It is clear that the dental profession has entered a new age of radiographic diagnostic imaging. A number of examples have shown that being able to visualize oral and maxillofacial pathologic entities in three dimensions assists in diagnosing and planning the appropriate treatment. The technology is an improvement for our profession and for the patients it serves.
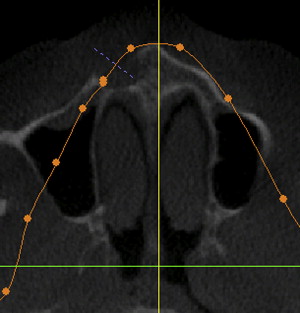
When pathologic lesions of the jaws are evaluated, a certain amount of information is gathered that is then distilled into the fabrication of a presumptive diagnosis, before surgical intervention (if that is necessary). Demographic information (age, sex, and race) is harvested. Patients are asked if they have certain complaints (pain, altered sensation, or anesthesia), or not. The facial structures are clinically examined for discolorations, depressions, swellings, and asymmetries. Laboratory studies may be indicated and ordered. And then, radiographic tools are used to evaluate that which we cannot see beneath the skin. The exposed images are examined, looking for the lesion’s exact location (maxilla, mandible, anterior, posterior, alveolar process, and so forth). The exact size of the defect and its relative density (radiolucent or radiopaque or a combination) are determined.
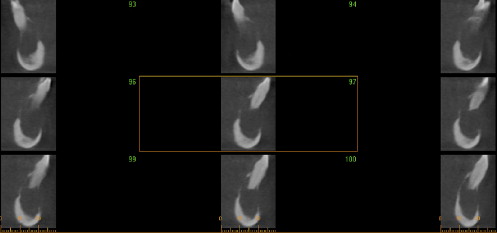
Information about potential aggressiveness is sought. Does the lesion expand the cortex? Does it thin it or perforate it? Is it unilocular or multilocular? Is it unifocal or multifocal? What are the characteristics of the border? Is it smooth, ragged, or can one even discern a border. Are teeth involved? Are they impacted or have they been displaced? Have the roots been resorbed? To perfect an accurate diagnosis, these are the questions that must be answered. This will be facilitated by gathering as much information as possible. In general, the greater its quality, the better will be the diagnosis.
Plain film radiography
During the past 4 decades, dentistry has seen a dramatic expansion and refinement of the technology used to identify dental and intraosseous disorders. Whereas the profession had always depended on intraoral radiographs (primarily periapical bite wings and occlusals), during the 1960s, commercially available extraoral panoramic radiography became available for use in the dental office. This introduction allowed the practitioner to gain much more information about the teeth and jaws, especially if surgical intervention was being contemplated. During the next 40 years, the main advances were seen in improvement of film stock and techniques to shorten the time of exposure and thereby the absorbed dose of irradiation. The current advanced state of intraoral and panoramic radiography is highlighted by the replacement of film-based image capture by digital imaging.
During this time frame (and previously as well), when there was a need for more information, patients had to be sent to private or hospital-based medical radiology centers so that more major extraoral facial or skull x-rays could be taken. Examples of films that were routinely ordered are posteroanterior and oblique skull and jaws views, Townes and reverse Townes views, submentovertex and specific exposures of the paranasal sinuses, and tomograms.
With the introduction of tomography, diagnosticians were given an additional tool to evaluate lesions, the ability to look at an object in three dimensions. These films had an advantage over panoramic x-rays since distortion was not as prevalent as is seen in the latter. However, similar to panoramic radiography, the problem of image magnification persisted.
Digital radiography
Then in the 1980s computed tomograms (CTs) became available and many of the films that had been previously taken for evaluation of the facial skeleton began to fade from use. There is little question that at this point, CT is the standard for maxillofacial hard tissue evaluation. However, within the dental community, with the exception of major pathology or trauma, there was a hesitancy to use this technology. This was understandable because (1) patients had to be sent out of the office to have the studies performed; (2) there were large doses of irradiation for the patient; (3) the medical radiologist did not always appreciate the information that the dental practitioner was seeking; (4) there was a variable lag time between the patient being sent and the practitioner receiving the information; and (5) the scans were expensive. In addition, most dentists did not have the training or experience necessary to read and properly evaluate the radiographic work product that they received.
