Introduction
In some skeletal Class III adult patients with nasomaxillary hypoplasia, the LeFort I osteotomy provides insufficient correction. This case report describes a 20-year-old woman with a combination of nasomaxillary hypoplasia and a protrusive mandible with a congenitally missing mandibular second premolar.
Methods
We performed a LeFort II osteotomy for maxillary advancement. Autotransplantation of a tooth was also performed; the donor tooth was used to replace the missing permanent tooth. To increase the chance of success, we applied light continuous force with an improved superelastic nickel-titanium alloy wire technique before extraction and after transplantation.
Results
The patient’s profile and malocclusion were corrected, and the autotransplanted tooth functioned well. The postero-occlusal relationships were improved, and ideal overbite and overjet relationships were achieved.
Conclusions
The methods used in this case represent a remarkable treatment.
Highlights
- •
The LeFort II osteotomy is the efficient method for improving nasomaxillary hypoplasia.
- •
A lower eyelid subciliary incision created a cosmetically acceptable result.
- •
Tooth autotransplantation combined with the improved superelastic wire technique is an effective treatment.
Comparative studies have shown the prevalence of Class III malocclusion to be related to race and ethnicity; the prevalences of Class III malocclusion have been reported as 13% for Japanese, 14.5% for Chinese, 19% for Koreans, and 3% for white people. The complications occurring in Class III patients can be classified as skeletal or dental; they include protrusive mandible, retrusive maxilla, and combinations of these. Therefore, the appropriate treatment for any patient should be carefully planned according to the specific type of malocclusion.
Wassmund was the first to perform a LeFort I osteotomy for dentofacial deformity correction, and Axhausen was the first to advance the maxilla by this method. During the 1960s, American surgeons began to adopt and modify maxillary surgical techniques that had been developed in Europe. Bell and Epker and Wolford reported encouraging results in dentofacial deformity correction using the LeFort I down-fracture technique, and this technique was widely adopted for maxillary osteotomies performed to correct dentofacial deformities.
However, in nasomaxillary hypoplasia patients, the standard LeFort I osteotomy may be insufficient to correct the total extent of the maxillary problem. Therefore, in some patients, the LeFort II osteotomy is the most efficient method for improving nasomaxillary hypoplasia. This technique was described by Henderson and Jackson in a landmark article published in 1973.
The patient in this case report had a combination of nasomaxillary hypoplasia and protrusive mandible with a congenitally missing mandibular second premolar. We demonstrate a successful result after performing a LeFort II osteotomy for maxillary advancement and tooth autotransplantation using the improved superelastic nickel-titanium (NiTi) alloy wire technique.
Diagnosis and etiology
The patient, a 20-year-old woman, had an anterior crossbite and a persistent mandibular left deciduous molar that was still present because the permanent second premolar was congenitally missing. Her chief complaint concerned her profile, which was characterized by a concave nasomaxillary area and a protrusive mandible. Other family members had no history of malocclusion. The pretreatment facial photographs showed a concave profile and upper lips that were retrusive relative to the E-line (upper lip, −5.0 mm; Fig 1 ). The maxillary midline was deviated by 1.0 mm to the right, and the mandibular midline was deviated 2.0 mm to the left relative to the facial midline. A chin deviation of 3.0 mm to the left of the midline was also evident. The patient had a Class III molar relationship on both sides ( Fig 2 ). She had a 4.0-mm overbite and a −3.0-mm overjet.

