold alloy melts synthetic porcelain faces
|
|
1,090
|
Porcelain teeth may survive
|

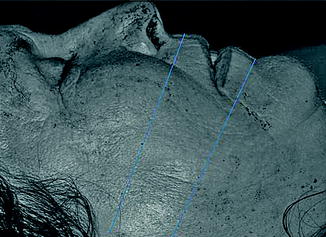
Fig. 2.1
Burned body with intact teeth

Fig. 2.2
Uniqueness of dentition
Norrlander (1997) classified body burns in five categories: (1) superficial burns; (2) destroyed epidermis areas; (3) destruction of the epidermis and dermis and necrosis areas in underlying tissues; (4) total destruction of the skin and deep tissues; and (5) burned remains. Because the destruction of burned victims of the third, fourth, and fifth categories is extensive, remains cannot be identified by common methods. In these cases, forensic odontologists are called in to assist the identification by comparing the postmortem records of the burned, charred, or incinerated individual teeth with the antemortem dental clinical history (Delattre 2000).
Dental identification takes on two main forms:
-
Comparative identification
-
Construction of postmortem profile
2.3.1 Comparative Identification (American Board of Forensic Odontology 2011)
The most commonly performed examination is a comparative identification. This includes the comparison of postmortem dental evidence with antemortem dental records (Fig. 2.3). Generally, when a body or human remains are found, it is reported to the police, who then initiate the request for identification. If this cannot be done by normal forensic methods of identification, then the police or a judge requests that a forensic odontologist perform a dental examination. Often a presumptive or tentative identification of the remains is evident, perhaps from identification cards in the wallet or from photos on a missing persons list, or the antemortem dental records can be located. The forensic odontologist should construct a postmortem record, recording all extraoral and intraoral features, charting all teeth and restorations and pathology findings. If the dentist has antemortem radiographs, photographs, and other dental evidence, then the forensic odontologist should try to compare these with the postmortem evidence.
Fig. 2.3
Postmortem and antemortem dental records
2.3.1.1 Dental Records
Dental records can be located from family dentists or oral physicians. Thus, it is important for dentists to keep records. The records should be complete, including proper dental charting, radiographs, and photographs from the first visit through follow-ups.
Dental charting: The dental record is considered legal, admissible evidence in the arbitration of contended negligence or malpractice. In many instances, the dental record is the only means of identifying a deceased person. Dentists should have recorded all the information on charts and possible X-rays and models.
Four-quadrant system: Zsigmondy (Zsigmondy 1874) adopted the old system of dividing the teeth into four quadrants and using a system of angles:
|
8 7 6 5 4 3 2 1 Right
|
1 2 3 4 5 6 7 8 Left
|
|
8 7 6 5 4 3 2 1 Right
|
1 2 3 4 5 6 7 8 Left
|
-
1: central incisor
-
2: lateral incisor
-
3: canine
-
4: first premolar
-
5: second premolar
-
6: first molar
-
7: second molar
-
8: third molar
Universal system: The universal system is very simple in concept: Just number the 32 permanent teeth from 1 to 32. Starting with the third molar in the upper-right quadrant (tooth #1), the teeth are numbered around the arch, so the maxillary left third molar is tooth #16. One then goes down to the mandibular left third molar (#17) and numbers the teeth around the lower teeth, finishing with the mandibular right third molar (#32). The 20 primary teeth are coded alphabetically from A through T. The system must be memorized by rote. If using this system infrequently, it helps to remember that A, J, K, and T are the second molars (at the distal ends of the quadrants) and that E, F, O, and P are the central incisors. Since there are only five teeth per quadrant, one can generally visualize the other tooth codes.
