Anterior open bite is one of the most challenging malocclusions for orthodontic treatment. The high incidence of relapse is a major concern. Therefore, accurate initial examination, diagnosis, treatment plan, and consideration of habitual risk factors are crucial for a successful outcome without unwanted sequelae. Excellent patient compliance for retainer wear is also a critical factor. This case report shows the 3-year stability of a nonsurgical and nonextraction orthodontic treatment of a 5-mm anterior open-bite malocclusion in a 12-year-old girl with extrusion mechanics and habit modification. After 2 years of orthodontic treatment, excellent outcomes were achieved. With an appropriate retention protocol, the long-term stability of the treatment was favorable.
Anterior open bite is a condition characterized by a lack of vertical overlap between the incisal edges of the maxillary and mandibular teeth when the remaining teeth are in occlusion. Anterior open bite has a multifactorial etiology including skeletal, dental, respiratory, neurologic, and habitual components. Thumb sucking, tongue thrust, and increased vertical skeletal relationships are significant risk factors associated with anterior open bite, and patients often have concomitant transverse discrepancies. Various treatments with nonsurgical or surgical approaches including habit modification have been reported in the literature for open bite. The long-term stability after surgical and nonsurgical approaches is thought to be acceptable, but some reports showed the opposite. It is one of the most challenging malocclusions to treat because of the high frequency of relapse. Open bites relapse in 25% to 38% of orthodontically treated patients. In this case report, we present the 3-year follow-up and the results of nonsurgical treatment of an adolescent patient with an anterior open bite and a constricted maxillary arch who was treated with rapid palatal expansion, habit modification, and extrusion mechanics.
Diagnosis and etiology
A Hispanic girl, age 12 years 9 months, had a convex profile, a Class I malocclusion, an anterior open bite, and a tongue-thrust habit. She was in a good general health and had no history of major systemic disease or accident or history of a thumb-sucking habit. Her chief complaint was an open bite with crooked mandibular teeth. The tongue-thrust habit was observed during swallowing and conversation.
Pretreatment facial photographs ( Fig 1 ) showed that the patient had a convex soft tissue profile with an obtuse nasolabial angle. From the frontal view, her face was slightly asymmetric, and the chin was deviated slightly toward the left. Upon smiling, she had inadequate gingival exposure. Intraoral and dental cast examinations ( Figs 1 and 2 ) demonstrated a Class II molar tendency bilaterally. A 5-mm anterior open bite was observed with 2 levels of occlusal planes, anterior and posterior. The only teeth in contact were the left first molars and the right second premolars and first molars. A significant tongue-thrust habit was noticed at rest and also while swallowing. The maxillary arch was relatively narrow compared with the mandibular arch. Five millimeters of anterior crowding in the maxillary arch and 4 mm of anterior crowding in the mandibular arch were observed. A 3-mm Bolton discrepancy with mandibular anterior tooth excess was measured. No mandibular deviation or clicking noises were detected during opening or closing of her jaws.

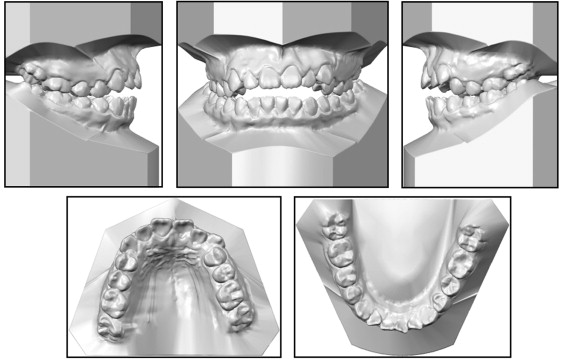
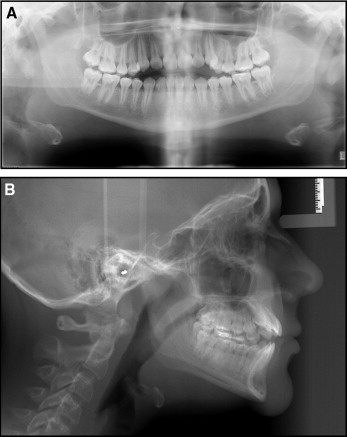
Panoramic and lateral cephalometric radiographs were taken before treatment ( Fig 3 ). The panoramic radiograph showed no caries, and all third molars were congenitally missing ( Fig 3 , A ). The cephalometric analysis ( Fig 3 , B ; Table ) demonstrated a Class I skeletal relationship (ANB, 2.2°; Wits appraisal, −2.2 mm) with a hyperdivergent growth pattern tendency (SN-MP, 38.7°). The angle between the maxillary incisors and the sella-nasion plane was 107.4°, the mandibular incisor to mandibular plane angle was 99°, and the interincisal angle was 114.8°. Based on the findings, the patient was diagnosed as skeletal Class I with a dental open bite. The etiology of the open-bite malocclusion appeared to be a combination of hereditary and habitual factors.
