Oral lichen planus (OLP) is commonly found in middle-aged women. Although the cause is unknown, research points to several complex immunologic events and cells that are responsible for the inflammatory destruction and chronicity of these lesions. Biopsy for histologic diagnosis is recommended. The mainstay of treatment remains topical corticosteroids; however, newer therapies such as immunomodulating agents are available for recalcitrant lesions. In cases of lichenoid mucositis or reactions, treatment should be directed at identifying and removing the presumed cause. Given the apparent risk of squamous cell carcinoma in these patients, frequent follow-up and repeat biopsy are vital.
Key points
- •
Oral lichen planus and lichenoid reaction are a common oral mucosal disease process encountered in clinical practice.
- •
This mucocutaneous disease can manifest as desquamative gingivitis, asymptomatic Wickham striae or plaques, or severe, painful erosions or ulcerations anywhere in the oral cavity.
- •
Although the cause initiating lichen planus is unknown, current research points to several complex immunologic events and cells that are responsible for the inflammatory destruction and chronicity of these lesions.
- •
The mainstay of treatment remains topical corticosteroids; however, newer therapies such as tacrolimus are available for recalcitrant lesions. In cases of lichenoid mucositis or reactions, treatment should always be directed at identifying and removing the presumed cause.
- •
Given the apparent risk of squamous cell carcinoma in these patients, frequent follow-up and repeat biopsy when indicated are vital.
Introduction
Nature of Problem and Definition
Lichen planus (LP) is a common mucocutaneous disease affecting 1% to 2% of the population. Lesions most commonly occur on both oral and cutaneous surfaces (40%), followed by cutaneous alone (35%) and mucosa alone (25%). Oral LP (OLP) occurs in men and women, usually between the ages of 30 and 70 years. Children and adolescents are rarely affected.
Varying in its clinic appearance, OLP can appear keratotic (reticular or plaquelike) or erythematous and ulcerative, and is often accompanied by skin lesions ( Box 1 ). Spontaneous remission of cutaneous LP after 1 year occurs in approximately 70% of cases. On the other hand, spontaneous remission of OLP is less common, occurring in less than 5% of patients over a 7.5-year follow-up. The reticular form of OLP has the best prognosis, because spontaneous remission occurs in 40% of cases. The reported mean duration of OLP is 5 years, but the erosive form of the disease can persist for up to 15 to 20 years.
Prevalence/Incidence
In the literature, different prevalence figures for OLP have been reported and vary from 0.5% to 2.2%. These figures may represent an underestimation, because minor lesions may easily be overlooked. The proportion of women is higher than men among referred patients, but this may not be accurate in the general population. The mean age of the time of diagnosis is 55 years.
Cause and Pathogenesis
The cause of LP remains unclear. Research exploring the pathogenesis of LP has yielded many data suggesting that immunologic mechanisms are fundamental to the initiation and perpetuation of LP ( Box 2 ). Primarily, focus has been given to the role of the epithelial antigenic processing macrophage, the Langerhans cell, the mast cell, and their interactions with the abundant T-cell population accumulated in the underlying connective tissue.
- •
Immunomarker studies have disclosed that the lymphocyte population is exclusively T cell in nature, with a mixture of CD4 and CD8 lymphocytes that express integrin molecules of the α 1 class
- ○
These integrin ligands bind to other adhesion molecules that are upregulated on endothelial cells (vascular cell adhesion molecule) and (intercellular adhesion molecule)
- ○
- •
Lower strata keratinocytes are able to present antigens to cells bearing the CD4-associated T-cell receptor
- •
CD8 lymphocytes are able to bind to antigen-complexed major histocompatibility complex I molecules on keratinoctyes
- •
Fibronectin, laminin, and types IV and VII collagens are upregulated in the basement membrane
- •
Angiogenesis and vasodilation are increased in lesional submucosa
- •
In the inflamed epithelium, lower strata keratinocytes express and secrete chemokines that are chemotactic to lymphocytes
- •
Reactive T cells leave submucosal vessels and enter the connective tissues
- •
Chemokines from keratinocytes direct lymphocyte traffic along extracellular matrix (ECM) using cell-matrix adhesion molecules
- •
Cytotoxic T cells release perforin and other enzymes, which lyse basal cells, particularly in the erosive form of the disease
- •
After antigenic challenge, lymphocytes adhering to vascular endothelia emigrate into the submucosa, migrating under the influence of the epithelial secreted chemoattractant molecules
- •
Lymphocytes are then able to adhere to ECM molecules, which are overproduced along the basement membrane
- •
On crossing the epithelial-mesenchymal interface, ECM molecules are able to bind, via integrins, to cell-surface adhesion molecules pathologically expressed on keratinocytes
Current evidence suggests that LP is a T-cell–mediated process. Lesional LP tissue shows massive local activated T-cell populations, with increased local expression of cytokines and altered adhesion molecule expression. In addition, therapies that suppress cell-mediated immune responses reduce the lymphocyte infiltrate and cause clinical improvement of LP lesions. Other evidence supporting the immunologic pathogenesis of LP includes the deposition of fibrinogen along the basement membrane and the cell-mediated autoimmune destruction of basal keratinocytes.
