Treatment of traumatized teeth generally occurs in two phases: short-term emergency treatment and stabilization followed by endodontic management and review. These authors recently reviewed the endodontic considerations in the treatment of traumatized permanent anterior teeth, and in this article review the early management of traumatized permanent teeth. Preoperative assessment and emergency management are emphasized, as is the treatment of immature teeth for which continued development of the root system must be encouraged. Factors influencing long-term prognosis are discussed and the influence of various management strategies evaluated.
Much literature discusses the causes and incidence of trauma to the dentition. Although most injuries occur as a result of falls and play accidents, an ever-increasing incidence of trauma from traffic accidents, sporting injuries, risk-taking activities, violence, and child physical abuse has meant that managing dental trauma has become an important part of clinical dental practice. More than 20% of children experience damage to their permanent dentition by 14 years of age, with men outnumbering women 2:1, and peak incidence at 8 to 10 years of age.
Although single-tooth injuries are most common, motor vehicle and sporting injuries often involve damage to multiple teeth. Treatment is often distressing for patients and difficult for practitioners. Several studies discuss the adverse psychological consequences of dental trauma. This article reviews the early management of traumatized permanent teeth, recommendations for which have been produced by the International Association of Dental Traumatology, the American Academy of Pediatric Dentistry, the American Association of Endodontists, and appear in numerous texts and articles.
Treatment invariably has two components: short-term emergency treatment and stabilization, and long-term endodontic management and review. The classification of dental injuries described by Andreasen and colleagues is generally followed.
Assessing traumatic dental injuries in permanent teeth
The systematic assessment of patients who have traumatic dental injuries is well covered in the literature. Emphasis has also been placed on the need for an interdisciplinary approach to management and to record a detailed and thorough history, not only to document the specific circumstances surrounding the incident but also to provide an accurate record for legal and insurance reporting. In this respect, all dental injuries should be meticulously documented and supported by appropriate sketches or photographs. Test results should be accurately recorded so reports can be written and future comparisons can be made.
Although this article addresses only the examination and management of the local dental injuries, clinicians must recognize that some dental injuries may not be accidental in nature. Injuries must be assessed vigilantly to distinguish, when possible, between accidental injuries and those resulting from abuse.
Soft tissue management
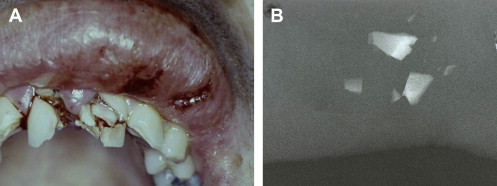
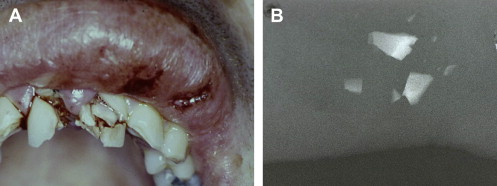
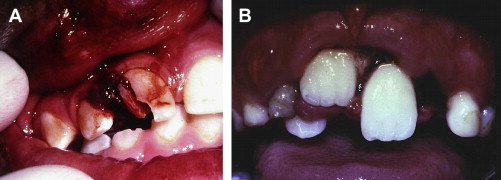
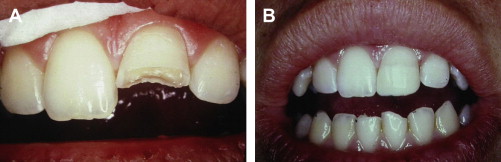
Hard tissue injuries also often involve damage to the supporting structures. When this occurs, the prognosis for the tooth (particularly with respect to the vitality of the pulp) is poorer. Any examination must include assessment of both components. Soft tissue injuries should be assessed; displaced or lacerated tissues immediately repositioned; and, where necessary, these should be sutured into place ( Fig. 1 ). When lacerations occur concomitantly with tooth fractures, tissues should be examined radiographically for the presence of embedded tooth fragments and debris ( Fig. 2 ).

Soft tissue management
Hard tissue injuries also often involve damage to the supporting structures. When this occurs, the prognosis for the tooth (particularly with respect to the vitality of the pulp) is poorer. Any examination must include assessment of both components. Soft tissue injuries should be assessed; displaced or lacerated tissues immediately repositioned; and, where necessary, these should be sutured into place ( Fig. 1 ). When lacerations occur concomitantly with tooth fractures, tissues should be examined radiographically for the presence of embedded tooth fragments and debris ( Fig. 2 ).

Bite testing
In general, if a patient can close their teeth together firmly without hurting, any fracture of the jaw or joint damage is unlikely. If the patient cannot close together firmly, the injury must be assessed to determine whether the jaw is fractured or teeth have been displaced, or both. Similarly, if a patient can open widely and simultaneously move their jaw from side to side without discomfort, any joint damage is unlikely. Pain on jaw movement must be examined closely and appropriate radiographs taken to exclude bone and joint damage.