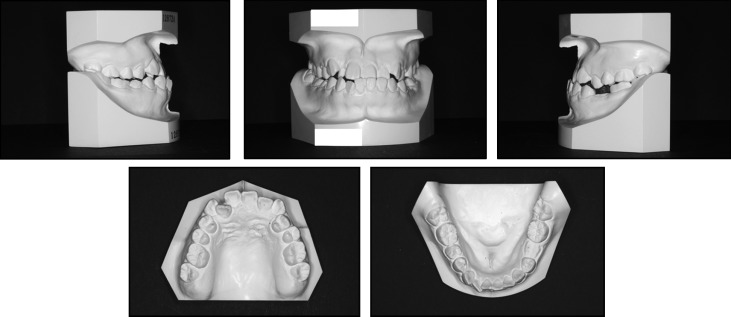
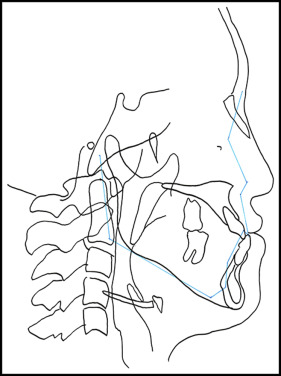
Lateral and anteroposterior cephalometric radiographs and a panoramic radiograph were taken before treatment ( Fig 3 ). The cephalometric analysis ( Table ) and the tracing ( Fig 4 ) demonstrated a Class III skeletal relationship (ANB, −3.7°) mainly because of the retrusive maxilla and the protrusive mandible. The SNA angle was 82.4°, and the SNB angle was large (86.8°). Nasion and orbitale were retruded compared with the Japanese average ( Fig 4 ). The midface was concave, and the wing of the patient’s nose was hidden by the cheek. The angle between the maxillary incisors and the SN plane was 120°, the angle between the mandibular incisors and the mandibular plane was 83.1°, and the interincisal angle was 122.4°. The apnea hypopnea index was 1.5 (within the normal range). The patient had a large tongue and a tongue-thrusting habit. Based on these findings, she was diagnosed as skeletal Class III with midface hypoplasia and a congenitally missing mandibular left second premolar.

| Variable (°) | Japanese norm | Pretreatment | Posttreatment | Retention |
|---|---|---|---|---|
| SNA | 82.3 ± 3.5 | 82.5 | 84.0 | 84.0 |
| SNB | 78.9 ± 3.5 | 86.3 | 84.5 | 84.5 |
| ANB | 3.4 ± 1.8 | −3.7 | −0.5 | −0.5 |
| FMA | 28.8 ± 5.2 | 25.6 | 28.2 | 28.0 |
| U1 to SN | 104.5 ± 5.2 | 120.0 | 114.9 | 115.1 |
| IMPA | 96.3 ± 5.5 | 83.2 | 81.8 | 80.3 |
| Interincisal angle | 124.1 ± 7.6 | 122.4 | 125.6 | 127.2 |
Treatment objectives
The treatment objectives for this patient were to (1) correct the midfacial hypoplasia and concave nasomaxillary appearance, which were her chief complaints; (2) correct the anterior crossbite; (3) establish full-cusp Class II molar relationships; (4) substitute a donor tooth for the missing mandibular left second premolar; (5) correct the midline shift; and (6) create an ideal occlusion with appropriate overbite and overjet.
Treatment objectives
The treatment objectives for this patient were to (1) correct the midfacial hypoplasia and concave nasomaxillary appearance, which were her chief complaints; (2) correct the anterior crossbite; (3) establish full-cusp Class II molar relationships; (4) substitute a donor tooth for the missing mandibular left second premolar; (5) correct the midline shift; and (6) create an ideal occlusion with appropriate overbite and overjet.
Treatment alternatives
The patient had midface hypoplasia, mandibular protrusion, and lateral deviation. Her chief complaints were a concave nasomaxillary area and a protrusive mandible. LeFort I or high LeFort I osteotomy with maxillary advancement and mandibular setback sagittal split ramus osteotomy (SSRO) are generally used to correct maxillary retrusion and mandibular protrusion. With nasomaxillary hypoplasia, however, the LeFort I osteotomy may be insufficient to correct the total extent of the maxillary problem. There are several treatment alternatives for maxillary advancement: LeFort II osteotomy and bone grafts, LeFort II osteotomy and LeFort I osteotomy and rigid external distractor system (simultaneously), and LeFort II osteotomy and rigid external distractor system.