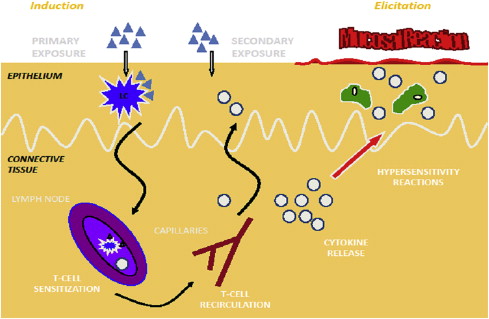
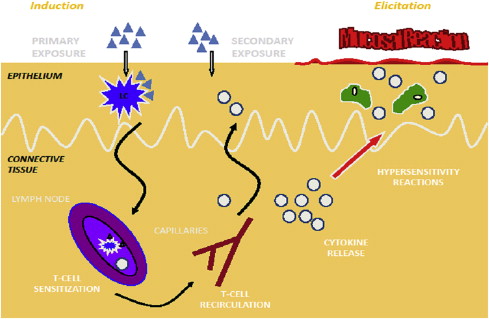
Antigenic challenge may come from the external environment or may be the result of keratinocyte autoantigen expression. Dendritic Langerhans cells and antigen-bearing class II molecules on keratinocytes relay molecular information to reactive CD4 cells in the regional lymph nodes, which engender an effector T helper cell (Th1) pathway response, leading to a mucosal or cutaneous eruption. The cellular response is similar to that seen in a contact allergic reaction or delayed-type hypersensitivity reaction ( Fig. 1 ).
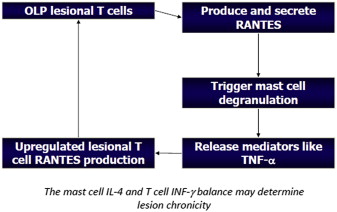
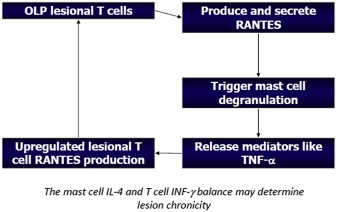
The chronicity of OLP is significantly greater than its cutaneous counterpart. Although the precise nature of this discrepancy has not been elucidated, some evidence supports the role of T-cell RANTES (regulated upon activation, normal T-cell expressed and secreted) and mast cell degranulation, leading to the release of tumor necrosis factor α and a cyclical process, where interleukin 4 and interferon γ may predict the chronicity of the disease process in some cases ( Fig. 2 ).
Symptoms
The red, inflamed lesions and open sores of OLP can cause a burning sensation or pain. The white, lacy patches may not cause discomfort when they appear on the buccal mucosa but may be painful when they involve the tongue. Most lacy white lesions cause patients to describe a rough sensation of the affected surfaces. Lesions most commonly occur on both oral and cutaneous surfaces (40%), followed by cutaneous alone (35%) and mucosa alone (25%).
The most common presenting symptoms are:
- •
Erythematous and desquamative gingivae
- •
Oral pain and soreness, exacerbated with acidic and spicy foods
- •
Ulceration
- •
Bleeding and irritation with tooth brushing
- •
Change in taste or a blunted taste sensation if the tongue is affected
- •
Sensitivity to hot, acidic, or spicy foods
Introduction
Nature of Problem and Definition
Lichen planus (LP) is a common mucocutaneous disease affecting 1% to 2% of the population. Lesions most commonly occur on both oral and cutaneous surfaces (40%), followed by cutaneous alone (35%) and mucosa alone (25%). Oral LP (OLP) occurs in men and women, usually between the ages of 30 and 70 years. Children and adolescents are rarely affected.
Varying in its clinic appearance, OLP can appear keratotic (reticular or plaquelike) or erythematous and ulcerative, and is often accompanied by skin lesions ( Box 1 ). Spontaneous remission of cutaneous LP after 1 year occurs in approximately 70% of cases. On the other hand, spontaneous remission of OLP is less common, occurring in less than 5% of patients over a 7.5-year follow-up. The reticular form of OLP has the best prognosis, because spontaneous remission occurs in 40% of cases. The reported mean duration of OLP is 5 years, but the erosive form of the disease can persist for up to 15 to 20 years.
Prevalence/Incidence
In the literature, different prevalence figures for OLP have been reported and vary from 0.5% to 2.2%. These figures may represent an underestimation, because minor lesions may easily be overlooked. The proportion of women is higher than men among referred patients, but this may not be accurate in the general population. The mean age of the time of diagnosis is 55 years.
Cause and Pathogenesis
The cause of LP remains unclear. Research exploring the pathogenesis of LP has yielded many data suggesting that immunologic mechanisms are fundamental to the initiation and perpetuation of LP ( Box 2 ). Primarily, focus has been given to the role of the epithelial antigenic processing macrophage, the Langerhans cell, the mast cell, and their interactions with the abundant T-cell population accumulated in the underlying connective tissue.
