Introduction
The hypothesis of this study was that toothpaste slurry rinsing, combined with other simple postbrushing steps (the modified fluoride toothpaste technique [MFTT]), would reduce the number of decayed and filled tooth surfaces.
Methods
The study population consisted of 100 orthodontic patients randomly divided into 2 groups, 51 in the test group (mean age, 16.2 ± 4 years) and 49 in the control group (mean age, 16.9 ± 4 years). Each patient was examined before starting orthodontic treatment (baseline) and shortly after debonding (follow-up) in a 2-year study period. At each of these 2 visits, the patients were examined in the following order: interviewed by using a standardized questionnaire, plaque index registration, intraoral clinical examination, and radiographic examination (bitewings). The test group patients were instructed to use the MFTT. The control group patients were given the same fluoridated toothpaste as the test group and the routine clinical oral hygiene instructions.
Results
Compared with the control group, the test group had significantly better plaque index scores at the end of the study. At follow-up, the clinical ( P <0.001), radiographic ( P <0.001), and clinical plus radiographic ( P <0.001) incidences of decayed and filled surfaces were significantly reduced: 87%, 78%, and 83%, respectively, in the test group compared with the control group.
Conclusions
Compared with routine oral hygiene instructions with fluoride toothpaste, the use of the MFTT significantly reduced the incidence of new carious lesions in orthodontic patients. We believe that this simple regimen should be considered in orthodontic clinics.
Fluoride toothpaste has been widely used for more than 4 decades and remains a benchmark for the prevention of dental caries. It reduces caries in both permanent and deciduous teeth. For this reason, fluoride toothpaste is important as an effective caries-prevention measure worldwide. Topical fluoride (mouth rinses, gels, or varnishes), used in addition to fluoride toothpaste, achieve a modest reduction in caries compared with toothpaste used alone. Several studies have shown that even low levels of fluoride, from the regular use of toothpaste, can have a profound effect on enamel demineralization and remineralization.
Four factors influence the anticaries efficacy of fluoride toothpaste: frequency of brushing, duration of brushing, fluoride concentration, and postbrushing rinsing. Brushing should be done twice daily, and patients should be persuaded to brush for a longer time. The salivary fluoride concentration measured after dentifrice application decreases significantly as the water rinse volume, rinse duration, and rinse frequency increase. A toothpaste technique in which a slurry rinse with the toothpaste is used after brushing increases the efficacy of the fluoride toothpaste ; it reduces approximal caries in preschool children by an average of 26%. Furthermore, eating immediately after brushing reduces the salivary fluoride level about 12 to 15 times compared with brushing alone. Postbrushing rinsing habits might play an important role in the oral retention of fluoride from dentifrices that could, in turn, affect their clinical efficacy.
Enamel demineralization associated with fixed orthodontic therapy is a rapid process caused by cariogenic microorganisms that develop around brackets and under ill-fitting bands. Despite improvements in materials and preventive efforts, demineralization can occur around orthodontic appliances after only 1 month. There is a higher risk of demineralization adjacent to brackets at earlier ages, because of the lower resistance of enamel and poorer cooperation by younger patients in the orthodontic treatment process. Children in the Kingdom of Saudi Arabia (KSA) have a high prevalence of dental caries. A recent study by Brown found a mean incidence of decayed, extracted, and filled teeth of 6.3 in healthy 5-year-old children.
Clinical trials are needed to give evidence-based advice on the optimal caries-prevention strategy, with clear practice guidelines. For orthodontic patients, more research is required into the various modes of delivering fluoride. The hypothesis of this study was that toothpaste slurry rinsing would reduce the numbers of decayed and filled tooth surfaces (DFS) in orthodontic patients.
Material and methods
A power analysis with an assumed significance level of 5%, standard deviations of 3.0 DFS, least detectable difference of 2.0 ΔDFS, and a power for that detection of 90% was performed and produced a minimum sample size of 45 observations per group.
