Oral and maxillofacial surgeons play an important role in the primary surgical treatment of patients with obstructive sleep apnea syndrome (OSAS). These surgical specialists have considerable experience and expertise in the diagnosis and treatment of dentofacial deformities. Application of the same surgical principles and procedures in patients who have anatomic abnormalities that contribute to narrowing or obstruction of the pharyngeal airway during sleep will produce predictable and successful outcomes.
Incidence
Patients with obstructive sleep apnea experience repeated complete and partial blockages of the upper airway during sleep. Such blockages are referred to as apneas and hypopneas. An obstructive apnea is defined as the absence of breathing for 10 seconds or more, despite an effort to breathe. The clinical definition of hypopnea is a 30% reduction in thoraco-abdominal movement or airflow as compared with baseline lasting at least 10 seconds, with 4% or more oxygen desaturation.
The severity of obstructive sleep apnea (OSA) is measured using the apnea-hypopnea index (AHI), which assesses the total number of apneas and hypopneas per hour of sleep. Obstructive sleep apnea syndrome is defined as an AHI ≥ 5 along with excessive daytime sleepiness reported by the patient. Guidelines produced by the Institute for Clinical Systems Improvement (ICSI) state that a diagnosis of mild OSA requires an AHI score of 5 to 15; AHI scores of 16 to 30 indicate moderate OSA; and those greater than 30 indicate severe OSA.
OSAS is a common disorder with an incidence of 4% and 2% among middle-aged (30 to 60 years) men and women, respectively. Estimates for elderly men range from 28% to 67% and from 20% to 54% for elderly women. The prevalence of sleep-disordered breathing, which is defined as an AHI of at least 5, is 24% of adult men and 9% of adult women.
There is a disparity between the estimated prevalence of obstructive sleep apnea and daytime sleepiness, and the number of patients whose conditions are recognized and treated. Young and colleagues reported that at least 80% of the cases of moderate and severe OSA in adults aged 30 to 60 years in the general population go undiagnosed. Kapur et al. have reported that the true prevalence of OSA and associated daytime sleepiness may be three times higher than the number of patients diagnosed with this sleep disorder. The significant health and social consequences of OSAS and the recent finding that it is a relatively common condition that frequently remains undiagnosed make it an important public health issue.
Risk/Causative Factors
The fundamental problem associated with obstructive sleep apnea is the inability to maintain upper airway (UAW) patency when sleeping, which can result in reduction (hypopnea) or cessation (apnea) of breathing. The obstruction can occur at multiple levels in the airway, and it is critical to diagnose the site of occlusion. Patency of the UAW is maintained mostly by the activation of pharyngeal muscles in the underlying soft tissue structures, which depends on the facial skeleton and muscle tone.
Factors associated with the patient’s craniofacial anatomy can alter the mechanical properties of the upper airway and increase its propensity to collapse during sleep. Static cephalometric analysis using radiography, computerized tomography, and magnetic resonance imaging (MRI) has revealed a number of skeletal and soft tissue structural differences during wakefulness between individuals with and without obstructive sleep apnea. Features such as retropositioning of the maxilla and mandible, enlarged tongue or soft palate, and decreased posterior airway space can narrow upper airway dimensions and promote the occurrence of apnea and hypopneas during sleep. Even in the absence of clinically obvious craniofacial abnormalities, subtle differences in maxillary and mandibular size or position can increase the vulnerability for obstructive sleep apnea. A meta-analysis of studies investigating the craniofacial risk factors show that mandibular body length is the craniofacial measure with the strongest association with increased risk for OSA. In the Wisconsin Cohort of Sleep Disordered Breathing Study, two thirds or more of the variability of the apnea-hypopnea index was explained by facial structure and obesity. In nonobese subjects, the major contributor was facial structure.
The size and the position of the tongue are important considerations in OSA. In the supine position, the tongue projects posteriorly and is counteracted by the tone of the genioglossal muscle. MRI volumetric studies have identified tongue size as a major predictor of OSA. With advancing age, sleep-related difficulties, including excessive daytime sleepiness secondary to obstructive sleep apnea, become increasingly common. Data from the community-based Sleep Heart Health Study have shown that OSA prevalence increases steadily with age and reaches a plateau after the age of 60 years. Mechanisms proposed for the age-related increase in prevalence include increased deposition of fat in the parapharyngeal area, lengthening of the soft palate, and changes in body structure surrounding the pharynx.