FDI system: Most dentists are right-handed, so quadrant 1 (maxillary right) is closest to the dentist when examining a patient and is scored first, then the upper-left quadrant, then one down to the lower-left quadrant, finishing with teeth in the lower-right quadrant (Keiser-Nielsen 1971, p. 105). This means the upper-right side (quadrant 1) is the patient’s upper-right side. The Fédération Dentaire Internationale’s (FDI) description also suggests how to verbalize the system, namely, “The digits should be pronounced separately; thus, the permanent canines are teeth one-three, two-three, three-three, and four-three” (Keiser-Nielsen 1971, p. 1034). So much dental practice attention is spent on the permanent teeth that they are coded as quadrants 1 through 4. The principle is to use numbers 5 through 8 to code the four primary quadrants even though they develop first. This numerical oddity was the subject of considerable discussion by the FDI committee, but it was reasoned that “mainly because deciduous teeth function for such a short time in comparison with permanent teeth that the bulk of dental data to be collected and computerized in the future would obviously concern permanent teeth” (Keiser-Nielsen 1971, p. 1035).
Permanent teeth
|
18 17 16 15 14 13 12 11
|
21 22 23 24 25 26 27 28
|
|
48 47 46 45 44 43 42 41
|
31 32 33 34 35 36 37 38
|
Deciduous teeth
|
55 54 53 52 51
|
61 62 63 64 65
|
|
85 84 83 82 81
|
71 72 73 74 75
|
Photography (Hinchliffe 2007): Forensic odontologists take photos to provide evidence of clinical findings in dental identification, abuse, bite marks, and similar cases. It allows reconstruction for forensic odontologists and assists in illustrating findings to juries and dentists. It can be used to explore unsuspected findings by infrared, ultraviolet, and alternative light source photography. Photographs should be sharp, labeled, and with the ABFO No. 2 ruler (Fig. 2.4). Dental evidence photographs should be taken by forensic odontologists because they are specially trained in taking close-ups and collecting all evidence for dental identification.
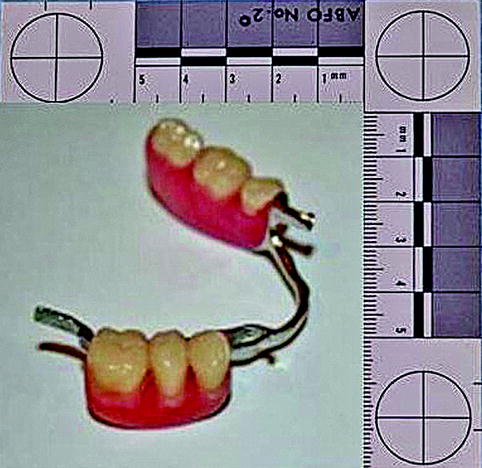
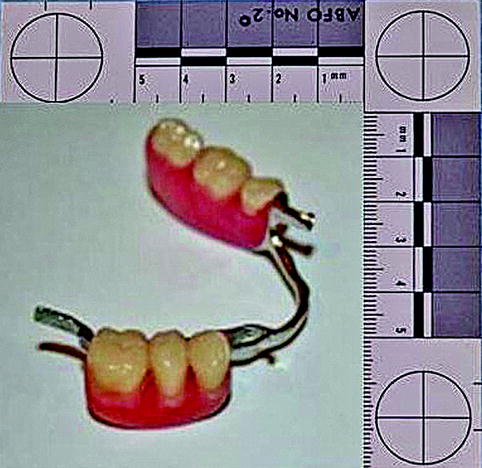
Fig. 2.4
Photograph with ABFO No. 2 ruler
Radiography (American Board of Forensic Odontology 2011): Radiographs are of principal importance in dental identification. The comparison of antemortem and postmortem radiographs is a major method of dental identification. Radiographs should be of high quality (Fig. 2.5). Digital radiography is an accepted method, whose image quality is equal to or better than conventional X-rays. With digital radiography technology, a digital sensor replaces the conventional film (Dölekogˇlu et al. 2011). Three types of sensor systems are commonly used in dentistry. Two types are known as charged-coupled devices (CCD), and the other one is known as a complementary metal oxide semiconductor sensor (CMOS). CCD systems are wireless systems connected to a computer. These technologies allow images to be loaded and viewed on a computer immediately. CMOS is an indirect system using a phosphor plate. It uses the plate to transfer the image from the subject to the plate-scanning device. These screens are reusable. Scanning electron microscopy and energy dispersion X-ray spectroscopy are useful in the recognition and discrimination of tooth materials from other materials. They are mainly useful in decomposed, incinerated, and bite mark analysis (Bush et al. 2008).