Our subjects consisted of 150 orthodontic patients at baseline, recruited consecutively during 6 months at a private orthodontic clinic in Riyadh, KSA. They were randomly divided into 2 groups (test and control groups) with 75 patients in each. The clinic’s receptionist assigned patients with odd birth dates to the test group and patients with even birth dates to the control group. The Saudi Ministry of Health Ethics Committee approved the study. Information leaflets were given to the patients before they consented to particiapate in the study; written consent was obtained from all subjects before the trial.
Before the start of the treatment or the trial, the following information was obtained for both control and test groups by using a standardized form: frequency of brushing, amount of toothpaste, frequency of fluoride rinses, and the fluoride content of the toothpaste used. The number of meals eaten in a 24-hour period was also recorded. The information was obtained by a dentist (A.M.) who was blinded to the patients’ group.
The examination consisted of recording the plaque index according to Silness and Löe, registration of caries according to the World Health Organization’s guidelines after prophylaxis, flossing, and radiographic examination according to the method of Mejare et al, which consisted of 4 bitewings taken with double film. A total of 24 surfaces were included in the radiographic DFS index, from the distal aspect of the first premolars to the mesial surface of the second molars. Filled surfaces underlined with caries were scored as recurring caries.
After the data collection, the patients in both test and control groups received Colgate Max Cavity toothpaste containing 1450 ppm of fluoride (Colgate, Riyadh, KSA).
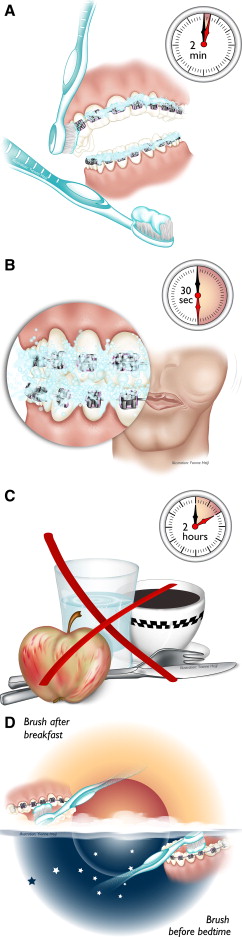
The test group received verbal and written instructions about the brushing technique: (1) use 2 cm (1 g) of dentifrice on a wet toothbrush; (2) spread the toothpaste evenly in both arches; (3) brush all surfaces for 2 minutes; (4) use a small amount of water, the equivalent of a handful with the dentifrice remaining in the mouth and filter the dentifrice slurry between the teeth by active cheek movements for 30 seconds before expectorating; (5) avoid further rinsing with water; (6) avoid drinking or eating for 2 hours; (7) brush twice a day, after breakfast and at night before going to bed; and (8) abstain from all other types of dentifrice during treatment and until its completion ( Fig 1 ). To ensure that all patients in both groups had a supply of the study toothpaste, they were given a tube at each visit or on request.
The control group was given the routine clinical oral hygiene instructions: brushing twice a day after breakfast and after dinner before going to bed, and rinsing with a fluoridated mouthwash. At each patient visit to the clinic for the treatment follow-up, the instructions were repeated by the assigned nurse or assistant.
At the end of the trial or treatment, compliance with the use of fluoridated mouthwash and the study toothpaste by the control group and the use of the toothpaste and brushing and rinsing instructions by the test group was assessed. For the test group patients, a standard form was used to rank their compliance with the duration of brushing, the frequency of brushing, the amount of water used, and the method of filtering the dentifrice slurry, and the time between brushing, rinsing, and eating. They were ranked from 1 to 5 according to the number of instructions they had followed. Of the 5 instructions, if patients followed 1 or 2, they were considered “good,” and, if they followed more than 3, they were “very good.”
Statistical analysis
The Statistical Package for Social Sciences (version 18.0, Mac OSX, SPSS, Chicago, Ill) was used for the statistical analysis of the determined measurements. ΔDFS and prevented fractions (PF) were calculated according to these 2 formulas (ΔDFS = follow-up DFS – baseline DFS) and (PF = [control group ΔDFS – test group ΔDFS]/control group ΔDFS × 100).
