Introduction
In the last decade, an increasing number of studies focusing on the impact of oral deformities and illnesses on quality of life have been published. Our goal was to evaluate the impact of oral problems on quality of life in 3 groups of adult patients in need of orthognathic-surgical treatment.
Methods
A total of 117 patients were recruited from the Clinic of Oral and Maxillofacial Surgery of the State University of Rio de Janeiro in Brazil: 20 in the initial phase, 70 in the presurgical phase (presurgical orthodontic preparation), and 27 in the postsurgical phase. The impact of treatment phase on oral health-related quality of life was evaluated with the oral health impact profile (OHIP-14). OHIP-14 scores were calculated by an additive method, and the participants were divided on the basis of level of impact into 2 groups: high impact (scores, >11) and low impact (scores, ≤11).
Results
Compared with patients in the postsurgical phase, those who needed orthognathic surgical treatment but had not yet begun it and those who were in the presurgical phase of treatment were 6.48 and 3.14 times more likely, respectively, to experience a negative impact of their oral condition.
Conclusions
Among those undergoing or anticipating orthognathic-surgical treatment, orthognathic surgery positively affects the patients’ quality of life.
In 1976, when sociodental outcomes were being adopted to evaluate the impact of oral problems on people’s lives, Cohen and Jago pointed out that, among all oral disorders, malocclusions are the most difficult to measure. This is basically because the diagnosis implies considerations that involve both professional views regarding deviations from “normal” occlusion and cultural values that influence body image and esthetic knowledge. The possible psychological repercussions and the effects of dentofacial deformities and their treatment on body image have been the subject of numerous studies. Garcia-Rodriguez et al, in a prospective study about some psychological aspects of adults with severe dentofacial deformities treated by orthognathic surgery, assessed the body image of surgical patients before and after treatment. The results showed that, despite the severity of the dentofacial deformity, presurgical mean scores of both subscales of a body image test were normal. On the other hand, longitudinal research by Kiyak et al reported significant improvements in body image after conventional and surgical orthodontics, particularly self-evaluations of facial and dental appearance. In addition, several retrospective studies have identified the psychological benefits of orthognathic surgery, including improvements in interpersonal skills, self-confidence, and positive life changes, such as in personal relationships. Kiyak et al studied the psychological impact of orthognathic surgery 9 and 24 months after surgery. The results highlighted the importance of completing postsurgical orthodontic treatment within 6 months after surgery and maintaining contact with orthognathic surgery patients for at least 2 years after surgery. Another study reported improvements in oral health-related quality of life (OHRQOL) and psychosocial function 2 years after surgical mandibular advancement in patients with Class II malocclusion.
Even though demand for orthodontic treatment is mostly related to personal concern about appearance and other psychosocial factors, measures of orthodontic need and outcomes of orthodontic treatment place relatively little emphasis on patients’ perceptions of need and the differences that orthodontic care would bring to their OHRQOL. The relationships between objective orthodontic indexes and patients’ perceptions of their own appearance and oral health status have been studied. It is important to understand the patient’s perceptions because they are central to the assessment of overall need and satisfaction with treatment. Primarily because of this concern, several OHRQOL measures have been developed to assess the impact of the mouth on quality of life. Subjective indexes to measure OHRQOL might be useful for practical, political, and theoretical purposes. Such measures have been increasingly used in various countries, since they add important complementary information to traditional oral health indexes.
The oral health impact profile (OHIP) was developed by Slade and Spencer to measure the dysfunction, discomfort, and disability attributed to oral conditions in older adults and elderly populations. A short form consisting of 14 items (OHIP-14), 2 of each dimension, was developed by Slade and translated into several languages. The Brazilian version of the OHIP-14 showed psychometric properties similar to those of the original questionnaire.
In this study, we aimed to evaluate the impact of oral health related problems on quality of life in young adults with dentofacial deformities, using the OHIP-14. Patients in 3 distinct phases of the treatment were assessed: initial stages, before any orthodontic procedures; presurgical, having completed orthodontic preparation for the surgery; and postsurgical, after surgery but still receiving orthodontic treatment.
Material and methods
This report describes the findings of research carried out at the Clinic of Oral and Maxillofacial Surgery of the State University of Rio de Janeiro (HUPE) and approved by its Committee of Research Ethics. The participants were 20 patients who had consulted with the HUPE regarding orthognathic-surgical treatment, without having had any previous orthodontic or surgical treatment (the initial group), 70 patients who were currently in presurgical orthodontic treatment (presurgical group), and 27 patients who had completed orthognathic surgery and presurgical orthodontic treatment but were still in postsurgical orthodontic treatment (postsurgical group). They were not selected on the basis of gender, race, age, or any type of malocclusion. This sample was obtained by a process of nonprobabilistic selection from persons eligible for examination in the Clinic of Oral and Maxillofacial Surgery of the HUPE from January to March 2006, based on the following criteria: those in the initial group had no previous orthodontic treatment in the past, initial and presurgery patients had no previous orthognathic surgery, treatment could be provided by the orthodontics clinic of HUPE or by a dental professional of any other institution, and the postsurgery group comprised patients from the Oral and Maxillofacial Surgery Clinic of Pedro Ernesto University Hospital, Rio de Janeiro, Brazil, at least 4 weeks after surgery.
Potential participants were contacted personally by staff of the Clinic of Oral and Maxillofacial Surgery during routine appointments. Sociodemographic information and other relevant facts for the impact of OHRQOL problems were obtained from a self-administered questionnaire. Before completing the questionnaires, instructions were given regarding the work, and questions were answered; participants were guided to answer on their own and to ask if they had questions. As part of their participation in this study, patients from the initial group received a dental evaluation and instructions about the orthognathic-surgical treatment after filling out the questionnaire.