This changed at the beginning of the current century when the first cone beam computed tomography (CBCT) machines for dental office use became commercially available. These machines have created a new paradigm for the evaluation of dental and maxillofacial structures in the ambulatory setting. The units are much smaller than the medical CTs, are less expensive to purchase and operate, produce a fraction of the radiation dose, and possess an open architecture that, generally, eliminates patient complaints of claustrophobia.
Most of the CBCT machines are structured so that the patient either sits or stands during the exposure, similar to what dental patients have been accustomed to in the past. This differs from virtually all medical CT units in which the patient must assume a supine position. Patients are therefore more comfortable and accepting of the CBCT designs. In addition, because the patient is positioned in a relatively natural head position, the temporomandibular joints can be more accurately evaluated.
Digital radiography
Then in the 1980s computed tomograms (CTs) became available and many of the films that had been previously taken for evaluation of the facial skeleton began to fade from use. There is little question that at this point, CT is the standard for maxillofacial hard tissue evaluation. However, within the dental community, with the exception of major pathology or trauma, there was a hesitancy to use this technology. This was understandable because (1) patients had to be sent out of the office to have the studies performed; (2) there were large doses of irradiation for the patient; (3) the medical radiologist did not always appreciate the information that the dental practitioner was seeking; (4) there was a variable lag time between the patient being sent and the practitioner receiving the information; and (5) the scans were expensive. In addition, most dentists did not have the training or experience necessary to read and properly evaluate the radiographic work product that they received.
This changed at the beginning of the current century when the first cone beam computed tomography (CBCT) machines for dental office use became commercially available. These machines have created a new paradigm for the evaluation of dental and maxillofacial structures in the ambulatory setting. The units are much smaller than the medical CTs, are less expensive to purchase and operate, produce a fraction of the radiation dose, and possess an open architecture that, generally, eliminates patient complaints of claustrophobia.
Most of the CBCT machines are structured so that the patient either sits or stands during the exposure, similar to what dental patients have been accustomed to in the past. This differs from virtually all medical CT units in which the patient must assume a supine position. Patients are therefore more comfortable and accepting of the CBCT designs. In addition, because the patient is positioned in a relatively natural head position, the temporomandibular joints can be more accurately evaluated.
Cone beam computed tomography compared with plain film tomography
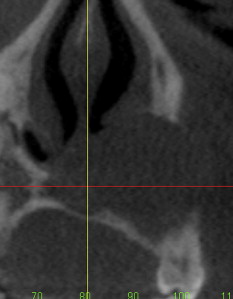
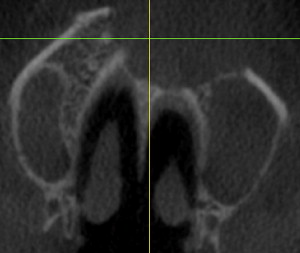
As compared with plain film tomograms, CBCT technology requires less time for the images to be captured, which is useful for patients who are not comfortable or are unable to keep still. In addition, the images generated via CBCT are less distorted and give the practitioner a better understanding of the density of the bone being imaged.
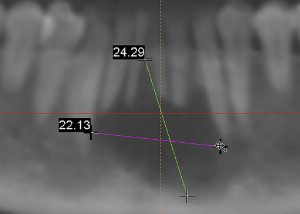
Cone beam computed tomography compared with panoramic radiography
While panoramic radiography has been the workhorse for most dental and oral and maxillofacial surgery practices, the images generated do have some shortcomings. Only flat, two dimensional, supero-inferior or postero-anterior images are created. And, as is typical with plain film radiography, panoramic x-rays suffer from superimposition of all structures that lie in the path between the x-ray source and the film or detector. CBCT allows these anatomic entities to be viewed in three dimensions and be included or excluded in the final image by simple digital manipulation. Furthermore, panoramic images are both distorted and magnified, which means that unreliable results are produced when measuring distance on panoramic x-rays, even when the magnification factor is known. Another advantage of CBCT is that it creates images that are both dimensionally faithful as well as anatomically accurate.
CBCT can also be teamed with stereolithographic model construction, which can be used in conjunction with dental implant placement or in the reconstruction of jaws resected due to pathology.