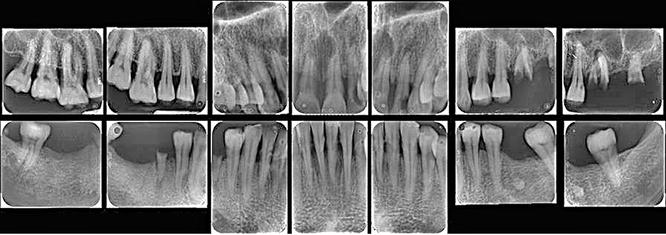
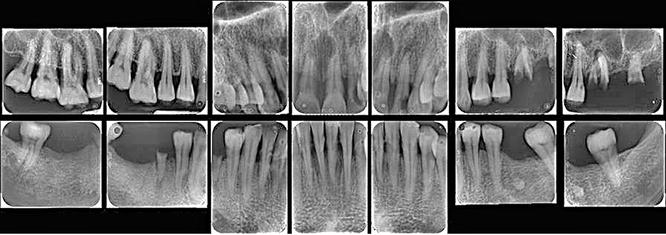
Fig. 2.5
Full mouth radiographic profile
Sources of antemortem identification (American Board of Forensic Odontology 2011) include ante-mortem records such as dental records, written records, and models. Photographs are then obtained from the dentist or oral physician. Collecting antemortem records is the responsibility of the investigating agency that has access to missing and other reports at the local, national, and international levels.
2.3.1.2 Charting, Records, and Databases (American Board of Forensic Odontology 2011)
Dental charting solves the problem of dental identification by giving the forensic odontologist antemortem charts, which can easily and quickly be interpreted into WinID, CAPMI, and Plassdata. Dentists’ shorthand, incomplete documentation, and different charting techniques are big problems for forensic odontologists when comparing antemortem and postmortem data. WinID (Fig. 2.6), CAPMI, or Plassdata charting (Figs. 2.7 and 2.8) should be used to solve this problem.
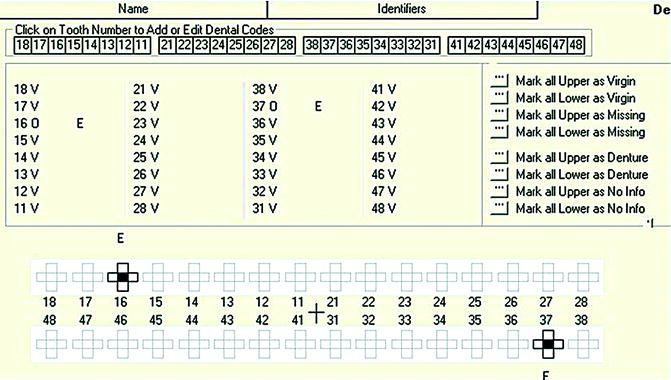
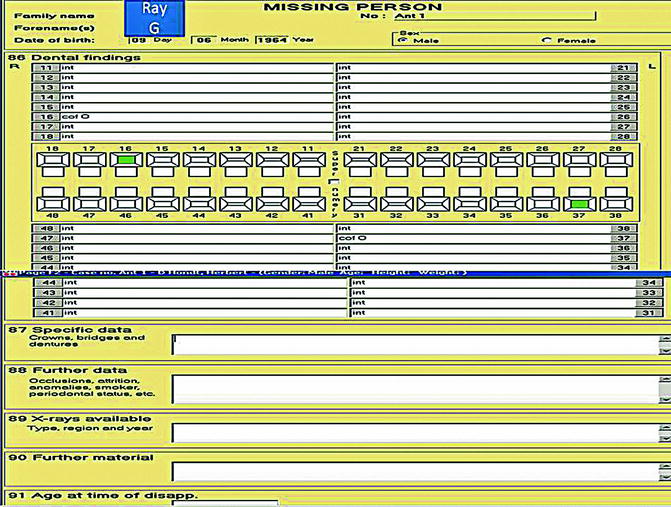
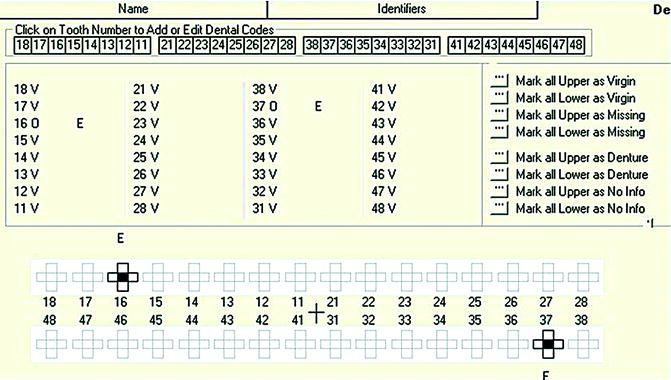
Fig. 2.6
WinID (antemortem)
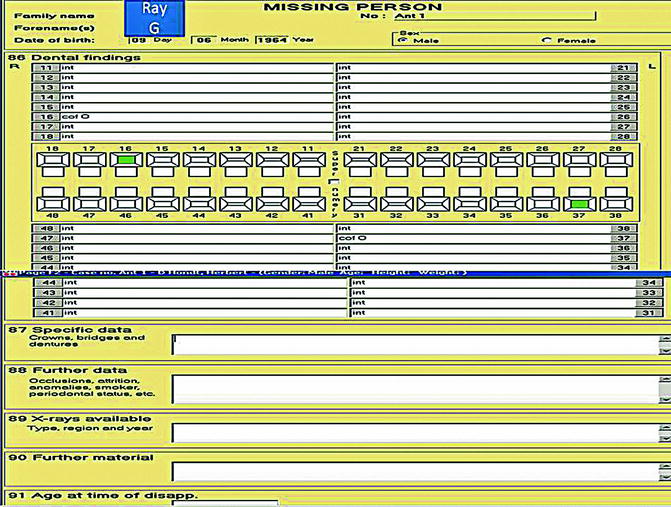
Fig. 2.7
Plassdata (antemortem)
Fig. 2.8
(a, b) Plassdata (postmortem)
Clinical records: Complete dental records must be maintained. The ability of clinical practitioners to produce and maintain good dental records is essential for good-quality patient care as well as being a legal obligation. Dentists have a role to play in keeping accurate dental records and providing all important information so that legal authorities may recognize malpractice, negligence, abuse, and identification of victims. In brief, a patient’s record includes a complete history, physical