Epidemiologic studies from around the world have consistently identified body weight as the strongest risk factor for obstructive sleep apnea. In the Wisconsin Sleep Cohort Study, a one standard deviation difference in body mass index (BMI) was associated with a fourfold increase in disease prevalence. It has long been recognized that men have greater vulnerability than women toward developing obstructive sleep apnea. Clinic-based studies have shown that, in patients referred for clinical evaluation, the ratio of men to women is in the range from 5 to 8 to 1. The male predisposition for the sleep disorder has been attributed to sex differences in anatomic and functional properties of the upper airway and in the ventilatory response to arousals from sleep. Hormonal influences are also likely to have an important role in the pathogenesis of obstructive sleep apnea, as disease prevalence is higher in post- versus premenopausal women.
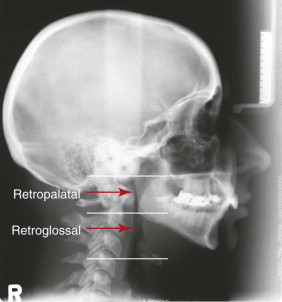
Studies to localize the site of functional obstruction in the upper airway have shown that there is rarely a single anatomic site of occlusion; more commonly there are multiple sites of UAW obstruction during episodes of hypopnea and apnea. The two major sites of obstruction are in the retropalatal and retroglossal regions ( Fig. 112-1 ). Positional factors that may exacerbate upper airway resistance during sleep include mouth opening (which increases collapsibility or decreases efficacy of dilator muscles) and a supine posture (which facilitates the gravitational forces that posteriorly displace the tongue and soft palate).
Upper airway competence involves complex interactions between anatomy and physiology. For most, OSA is an abnormality of a structurally small and abnormally collapsible upper airway interacting with normal physiologic mechanisms.
Risk/Causative Factors
The fundamental problem associated with obstructive sleep apnea is the inability to maintain upper airway (UAW) patency when sleeping, which can result in reduction (hypopnea) or cessation (apnea) of breathing. The obstruction can occur at multiple levels in the airway, and it is critical to diagnose the site of occlusion. Patency of the UAW is maintained mostly by the activation of pharyngeal muscles in the underlying soft tissue structures, which depends on the facial skeleton and muscle tone.
Factors associated with the patient’s craniofacial anatomy can alter the mechanical properties of the upper airway and increase its propensity to collapse during sleep. Static cephalometric analysis using radiography, computerized tomography, and magnetic resonance imaging (MRI) has revealed a number of skeletal and soft tissue structural differences during wakefulness between individuals with and without obstructive sleep apnea. Features such as retropositioning of the maxilla and mandible, enlarged tongue or soft palate, and decreased posterior airway space can narrow upper airway dimensions and promote the occurrence of apnea and hypopneas during sleep. Even in the absence of clinically obvious craniofacial abnormalities, subtle differences in maxillary and mandibular size or position can increase the vulnerability for obstructive sleep apnea. A meta-analysis of studies investigating the craniofacial risk factors show that mandibular body length is the craniofacial measure with the strongest association with increased risk for OSA. In the Wisconsin Cohort of Sleep Disordered Breathing Study, two thirds or more of the variability of the apnea-hypopnea index was explained by facial structure and obesity. In nonobese subjects, the major contributor was facial structure.
The size and the position of the tongue are important considerations in OSA. In the supine position, the tongue projects posteriorly and is counteracted by the tone of the genioglossal muscle. MRI volumetric studies have identified tongue size as a major predictor of OSA. With advancing age, sleep-related difficulties, including excessive daytime sleepiness secondary to obstructive sleep apnea, become increasingly common. Data from the community-based Sleep Heart Health Study have shown that OSA prevalence increases steadily with age and reaches a plateau after the age of 60 years. Mechanisms proposed for the age-related increase in prevalence include increased deposition of fat in the parapharyngeal area, lengthening of the soft palate, and changes in body structure surrounding the pharynx.
Epidemiologic studies from around the world have consistently identified body weight as the strongest risk factor for obstructive sleep apnea. In the Wisconsin Sleep Cohort Study, a one standard deviation difference in body mass index (BMI) was associated with a fourfold increase in disease prevalence. It has long been recognized that men have greater vulnerability than women toward developing obstructive sleep apnea. Clinic-based studies have shown that, in patients referred for clinical evaluation, the ratio of men to women is in the range from 5 to 8 to 1. The male predisposition for the sleep disorder has been attributed to sex differences in anatomic and functional properties of the upper airway and in the ventilatory response to arousals from sleep. Hormonal influences are also likely to have an important role in the pathogenesis of obstructive sleep apnea, as disease prevalence is higher in post- versus premenopausal women.