For the descriptive statistics, the mean values with standard deviations were calculated. To determine statistically significant differences between the groups, the independent sample t test was applied between the groups, control vs test, and good vs very good. The significance level was set at P <0.05. The paired t test was used to check intraexaminer reliability for the radiographic analysis. The 25 randomly selected radiographs were checked within a 1-week period.
Results
At the end of treatment, 50 patients were lost or excluded, leaving 100 patients. This loss did not affect the power of the study as determined by the power analysis to determine the sample size ( Fig 2 ).
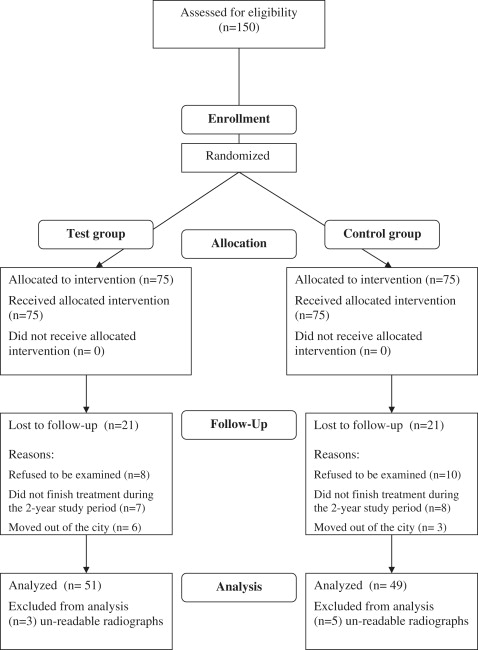
The patients were divided into the test group (n = 51;10 male, 41 female; mean age, 16.2 ± 4 years) and the control group (n = 49; 17 male, 32 female; mean age, 16.9 ± 4 years).
Intraexaminer reliability for the radiographic examination showed no significant difference ( P >0.05), indicating good reliability.
The information obtained with the standardized form by the examiner blinded to the patients’ groups showed the following for both groups at the start of the trial: 70% brushed 2 or 3 times daily; about 50% used 1 g of toothpaste, and more than 85% used only fluoride toothpaste with no other fluoride supplements; 90% had 3 to 5 meals (plus snacks) a day; and only 6% had 7 or more meals (plus snacks) a day. At follow-up, 86% of the control patients used fluoride toothpaste only, 8% used fluoride toothpaste with fluoride mouthwash infrequently, and the remaining 6% used no fluoride.
The test and control groups’ baseline and follow-up plaque index, clinical DFS, radiographic DFS, and clinical and radiographic DFS values are shown in Table I . At baseline, there were no significant differences between the groups. At follow-up, the total number of teeth available was almost the same in both groups (test, 26.9 ± 1.7; control, 26.8 ± 1.7). At the end of the study, the test group patients had significantly better plaque index scores compared with the control group ( P <0.05). Both groups had increases in their DFS index, both clinically and radiographically, with a higher increment in the control group.
| Baseline | Follow-up | |||
|---|---|---|---|---|
| Test (n = 51) | Control (n = 49) | Test (n = 51) | Control (n = 49) | |
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | |
| Plaque index | 1.4 ± 0.5 | 1.5 ± 0.6 | 1.1 ± 0.8 | 1.6 ± 0.7 |
| Clinical DFS | 5.6 ± 5.7 | 5.7 ± 5.4 | 5.8 ± 6.0 | 7.4 ± 7.7 |
| Radiographic DFS | 2.7 ± 3.0 | 2.3 ± 3.2 | 3.1 ± 3.0 | 4.1 ± 4.0 |
| Total DFS | 8.3 ± 7.5 | 8.1 ± 8.4 | 9.0 ± 8.0 | 11.6 ± 10 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