Previous studies have suggested that if the maxilla is advanced more than 5 mm (the desired amount), iliac bone grafts should be performed with the rigid external distractor system to improve treatment stability. However, the patient refused to have iliac bone grafts because of the scars after surgery and also refused the rigid external distractor system device, which she found esthetically unpleasant and frightening. Therefore, a 2-step approach was planned. First, we would perform a LeFort II osteotomy followed by reassessment. Second, if further treatment were to be indicated, a LeFort I osteotomy and SSRO would be performed. In this case, there were large discrepancies in both the maxilla and the mandible. Maxillary molar distalization was not an option because there was not enough space posteriorly. Moreover, we did not plan for dental expansion because the basal arch width was narrow. The angle of inclination of the maxillary incisors was determined according to the plan from the setup model. Another reason behind our planning for the maxillary incisors was the limitation of the alveolar bone labial to the incisors. As seen in Figure 4 , there was limited thickness of alveolar bone in the anterior area.
This patient had anterior maxillary crowding and a large angle between the maxillary incisors and the SN plane (ie, labial inclination). Furthermore, she had a congenitally missing mandibular left second premolar and a residual deciduous molar. Extractions of the maxillary first premolars and third molars and the mandibular deciduous tooth were planned to create an appropriate occlusion, although other options such as a prosthesis were possible to replace the missing tooth. The maxillary left premolar was autotransplanted to replace the deciduous molar.
Treatment progress
The maxillary and mandibular third molars were extracted. Preadjusted edgewise appliances with an 0.018 × 0.025-in slot (Dentsply-Sankin, Tokyo, Japan) were bonded to the maxillary lateral segment canine and molars and to the mandibular teeth; 0.016 × 0.022-in improved superelastic NiTi alloy wires (L&H, Tomy International, Tokyo, Japan) were used for leveling. A transpalatal arch, J-hook headgear, and cervical headgear were used for anchorage.
Two weeks after extraction of the mandibular left deciduous molar, the maxillary left first premolar was extracted and autotransplanted in place of the mandibular left second premolar. After confirmation of autotransplantation, the maxillary right first premolar was extracted ( Fig 5 , A ). Then, the preadjusted edgewise appliances (with 0.018 × 0.025-in slots) were bonded to the maxillary anterior teeth, and a 0.016-in NiTi alloy wire (Sentalloy Blue, Tomy International) was used for leveling the maxillary anterior teeth ( Fig 5 , B ). The maxillary canines and anterior teeth were retracted by Prochain (Sankin, Tokyo, Japan) and NiTi alloy closed-coil springs (Tomy International).
After leveling and alignment, the LeFort II osteotomy was performed. The nasomaxillary complex was advanced by approximately 5.0 mm. During the LeFort II surgery, miniscrews were implanted on the maxillary alveolar bone between the lateral incisors and on the mandibular alveolar bone between the canines and first premolars ( Fig 5 , C ). The outlines for the skin incision and osteotomies are shown in Figure 6 . After the operation, heavy elastics (190 gf) and a maxillary protracting appliance (MPA) (adjustable dynamic protraction facemask; Ormco, Glendora, Calif) were used for surgical retention. The maxillary protracting appliance was protracted from miniscrews in the maxillary arch, and intermaxillary elastics were applied vertically between the maxillomandibular miniscrews.
Next, the intraoral component was pulled forward using approximately 150 g of elastic force applied unilaterally in a 20° to 30° downward direction from the occlusal plane. The patient wore the maxillary protracting appliance more than 13 hours per day for 18 months. The maxillary protracting appliance was used not only as the anchorage for maxillary advancement, but also for movement of the maxillary posterior teeth. Mesial movement was sequentially performed with the maxillary first premolar, second premolar, and first molar.
After LeFort II surgery, the patient refused to undergo a LeFort I osteotomy and SSRO. Elastics were used to correct the shifted midline. Elastics were prescribed for use between the maxillary left canine and the mandibular left first premolar, the maxillary right lateral incisor and the mandibular left lateral incisor, and the maxillary right second premolar and the mandibular right canine. Improved superelastic NiTi alloy wires (0.018 × 0.025 in) were used for detailing. After 3 years of edgewise appliance treatment (1.5 years after surgery), a circumferential-type retainer and a bonded retainer were placed in the maxilla, and a Hawley-type retainer and a bonded retainer were placed in the mandible. The apnea hypopnea index score was 3.1 (within the normal range). Patient compliance was excellent throughout the treatment.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