Studies to localize the site of functional obstruction in the upper airway have shown that there is rarely a single anatomic site of occlusion; more commonly there are multiple sites of UAW obstruction during episodes of hypopnea and apnea. The two major sites of obstruction are in the retropalatal and retroglossal regions ( Fig. 112-1 ). Positional factors that may exacerbate upper airway resistance during sleep include mouth opening (which increases collapsibility or decreases efficacy of dilator muscles) and a supine posture (which facilitates the gravitational forces that posteriorly displace the tongue and soft palate).
Upper airway competence involves complex interactions between anatomy and physiology. For most, OSA is an abnormality of a structurally small and abnormally collapsible upper airway interacting with normal physiologic mechanisms.
Harmful Effects of OSAS
The physiologic changes that accompany each obstructive event in patients with OSAS include hypoxemia, hypercapnia, fluctuations in intrathoracic pressure caused by increased respiratory effort, arousal from sleep, and increased sympathetic tone. On a repetitive basis, these physiologic events are believed to result in long-term comorbidities such as hypertension, cardiac-related death while sleeping, coronary artery disease, stroke, depression, diabetes mellitus, and glaucoma. Results demonstrating that effective treatment of OSAS can abort and even reverse the atherogenic process suggest that it should be diagnosed and treated as early as possible to prevent cardiovascular sequelae. Deficits affecting attention, concentration, vigilance, manual dexterity, visual motor skills, memory, verbal fluency, and executive function have been reportedly associated with OSAS. Excessive daytime sleepiness can undoubtedly influence one’s driving performance. Prospectively gathered motor vehicle accident rates in OSAS patients have been found to be 1.3 to 7 times higher than those in the general population. There is evidence indicating an increased risk of occupational accidents for those with OSAS. Patients suffering from excessive daytime sleepiness (EDS) will often complain of a lack of daytime energy, decreased feeling of well-being, and decreased libido and sexual performance.
OSAS is a life-threatening disease that predisposes the patient to physical harm, significant social discord, and poor quality of life.
Evaluation of Obstructive Sleep Apnea
The diagnosis of obstructive sleep apnea is based on findings acquired by a clinical history, physical examination, imaging studies, and polysomnography.
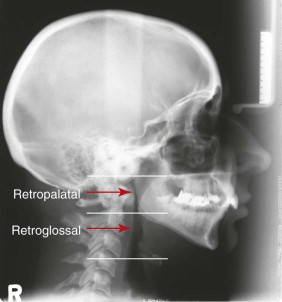
Clinical symptoms of OSA include very loud snoring, choking at night, witnessed apneas, frequent arousals, excessive daytime sleepiness, poor concentration, poor memory, mood changes, irritability, headaches upon awakening, absence of dreams, and symptoms of depression. Although many of these symptoms are very sensitive, they are not always specific to obstructive sleep apnea. The best predictor of obstructive sleep apnea is the triad of symptoms that includes loud snoring, apnea witnessed by a bed partner, and excessive daytime sleepiness. In the primary care setting, the Epworth Sleepiness Scale (ESS) is the most frequently used questionnaire-based measure of excess daytime somnolence; it is a subjective, eight-item, self-reported questionnaire that is simple to use and takes less than 2 minutes to complete ( Fig. 112-2 ). Not only can the ESS confirm pathologic sleepiness, but it can also be used to validate posttreatment improvement in patients with OSA. An ESS score of 10 or greater is considered abnormal.
Clinical examination has been shown to be useful in the prediction of OSA and its severity. During the clinical examination, the patient’s height, weight, BMI, and blood pressure are recorded. The patient’s facial profile is noted, with special attention paid to the chin-neck angle and nasolabial angle. Examination of the oral cavity includes documentation of the presence/size of tonsils, soft palate tissue redundancy, uvula length and thickness, and size and presence of indentations of the tongue. Although many authors recommend nasopharyngoscopy in conjunction with the Müller maneuver to identify the site of obstruction, several recent articles suggest that, because multiple factors are involved in the dynamics of OSA that are not fully understood, the likelihood of surgical success does not correlate with the clinical finding on Müller’s maneuver. A recent clinical review of airway evaluation in obstructive sleep apnea patients by Stuck found that the reliability of the Müller maneuver remains highly questionable, as the evaluation used by this technique seems subjective and hard to reproduce. He concluded that the Müller maneuver does not facilitate patient selection for the varying surgical interventions used in OSA patients.