examination, diagnosis, treatment, and care (Lawrey 1998). The record may consist of different elements, including written notes, radiographs, study models, referral letters, consultants’ reports, clinical photographs, results of special investigations, drug prescriptions, laboratory prescriptions, patient identification information, and a comprehensive medical history. It is essential that a practitioner maintains this information in an easily accessible manner (Collins 1996). The production, retention, and release of clear and accurate patient records is an essential part of a dentist’s professional responsibility (Rai et al. 2006).
Content of patient’s record: The patient’s record consists of the history, physical examination, diagnosis, treatment, and care. The established minimum information in written notes should include (Lawrey 1998):
-
Identification data: Name, date of birth, address, phone numbers, and emergency contact information;
-
Medical history: Thorough investigation, to include a minimum of
-
Name and phone number of general physician
-
Dentist’s own evaluation of patient’s general health and appearance
-
List of systemic diseases, such as diabetes, rheumatic fever, hepatitis, etc.
-
Any ongoing medical treatment
-
Any bleeding disorders, drug allergies, smoking, and history of alcohol consumption
-
Any cardiac disorders
-
Relevant family medical history
-
Pregnancy
-
Physical and emotional tolerance for procedures
-
-
Dental history
-
Clinical examination, to include an accurate charting
-
Diagnosis
-
Treatment plan
-
Documentation of informed consent
How to create and maintain a patient’s record: Lawrey (1998) describes a simple ten-step procedure to ensure that patients’ records are adequate. A modified and expanded version, appropriate for the National Health Service, UK, is given below:
1.