Cone beam computed tomography use in dentistry
CBCT technology allows the dental practitioner to virtually immediately, in her or his office, evaluate patients for a wide variety of maladies, ranging from dental and jaw trauma and infections, edentulism (quantitative and qualitative osseous evaluation for dental implants), temporomandibular joint osseous pathology, impacted and supernumerary teeth, developmental and congenital jaw deformities, dental endodontic lesions, and oral and maxillofacial pathology.
It is clear that CBCT is an imaging modality that is becoming an integral part of many dental practices. While much of the early focus has been on its use in dental implantology, it has proven to be a valuable asset in the diagnostic assessment of oral and maxillofacial pathology. The remainder of this article will focus on examples of common as well as some rarely encountered lesions.
Case studies
There is no better way to illustrate the utility of cone beam computed radiography than to demonstrate a variety of oral and maxillofacial pathology cases in which its use assists in the diagnosis and helps to guide the treatment. Viewing the disease processes in three dimensions provides the practitioner with a more global view of their pathogenesis and extent.
Case 1
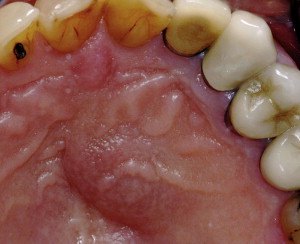
Clinical Correlation: The lesion was excised and biopsied Figs. 1–3 . Apicoectomy with root end restoration and grafting of the site was accomplished.

Diagnosis: Periapical radicular cyst.
Case 2
Clinical Correlation: The lesion was excised and biopsied Figs. 4–7 . Apicoectomy of the maxillary left central incisor followed by grafting the defect with 4 mL of allogeneic bone was performed.
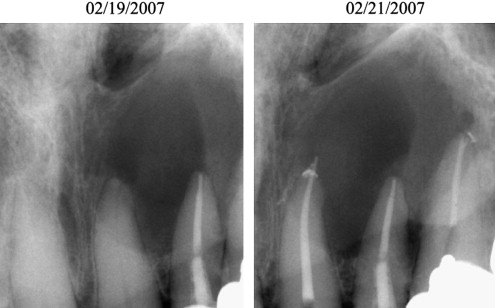
Diagnosis: Periapical radicular cyst.
Case 3
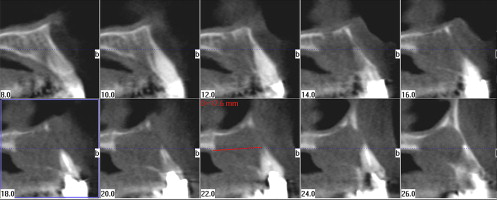
Clinical Correlation: The teeth were nonmobile and the teeth within the lesion all tested vital Figs. 8 and 9 . A deep bone biopsy was performed along with an extensive curettage of the lesion. Once the histologic diagnosis was made, the patient was advised of the necessity to perform additional surgery, including removal of some of the teeth, which would prevent adequate excision if left. The patient refused, and on follow-up 10 months later, recurrence was noted.
Diagnosis: Central giant cell granuloma, mandible.
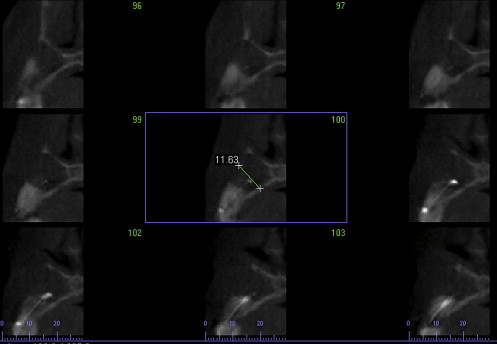
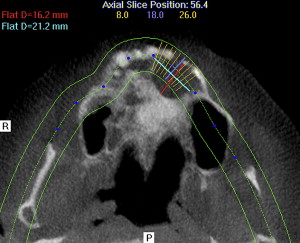
Case 4
Clinical Correlation: Teeth #9 and 10 were nonvital Figs. 10–13 . Aspiration of the lesion revealed a solid mass. There was no aspiration of blood or purulence. The patient refused treatment at the time. At a later date, her lesion was biopsied by a colleague who informed me of the diagnosis.