Lateral x-ray cephalometry is one of the standard diagnostic tools used for patients with sleep-disordered breathing (SDB), especially with regard to the evaluation of the skeletal craniofacial morphology. It is regarded as a mandatory assessment tool and its value is not questioned. Although beneficial effects of CT scanning on treatment selection and thereby treatment outcome have been repeatedly postulated, the literature does not demonstrate its clinical use to date. Only a small number of authors have attempted to establish distinct protocols for the use of MRI of the upper airway in SDB. Hardly any consensual standards exist for this indication. MRI has not become a standard procedure, neither in the diagnostic workup for patients with SDB nor in management of the disease in terms of surgical or nonsurgical treatment.
Overnight polysomnography conducted in a sleep laboratory identifies sleep apnea caused by obstructive or central events and remains the gold standard for the diagnosis of sleep apnea. Central sleep apnea (CSA) is characterized by a lack of drive to breathe during sleep, resulting in insufficient or absent ventilation and compromised gas exchange. In contrast to OSA, in which ongoing respiratory efforts are observed, CSA is defined by a lack of respiratory effort during cessation of airflow. CSA, like OSA, is associated with important complications including frequent nighttime wakenings, excessive daytime sleepiness, and an increased risk of adverse cardiovascular outcomes. CSA is relatively uncommon and may affect less than 5% of patients referred to a sleep clinic. Usually, CSA is considered to be the primary diagnosis when greater than 50% of apneas are scored as central in origin (i.e., greater than 10-second cessation of breathing in the absence of respiratory effort). Typically, these patients are thinner and snore less than patients with OSA, although male predominance is likely a common trait. The underlying mechanisms for this disorder are not fully understood. Given the range of pathophysiologic factors contributing to the varied forms of CSA, treatment approaches also vary considerably and do not include surgery. Noninvasive ventilation such as continuous positive airway pressure (CPAP) has been shown to be effective in some patients with CSA. The mechanism for improvement in these patients is not clear but may relate to the prevention of inhibitory reflex mechanisms that arise during airway closure and potentially to CPAP-induced increases in lung volume and oxygen stores.
Overnight polysomnography involves the use of electroencephalogram (EEG), electro-oculogram (EOG), electromyogram (EMG), electrocardiogram (ECG), microphone measurement of snoring, pulse oxymetry, respiratory inductance plethysmography, airflow measurement, and recording of body position by infrared imaging. The stage of sleep is determined by a combination of EEG, EOG, and EMG. Episodes of apnea and hypopnea are determined from a reduction in airflow in combination with oxygen desaturation.
Treatment Options
To assist the patient in making an informed decision regarding treatment choices, the oral and maxillofacial surgeon must be familiar with the risks and benefits of common treatment options. OSAS can be managed nonsurgically or surgically. The recommended treatment should target potential contributing factors identified by history, physical examination, and UAW imaging. The severity of the patient’s condition should also be considered when treatment options are reviewed.
In 2009, a literature search in PubMed under the heading “obstructive sleep apnea and treatment” yielded approximately 7,200 articles. The same search in 2005 resulted in approximately 3,400 articles. This demonstrates that the interest in this condition is increasing in an exponential fashion, but it also suggests that there is not a clear-cut approach to the management of these patients. A breakdown of these articles reveals approximately 13 nonsurgical options. Surgical options total approximately 19 procedures and deal with surgery in eight regions of the head and neck, which include the pharynx, hyoid, tonsil, tongue, palate, turbinates, nasal septum, and nasal valve. To recommend the best treatment option, the surgeon needs to understand the underlying pathology and recommend treatment based on the correction of an anatomic abnormality.
Nonsurgical management options included behavioral interventions, CPAP devices, and oral appliances. Because obesity is a risk factor for OSAS, a reduction in body weight can reduce the number of obstructive apneas. In the Wisconsin Sleep Cohort Study, a 10% weight gain predicted a 32% increase in AHI, whereas a 10% weight loss predicted a 26% decrease in AHI. It should be noted, however, that the recurrence of OSAS has been reported after surgically induced weight loss, even though the weight was not regained. Although patients may be advised to lose weight, they will have difficulty doing so, particularly in the more severe cases, because excess daytime somnolence and fatigue may discourage the patient from exercising. It is also important to note that approximately 30% of people with OSAS are not obese, and these patients most often have an underlying craniofacial deformity. Mild OSA may be improved with avoidance of alcohol and sedatives and by sleeping in a more upright or lateral position. Patients with OSA who sleep on their backs (the supine position) often have prolonged respiratory events, greater oxygen desaturation, longer arousals from sleep, and louder snoring than those who sleep laterally. When sleep posture is altered to a more lateral position through the use of pillows or body belts, changes occur in the patient’s lung volume, neurovascular activity, and airway size, so as to support the airway with reduced collapsibility. However, long-term randomized trials are lacking for this intervention, and a number of small studies have reported that AHI scores are only partially reduced by lateral sleep posture. Nasal dilators do not appear to alleviate the symptoms or decrease the severity of OSA.