Use a consistent style for entries: The appearance of the record is enhanced by using the same color and type of pen and the same abbreviations and notifications, etc.
2.
Date and explain any corrections: It may be a fatal error in a malpractice case if records appear doctored in any way. These unexplained corrections can undermine the credibility of the entire record and of the treating dentist.
3.
Do not use correction fluids: Not only is this messy, but it is conspicuous and may indicate that there has been an attempt to hide information.
4.
Use ink: Pencil can fade and opens up the question of whether or not the records have been altered.
5.
Use single line cross-out: This preserves the integrity of the record and shows that you have nothing to hide.
6.
Write legibly: An illegible record may be as bad as no record at all. Entries that are difficult to read can lead to guesswork by others, and this may not be favorable to you.
7.
Express concerns about patient needs: By doing this, one is documenting that one has listened, empathized, understood, and acted upon the wishes of the patient. It also enables an explanation to be given should a patient’s wishes be unobtainable or unrealistic and can help instantly diffuse a malpractice case.
8.
Never write derogatory remarks in the record: Superfluous entries only serve to convey a feeling of unprofessionalism and may give doubts to the overall credibility.
9.
Use only accepted abbreviations for treatments: This is helpful both in a malpractice situation and also when transferring records to a dentist for referral, to obtain prior approval, or to change the dentist of record.
10.
Maintain a chronological order: The use of a hole punch and metal retainer clips in the top of the record may be helpful to keep loose sheets organized.
Storing radiographs: The most common technique for radiograph storage is in a small envelope with the patient’s details, type of radiograph, and data listed on the front. The patient’s record can quickly become filled with these envelopes, and establishing a timeline can be difficult and confusing, especially when endodontic films become commingled with diagnostic films. A mounting method can be a more effective solution to radiograph storage. As well as the need for accurate, well-stored and documented radiographs, the frequency of radiographic examination is important. A patient’s record that is lacking up-to-date radiographs may jeopardize a malpractice case and is contrary to the patient’s best interest (Plunkett 1997).
Use computers to maintain records: Paper records and radiographs can simply be scanned into a personal computer using a desktop scanner. The most commonly used programs in forensic investigations are Adobe Photoshop 4.0 and Microsoft Program. By using these techniques, the dentist can protect him- or herself from malpractice claims without using valuable physical storage space.
The law concerning the length of time records must be stored varies from country to country, between 2 and 20 years, with 5–10 years in India, for example. Thus, each dentist has a responsibility to understand the forensic implications associated with the practice of his or her profession. This understanding should include more than ethics and jurisprudence, which were traditionally the only aspects of a dentist’s knowledge of the law. An appreciation of forensic dental problems permits clinicians to maintain legally acceptable records and to assist legal authorities in the identification of victims of disasters and crimes. Success in this task will assist the dentist should a medico-legal claim be made and can assist the police and crime detectors in the correct identification of individuals.
2.3.1.3 Types of Antemortem Records (American Board of Forensic Odontology 2011; Pretty and Sweet 2001)
Antemortem dental records consist of X-rays and dental charts, described in this section.
X-rays: X-rays are the most vital antemortem records. These are recovered and submitted in forensic investigations. The dentist should submit copies of the X-rays and keep the duplicates. The original film should be a better-quality X-ray than the duplicate. Bitewing, periapical, a full mouth series of X-rays (consists of periapical and bitewing X-rays), a Panoramic X-ray or lateral skull X-ray, CT scan, cone beam CT, and so forth are important tools. Scanned images of dental X-rays or a digital X-ray, saved as bitmap files, can be transmitted electronically when required.
Dental charts: The original dental chart should be obtained if possible. It can be very important, but the forensic odontologist should keep in mind that the original dentist may have made mistakes when filling out the chart. Therefore, X-rays are a much improved means of making a comparison.
If the dentist has kept dental models or casts, they can be very important in bite mark cases. Additionally, dentists commonly take photographs of their patients’ teeth to document their condition. Family snapshots, award receptions, graduations, weddings, or other ceremonial pictures may expose a smile. Dental appliances, such as partial dentures, bite splints, mouthguards, orthodontic retainers, or full dentures are also part of a forensic investigation.