To characterize the study population regarding economic status, the Brazil Economic Classification Criteria developed by the Brazilian Association of Advertisers was used. The collected data refer to the level of education of the head of the family, essential assets, essential goods, monthly salary of their home employees, and vehicles.
OHRQOL was assessed with the Brazilian version of the OHIP-14. The original OHIP consists of 49 items organized into 7 subscales: functional limitation, physical pain, psychological discomfort, physical disability, psychological disability, social disability, and handicap. The subscales are based on a conceptual framework suggested by Locker and derived from the World Health Organization’s International Classification of Impairments, Disabilities and Handicaps. A pretest was carried out with 30 patients to evaluate whether the OHIP-14 questions were fully understood by the participants, and whether any terms or expressions required replacement. The patients had been instructed to answer the OHIP-14 questions, taking into account their experiences regarding teeth, mouth, or dentures, during the 6 months preceding this assessment. The postsurgical patients were also instructed to consider the impact of surgery on their OHIP-14 responses.
Statistical analysis
The results of this research were tabulated in a statistical program (version 9, StataCorp, College Station, Tex), with bivariate and multivariate analyses (chi-square and Student t tests, and simple and multiple logistic regressions).
OHIP-14 scores were obtained by adding the responses to all 14 items, ranging from never (0 point), hardly ever (1 point), occasionally (2 points), fairly often (3 points), and very often (4 points). As a result, total scores could range from 0 to 56 points. Because of the skewed distribution of the values of OHIP-14, the sample was divided into 2 groups by using the median value: the high-impact group had scores >11, and the low-impact group had scores ≤11. All subsequent analyses testing the association between OHRQOL, phase of treatment, and sociodemographic variables were based on this median split.
The frequency of answers in each of the 7 dimensions of the OHIP-14 was evaluated, with those who replied “very often” or “fairly often” representing the high-impact group and all others the low-impact group. Thus, the subjects who had chosen, in each dimension, the options “never,” “hardly ever,” and “occasionally” were placed in the low-impact group, and those who had selected “fairly often” and “very often” comprised the high-impact group. Internal consistency of the scale was assessed with the Cronbach alpha coefficient.
Results
As stated earlier, 20 (17%) of the participants were in the initial group, 70 (60%) in the presurgery group, and 27 (23%) in the postsurgery group. The sample consisted mostly of single, unmarried subjects (83%); only 20 (17%) were married or divorced. They were also more likely to be female (55.6%). According to the Brazil Economic Classification Criteria, those who belonged to economic classes B (n = 49, 41.8%) and C (n = 46, 39.3%) represented the majority of this sample. The 3 groups did not differ in these sociodemographic characteristics, as shown in Table I .
| OHIP ≤11 | OHIP >11 | Total | ||||||
|---|---|---|---|---|---|---|---|---|
| P ∗ | n | (%) | n | (%) | n | (%) | ||
| Economic status | Class A | 0.86 | 7 | (58.3) | 5 | (41.7) | 12 | (100) |
| Class B | 25 | (51.1) | 24 | (48.9) | 49 | (100) | ||
| Class C | 23 | (50.0) | 23 | (50.0) | 46 | (100) | ||
| Class D | 4 | (40.0) | 6 | (60.0) | 10 | (100) | ||
| Marital status | Single | 0.71 | 48 | (49.4) | 49 | (50.6) | 97 | (100) |
| Married | 7 | (50.0) | 7 | (50.0) | 14 | (100) | ||
| Divorced | 4 | (66.7) | 2 | (33.3) | 6 | (100) | ||
| Gender | Male | 0.07 | 31 | (59.6) | 21 | (40.4) | 52 | (100) |
| Female | 28 | (43.1) | 37 | (56.9) | 65 | (100) | ||
| Treatment stage | Initial | 0.02 | 6 | (30.0) | 14 | (70.0) | 20 | (100) |
| Presurgery | 34 | (48.6) | 36 | (51.4) | 70 | (100) | ||
| Postsurgery | 19 | (70.4) | 8 | (29.6) | 27 | (100) | ||
| Age (y) (mean ± SE) † | 0.85 | 24.4 ± 0.98 | 24.6 ± 0.92 | 24.5±0.67 | ||||
| Total | 59 | (50.4) | 58 | (49.6) | 117 | (100) | ||
Internal consistency for the OHIP-14 was high (Cronbach’s coefficient α = 0.88; lower limit 95% CI, 0.90).
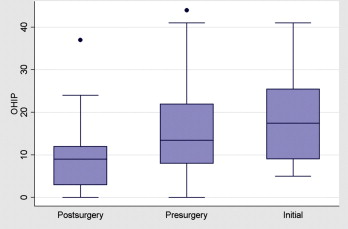
The OHIP-14 total scores from all participants varied between 0 and 45, with no standard pattern of distribution. There was a tendency of scores to decline from the initial to the presurgical groups, and from the presurgical to the postsurgical groups ( Fig ). The OHIP-14 mean value was 14.7 (SD, 10.4) for the total sample, with a median value of 11 (95% CI, 8.5-13.5). Among all variables of interest in this study (ie, economic status, marital status, gender, phase of treatment), only phase of treatment was significantly related to OHRQOL. That is, patients who reported high impact on the OHIP-14 were most likely to be in the presurgery or the initial phase group ( Table I ). The only sociodemographic variable with a P value <0.20 was gender, so it was included in the multivariate analysis to evaluate the strong association between high impact and phase of treatment ( Table II ).

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