The most successful nonsurgical treatment of OSAS is continuous positive airway pressure (CPAP) applied by a nasal or full face mask. CPAP therapy maintains upper airway patency during sleep by acting as a pneumatic splint and opening the airways, thus abolishing apnea, hypopnea, and snoring, and improving sleep quality. The pressure required to achieve this is titrated at a sleep laboratory during the polysomnography. CPAP is a sound, evidence-based treatment option that has been shown to decrease daytime sleepiness and improve mood and quality of life. Unfortunately, because of physical discomfort associated with wearing the unit, drying of the nasal and oral mucous membranes, dislodgement during sleep, noise, and the inconvenience of transporting the unit, the long-term compliance with CPAP use on a nightly basis can be as low as 25%. It is prudent to advise all patients to undergo a trial of CPAP therapy before considering irreversible treatment options such as surgery.
The American Academy of Sleep Medicine (AASM) currently recommends oral appliances for the treatment of mild to moderate OSA in patients who prefer them to CPAP therapy or who do not respond to the CPAP therapy. Treatment of OSA with dental devices is generally viewed as being less efficacious than treatment with CPAP. Overall, oral appliances are felt to be successful in cases of mild OSAS but relatively less effective in more severe cases. One of the factors limiting wider application of oral appliance treatment is the inability to identify those patients who will have a successful outcome before investing the time and resources necessary to implement this treatment. The significant potential negative long-term effects of oral appliances are temporomandibular joint pain and detrimental changes to the patient’s occlusion. An important concern is that a dental appliance may eliminate or decrease snoring in certain patients but their sleep apnea persists, and the patient is not aware of the potential need to seek further treatment.
Surgical treatment options include tracheostomy, uvulopalatopharyngoplasty (UPPP), isolated hard or soft tissue surgery, and maxillo-mandibular advancement (MMA). Tracheostomy was the first successful surgical treatment for OSAS and has a virtually 100% success rate because it bypasses the level of obstruction in the UAW completely. Medical and obvious social problems associated with tracheostomy stimulated the search for alternate treatment.
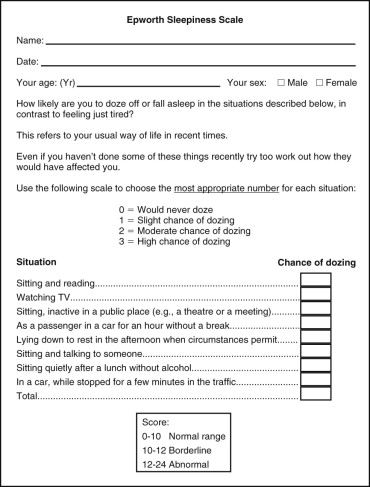
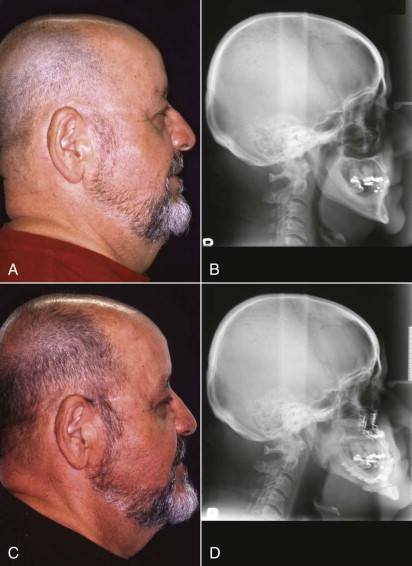
A common surgical treatment is the UPPP, originally described in 1981 by Fujita and, at that time, recommended as the sole treatment for OSAS. It continues to be popular despite reviews that report improvement in less than 50% of patients and complete control of OSAS in less than 25% of patients. The reason for the very low success rate of this procedure is that it addresses only one site of a multisite problem. Soft tissue changes are unpredictable—in fact, the changes can be detrimental because they cause narrowing of the pharyngeal airway. Clinical examination of the UPPP patient reveals that the soft palate appears shorter and has a firm scar band on the inferior surface. More important, however, is that lateral cephalometric radiographs reveal that although the soft palate is much shorter, it is also much thicker, and this can result in a narrower retropalatal pharyngeal airway as seen on cephalometric radiographs ( Fig. 112-3 ). This could explain why the AHI increases in approximately 30% of patients after UPPP .