The antemortem forensic record should be recorded in a layout that accurately shows the latest known status of that patient’s dental status (Table 2.2).
Table 2.2
Ethnic differences among three groups
|
Negroid
|
Mongoloid
|
Caucasoid
|
|
|---|---|---|---|
|
Cranial shape
|
Long
|
Broad
|
Medium
|
|
Nose shape
|
Broad
|
Medium
|
Narrow
|
|
Nasal bone size
|
Medium/small
|
Small
|
Large
|
|
Sagittal view
|
Highly variable, post bregmatic depression
|
High and globular
|
High and rounded
|
|
Nasal view
|
Straight to concave
|
Concave
|
Straight
|
|
Incisor shape
|
Blade
|
Blade
|
Shoveled
|
|
Facial profile
|
Extreme prognathism
|
Moderate prognathism
|
Reduced prognathism
|
|
Mandible
|
Gracile, oblique gonial angle
|
Robust
|
Medium
|
|
Chin shape
|
Median
|
Median
|
Bilateral
|
2.3.1.4 Procedures for Postmortem Dental Record Collections (American Board of Forensic Odontology 2011; Rφtzscher et al. 2004)
This section describes the appropriate procedures for postmortem dental record collection.
Examination of the oral tissues: A forensic odontologist can help find and identify dental remains that are decomposed, charred, or traumatically mutilated. A fragment of a tooth, a single tooth, or a jaw fragment may be vital to the identification. Postmortem head and neck X-rays (full body X-rays, CT scan) may find dislodged teeth or fragments. X-ray assessment of muck or charred debris may also help in finding the fragmentary evidence. Depending on the condition of the body, the precise procedures used for the identification may vary. A forensic odontologist may utilize the following techniques in processing a dental identification:
1.
Normal condition or visually identifiable.
(a)
A dental examination should be conducted if
1.
There are no reports of a missing individual or suspicions as to the identity.
2.
No personal effects are found.
3.
No fingerprints are done.
(b)
Dental examination should carry on with no mutilation to the face, that is, no resection or removal of the jaws.
(c)
Dental examination would comprise photographs of the teeth, a full mouth series of standard dental X-rays with a portable dental X-ray machine, dental charting, and dental impressions and cast construction (if possible).
2.
Completely decomposed or skeletonized.
(a)
Simple and easy to work with.
(b)
Some of the teeth will dislocate from sockets because the periodontal ligaments have been damaged in the breakdown process. All loose teeth should be recovered and replaced in their sockets.
(c)
Dental examination would comprise photographs of the teeth, a full mouth series of standard dental X-rays with a portable dental X-ray machine, dental charting, jaw articulation and occlusal analysis, and preservation of remains (if possible).
3.
Partially decomposed.
(a)
Difficult to examine due to the odor and presence of insects (e.g., maggots, flies, beetles, etc.).
(c)
Dental examination would comprise photographs of the teeth, a full mouth series of standard dental X-rays with a portable dental X-ray machine, dental charting, and preservation of remains (if possible).
4.
Burned.
(a)
Access to the teeth is very difficult, as the tissues are very rigid and fragile.
(b)
Jaws need to be resected.
(c)
Caution is recommended in resecting seriously burned or calcined jaws because they are extremely fragile. Fixation with clear acrylic spray is recommended.
(d)
Dental examination would comprise photographs of the teeth, a full mouth series of standard dental X-rays with a portable dental X-ray machine, dental charting, and preservation of remains (if possible).
5.
Mutilated or traumatized.
(a)
Teeth and jaws may be fragmented and distorted.
(b)
Recovery of all the teeth and teeth segments may be difficult.
(c)
Dental evidence may be imbedded in other areas of the body or scattered about the area.
(d)
Resection of both jaws.
1.
Generally, in cases of complex decomposition, severe mutilation, and bodies that are burned or burned beyond recognition, the jaws must be detached.
2.
Resection of the jaws must be accomplished if there is no open viewing of the body.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses