Chapter 7 Obstructive sleep apnea: decision making and treatment algorithm
1 INTRODUCTION
Numerous treatment options for obstructive sleep apnea (OSA) presently exist. These treatments range from non-invasive behavioral modifications to nightly use of positive airway pressure (PAP) devices to surgical treatments that alter airway anatomy. Selection of patients for these treatments is complex given the range of variability in patient anatomy and physiology, patient preference, disease severity, and controversy with regard to the effectiveness of available treatments. The threshold for treatment is also in flux with some arguing that symptoms of sleepiness are more important than measured disease severity in most patients.1 What can result from this is a confusing array of treatment options and treatment guidelines which leave patients and physicians unsure as to what decision is most appropriate for the individual. This chapter seeks to provide a framework for these issues and a guide for synthesis and evaluation of treatment options in this disease.
2 DEFINITIONS OF DISEASE
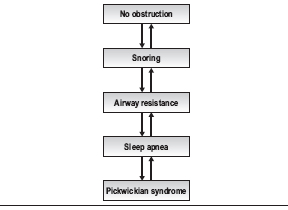
Sleep-disordered breathing can be viewed as a continuum from normal non-obstructed breathing at one end to a patient with sleep apnea and Pickwickian syndrome at the other (Table 7.1). The level of disease in an individual patient can improve or worsen, moving the patient up or down this continuum both over time and on a night-to-night basis. For instance, a normal patient who gains a significant amount of weight may begin to snore, develop arousals during the night and begin to move into a disease state. With additional weight gain, this patient may develop increased airway resistance or sleep apnea. A patient who consumes alcohol on a given night can also move on the scale in a similar fashion; as muscle tone decreases, obstruction increases. Similarly, a patient with sleep apnea who loses weight may develop less severe airway resistance, simple snoring, or even achieve a normal state of breathing at night. Thus, the number generated on a polysomnogram must be viewed in the context of the patient’s overall disease and night-to-night variation of their sleep-disordered breathing.
Table 7.1 The continuum of sleep disordered breathing
Although there are numerous metrics to measure the severity of obstructive sleep apnea, disease severity is generally described in terms of the number of apneas plus hypopneas per hour of sleep, or via the Apnea Hypopnea Index (AHI) and O2 saturation as measured on an overnight sleep study, or polysomnogram. The polysomnogram represents a snapshot in time which may not reflect a patient’s level of disease over a long period of time, but it is still the best measure of disease severity available at present.
Lastly, a respiratory effort-related arousal (RERA) is an event that occurs when a patient develops an arousal on electroencephalogram in conjunction with increasing inspiratory effort during sleep. RERAs can be added to apneas and hypopneas to create the Respiratory Disturbance Index (RDI) which many use to guide treatment.2
3 EFFECTS OF SLEEP APNEA AND TREATMENT THRESHOLDS
The physiological manifestations are important and principally relate to cardiovascular consequences of OSA, though there are other physiological effects of disordered breathing during sleep, such as alterations in inflammatory biomarkers, which also occur. Cardiovascular consequences include associations with stroke, hypertension and myocardial infarction and are being studied rigorously in the Sleep Heart Health Study, which is longitudinally tracking a cohort of OSA patients with measures of OSA and medical outcomes.3
The behavioral effects of sleep disruption are commonly evident. These may manifest as tiredness in the morning or daytime, falling asleep in permissive situations such as watching TV or reading a book, an increased incidence of motor vehicle accidents, and losses of concentration and productivity. A simple patient self-report scale, the Epworth Sleepiness Scale, was designed to quantify this level of tiredness4 though there are also objective measures of alertness such as the psychomotor vigilance test.5 The behavioral effects of OSA can be variable among patients where a patient with snoring may have significant tiredness whereas a patient with an elevated AHI and greater nighttime obstruction may not display tiredness. This discrepancy appears to make behavioral measurement alone insufficient to fully characterize the disease or its treatment.
In light of the variability in the manifestation of OSA in patients and the gaps in our knowledge as to which patients will suffer cardiovascular consequences of this disease, significant controversy exists with respect to selection of patients for OSA treatment. In a review article on OSA, Ward Flemons writes, ‘In the majority of patients without coexisting conditions … the primary reason to test for and treat sleep apnea is the potential to improve the quality of life.’1 Studies vary in determining the magnitude of effects of mild to moderate OSA on hypertension and cardiovascular consequences. However, ongoing studies of large cohorts of patients such as the Sleep Heart Health Study are yielding important data that will provide guidelines for treatment in the future.6 With information on physiological consequences of OSA such as effects on inflammatory and other biomarkers as well as data from the Sleep Heart Health Study emerging, our threshold and circumstances for intervention will certainly evolve.
Nevertheless, physicians are faced today with patients needing treatment and decisions must be made. The best available evidence is synthesized to assist with these decisions, and treatment thresholds developed. In an attempt to help delineate a treatment threshold, one oft-quoted study determined that patients with an Apnea Index (AI) of >20 were at increased cardiovascular risk.7 Many use the cut-off of an AHI of 20 as the threshold for treatment (note the original cut-off of AI >20 has been subsequently adopted as AHI >20). While virtually all admit that patients with an AHI of >30 should be treated regardless of co-morbidity or behavioral effects, rigorous evidence for treatment of patients with an AHI of <30 is lacking.2 However, patients with AHI <30 with significant co-morbidity or behavioral effects (e.g. tiredness, loss of concentration) are also considered candidates for treatment of OSA.
It is the opinion of the author that all patients with an AHI >30 should be treated for OSA and symptomatic patients with an AHI <30 should be treated. Patients with an AHI <30 may have other factors that bring them to treatment including medical co-morbidities or other parameters on the polysomnogram that mandate treatment (e.g. low oxygen saturation, arrhythmias).
4 EVALUATION FOR OSA
4.1 HISTORY
A history of snoring, gasping, or witnessed apneas may be characteristic of sleep-disordered breathing, and the duration of the problem should be noted. Patients may be tired in the morning or daytime and may fall asleep in permissive situations. Patients should be generally questioned about their sleep habits and relevant history. Various questionnaires are available to evaluate the patient with sleep-disordered breathing. The Epworth Sleepiness Scale is particularly easy to administer, it is quantitative, and gives insight into the degree of sleepiness that the patient is experiencing.4
< div class='tao-gold-member'>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