The presence of tonsil or adenoid hypertrophy physically reduces the dimensions of the pharyngeal airway, and, when present, surgery to remove this excess tissue should be considered as first-stage treatment. If septal deviation or exostosis and turbinate enlargement are present, these abnormalities can be addressed at the same time as the performance of a maxillary advancement procedure. Treatments isolated to these areas in the nasal cavity have not proven to significantly benefit the patient, and ultimately the patient requires additional surgical procedures including orthognathic surgery.
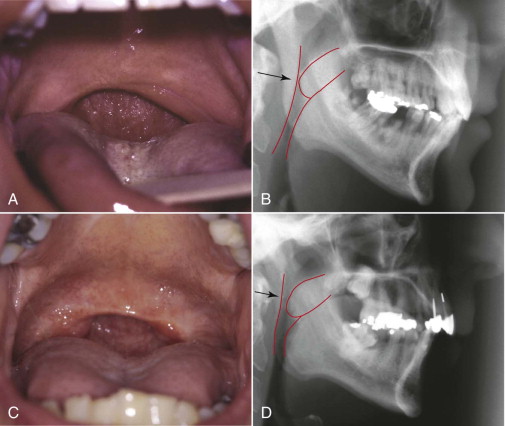
Maxillo-mandibular advancement surgery (MMA) has been considered in the treatment of sleep apnea since the late 1970s and is considered the most successful surgical alternative to tracheostomy for the treatment of OSA. Of significance, is the realization that MMA is the one procedure that can address anatomic abnormalities in all of the anatomic regions of the head and neck identified as the surgical objective in each of the 19 surgical procedures commonly discussed in the literature. The major biologic basis of this treatment relates to how MMA improves the dimensions and stability of the pharyngeal airway. When a mandibular advancement is performed, the anterior belly of the digastric, the mylohyoid, the genioglossus, and the geniohyoid muscles help pull the tongue forward and upward away from the pharynx. Performing a maxillary advancement pulls the soft tissue of the palate forward and upward and also pulls the palatoglossal muscles, which increases tongue support. Both movements have a positive influence on the pharyngeal airway ( Fig. 112-4 ). Fiberoptic nasopharyngoscopy after MMA reveals a decrease in airway collapsibility secondary to improvement in lateral pharyngeal wall stability. Analysis of the morphologic changes of the pharyngeal airway in obstructive sleep apnea patients by helical computed tomography scanning following maxillo-mandibular advancement surgery revealed a significant enlargement of lateral and anteroposterior (AP) airway dimensions for all patients, at all levels.
Treatment Planning
A criticism of most surgical treatment protocols for MMA surgery in patients with OSAS is the rather “abstract” selection process for surgical candidates. This criticism highlights the need for the use of a cephalometric radiograph and the appropriate cephalometric analysis that will identify bony and soft tissue abnormalities related to the soft palate, pharyngeal airway, and maxillo-mandibular complex influencing the multiple sites of obstruction. If the radiographic and clinical examinations of the soft tissues of the pharynx reveal a narrow airway in conjunction with retrognathia of the maxilla and mandible, then the patient should be a candidate for MMA surgery. Because an underlying skeletal abnormality is sometimes hard to detect clinically, it is reasonable for an oral and maxillofacial surgeon to assess these patients ( Fig. 112-5 ).
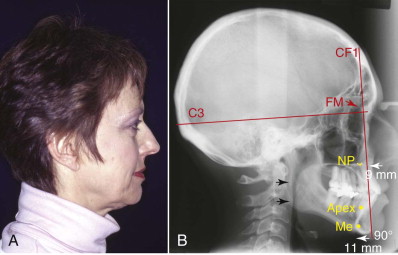
The surgeon’s goal is to optimize the advancement of the deficient structures while maintaining normal facial balance for each individual patient. To do this, the surgeon should use a cephalometric analysis that clearly demonstrates all the maxillofacial abnormalities, as well as provide a visual treatment objective. An example of such an analysis is the Architectural and Structural Craniofacial Analysis of Delaire ( Fig. 112-6
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