| Measurement | Norm | Initial | Final | Retention (3 years) |
|---|---|---|---|---|
| SNA (°) | 83.6 ± 6.4 | 75.3 | 76.9 | 76.9 |
| SNB (°) | 80.8 ± 6.0 | 73.2 | 74.0 | 74.0 |
| ANB (°) | 2.8 ± 3.8 | 2.2 | 2.9 | 2.9 |
| Wits appraisal (mm) | −1.0 ± 1.0 | −2.2 | −2.5 | −3.1 |
| SN to MP (°) | 26.6 ± 10.6 | 38.7 | 39.7 | 39.6 |
| U1 to SN (°) | 105.0 ± 10.6 | 107.4 | 102.1 | 101.6 |
| L1 to MP (°) | 4.3 ± 11.1 | 9.0 | 9.3 | 10.1 |
| Upper lip to E-line (mm) | −3.2 ± 2.0 | −6.4 | −7.1 | −6.9 |
| Lower lip to E-line (mm) | 3.0 ± 2.0 | −2.8 | −2.3 | −2.5 |
Treatment objectives
The following treatment objectives were established: (1) close the patient’s open bite and create ideal overject and overbite, (2) relieve the crowding, (3) correct the constricted maxilla, (4) eliminate the tongue thrust, (5) correct the midline deviation, (6) obtain a stable occlusal relationship, and (7) ultimately improve her dental esthetics by establishing an esthetic smile.
Treatment objectives
The following treatment objectives were established: (1) close the patient’s open bite and create ideal overject and overbite, (2) relieve the crowding, (3) correct the constricted maxilla, (4) eliminate the tongue thrust, (5) correct the midline deviation, (6) obtain a stable occlusal relationship, and (7) ultimately improve her dental esthetics by establishing an esthetic smile.
Treatment alternatives
The patient had a hyperdivergent growth pattern tendency, and dental extrusion mechanics might create a more severe open bite without control of the vertical dimension. Orthognathic surgery to close her open bite by a segmented 3-piece LeFort I osteotomy with a bone graft, combined with fixed orthodontic treatment, was discussed with the patient and her parents. Skeletal discrepancy correction, facial and dental esthetic change, and establishment of an ideal occlusion would all be possible with this surgical approach.
Fixed orthodontic treatment alone could extrude the anterior teeth and induce skeletal alveolar bone growth to correct the open-bite malocclusion and increase the anterior gingival display. For this patient, both nonextraction and extraction were possible: (1) nonextraction with maxillary expansion to correct the posterior crossbite and gain space to correct crowding and also use a tongue crib or spurs to modify the tongue-thrust behavior during the treatment followed by a set of retainers with a tongue reminder; or (2) extraction of 4 premolars to gain space for the correction of crowding and in consideration of the open-bite tendency for hyperdivergent growth.
The patient and her parents declined orthognathic surgery as well as orthodontic treatment with extractions. Because of this response, the plan included a nonextraction approach with rapid palatal expansion and a tongue appliance to correct the open-bite malocclusion.
Treatment progress
Before the treatment, the patient was referred to a pedodontist to verify that she had no caries and for a routine periodontal checkup. Bands were fitted on the maxillary first premolars and first molars, and an impression was taken for a Haas rapid palatal expander. The Haas expander with a 12-mm expansion screw was cemented in the maxillary arch, and the parents and the patient were instructed to turn the screw once each day until a buccal overjet was observed. Then the expander was stabilized for 4 months. A 3-mm diastema between the maxillary central incisors was observed at the end of expander activation ( Fig 4 ). Preadjusted 0.018 × 0.025-in slot edgewise brackets (3M Unitek, Monrovia, Calif) were bonded to each tooth, and a 0.016-in archwire and a 0.016 × 0.022-in superelastic nickel-titanium archwire (Dentsply GAC, Bohemia, NY) were used for the initial leveling. At the same time, a supplemental 0.016 × 0.022-in stainless steel archwire (Dentsply GAC) was fabricated as an extrusion arch using the Haas expander as anchorage and ligated to the nickel-titanium base wire at the midline during the leveling stage ( Fig 5 ). Two 0.030-in stainless steel wires were fabricated as tongue spurs and bonded on the mandibular central incisors with composite resin to modify the patient’s tongue-thrust habit ( Fig 6 ). After removal of the Haas expander, a transpalatal arch was cemented to maintain the transverse dimension of her maxilla ( Fig 6 ). Class II triangle elastics (1/4 in, 4.5 oz) from the maxillary canines to the mandibular canines and first molars, and box-vertical elastics (1/4 in, 4.5 oz) from the maxillary lateral incisors to the mandibular lateral incisors were applied during the entire orthodontic treatment. During the finishing stage, final detailing of the occlusion was accomplished with 0.017 × 0.025-in titanium-molybdenum archwires (Dentsply GAC) in conjunction with vertical elastics with Class II vectors (1/4 in, 6 oz). While the orthodontic treatment was in progress, the patient learned new tongue positions at rest and during swallowing. Her compliance was excellent throughout the treatment. One and a half millimeters of interproximal reduction was performed on the mandibular anterior teeth to eliminate the Bolton discrepancy.