- •
Immunomarker studies have disclosed that the lymphocyte population is exclusively T cell in nature, with a mixture of CD4 and CD8 lymphocytes that express integrin molecules of the α 1 class
- ○
These integrin ligands bind to other adhesion molecules that are upregulated on endothelial cells (vascular cell adhesion molecule) and (intercellular adhesion molecule)
- ○
- •
Lower strata keratinocytes are able to present antigens to cells bearing the CD4-associated T-cell receptor
- •
CD8 lymphocytes are able to bind to antigen-complexed major histocompatibility complex I molecules on keratinoctyes
- •
Fibronectin, laminin, and types IV and VII collagens are upregulated in the basement membrane
- •
Angiogenesis and vasodilation are increased in lesional submucosa
- •
In the inflamed epithelium, lower strata keratinocytes express and secrete chemokines that are chemotactic to lymphocytes
- •
Reactive T cells leave submucosal vessels and enter the connective tissues
- •
Chemokines from keratinocytes direct lymphocyte traffic along extracellular matrix (ECM) using cell-matrix adhesion molecules
- •
Cytotoxic T cells release perforin and other enzymes, which lyse basal cells, particularly in the erosive form of the disease
- •
After antigenic challenge, lymphocytes adhering to vascular endothelia emigrate into the submucosa, migrating under the influence of the epithelial secreted chemoattractant molecules
- •
Lymphocytes are then able to adhere to ECM molecules, which are overproduced along the basement membrane
- •
On crossing the epithelial-mesenchymal interface, ECM molecules are able to bind, via integrins, to cell-surface adhesion molecules pathologically expressed on keratinocytes
Current evidence suggests that LP is a T-cell–mediated process. Lesional LP tissue shows massive local activated T-cell populations, with increased local expression of cytokines and altered adhesion molecule expression. In addition, therapies that suppress cell-mediated immune responses reduce the lymphocyte infiltrate and cause clinical improvement of LP lesions. Other evidence supporting the immunologic pathogenesis of LP includes the deposition of fibrinogen along the basement membrane and the cell-mediated autoimmune destruction of basal keratinocytes.
Antigenic challenge may come from the external environment or may be the result of keratinocyte autoantigen expression. Dendritic Langerhans cells and antigen-bearing class II molecules on keratinocytes relay molecular information to reactive CD4 cells in the regional lymph nodes, which engender an effector T helper cell (Th1) pathway response, leading to a mucosal or cutaneous eruption. The cellular response is similar to that seen in a contact allergic reaction or delayed-type hypersensitivity reaction ( Fig. 1 ).
The chronicity of OLP is significantly greater than its cutaneous counterpart. Although the precise nature of this discrepancy has not been elucidated, some evidence supports the role of T-cell RANTES (regulated upon activation, normal T-cell expressed and secreted) and mast cell degranulation, leading to the release of tumor necrosis factor α and a cyclical process, where interleukin 4 and interferon γ may predict the chronicity of the disease process in some cases ( Fig. 2 ).
Symptoms
The red, inflamed lesions and open sores of OLP can cause a burning sensation or pain. The white, lacy patches may not cause discomfort when they appear on the buccal mucosa but may be painful when they involve the tongue. Most lacy white lesions cause patients to describe a rough sensation of the affected surfaces. Lesions most commonly occur on both oral and cutaneous surfaces (40%), followed by cutaneous alone (35%) and mucosa alone (25%).
The most common presenting symptoms are:
- •
Erythematous and desquamative gingivae
- •
Oral pain and soreness, exacerbated with acidic and spicy foods
- •
Ulceration
- •
Bleeding and irritation with tooth brushing
- •
Change in taste or a blunted taste sensation if the tongue is affected
- •
Sensitivity to hot, acidic, or spicy foods
Clinical findings
Physical Examination
A thorough history is vital in arriving at a definitive diagnosis and should include a thorough history of present illness with previous treatments listed, a detailed past medical history, a complete list of current medications, and a thorough review of systems. An exhaustive extraoral and intraoral examination should be performed after a detailed history.
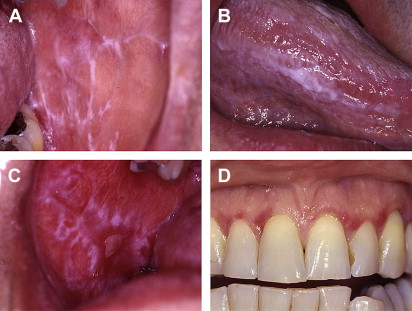
LP has a wide range of clinical appearances, which correlate well with disease severity. Four distinct clinical presentations are most often described: reticular, erosive, plaquelike, and bullous. Often, patients have a combination of the reticular and erosive forms, whereas plaquelike LP usually occurs as a solitary white plaque resembling leukoplakia and not in combination with other forms ( Fig. 3 , Table 1 ).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