Percussion sensitivity, percussion tone, and mobility
Teeth that are sensitive to percussion have experienced damage to the supporting tissues. If they exhibit a lower tone than normal when percussed, they have usually been extruded or loosened in their socket. Teeth that exhibit higher tone immediately after trauma are often wedged into the bone. Mobility implies loosening of the tooth within the socket. Mobility of several teeth or groups of teeth indicates an associated alveolar fracture or a fracture of the alveolar plate. Thus, in examining tooth mobility, teeth should be examined individually and teeth and groups of teeth tested against each other.
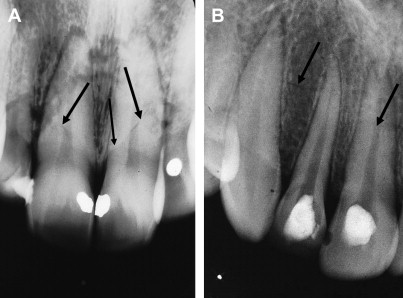
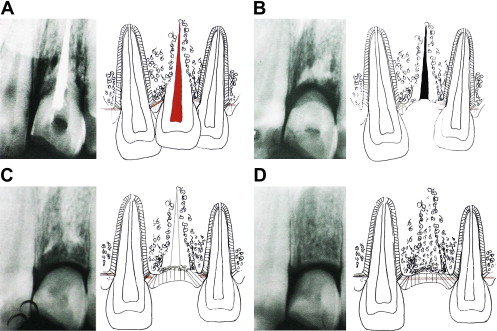
In adults, tenderness to percussion with concussed and subluxated teeth can take time (months) to settle. No emergency treatment is required except judicious grinding to free the tooth from occlusion. Prolonged sensitivity to percussion can also occur as a result of small fractures in the alveolar plate ( Fig. 3 A ). These teeth need splinting. Pulp extirpation will not relieve these symptoms (see Fig. 3 B).
Pulp sensibility testing
Response to cold testing is the most reliable and accurate way of testing teeth in children. Routine sensibility testing of the traumatized and adjacent teeth should occur as soon as possible after injury, and then at regular intervals, to form a baseline for future comparisons. Because sensibility results can be unpredictable immediately after trauma, initial testing may be delayed for a short time after injury, particularly in the presence of hemorrhage and associated soft tissue injuries, or when sensitivity to thermal stimulation or touching the exposed surface clearly indicates that the pulp is responsive.
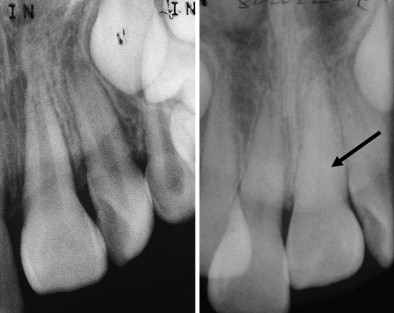
Longer observation times (≥8 weeks initially) may be required before a definitive decision can be made regarding the state of the pulp. Pulp tests only measure neural response and do not assess pulp vitality, which is dependant on blood supply. Damage to neural structures can often occur without damage to the more flexible vascular elements. Thus, although many traumatized teeth may not respond to sensibility testing, progressive radiographic changes in pulpal anatomy can show that the pulp is healthy ( Fig. 4 ). Reversals of negative sensibility testing results can occur, particularly in immature teeth and teeth with open apices. Of particular clinical importance are teeth that exhibit reversals in responses from positive to negative. Pulps in these teeth have most probably become necrotic. Necrosis will generally occur within the first 6 months of injury.
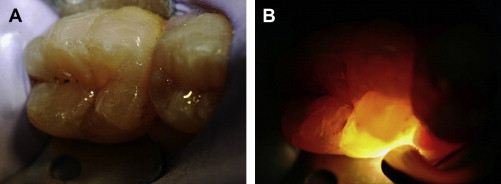
Transillumination
Using a bright light to assess for enamel cracks and detect subtle changes in color, which may not otherwise be obvious, is invaluable. Transillumination also helps to identify traumatized teeth that do not show obvious signs of trauma ( Fig. 5 ).
Type of force
An assessment of the type of force or blow that caused the trauma is sometimes overlooked. Factors to consider include the type of trauma (direct or indirect), the composition (soft, hard, resiliency) and speed of the object, the direction of the blow, and whether teeth came into contact with objects or the ground.
With indirect trauma, the upper and lower teeth are forcibly brought together. If the energy of impact is great, widespread damage occurs, often resulting in significant damage (including deep subgingival fractures) to molar teeth ( Fig. 6 A ). These injuries are difficult to manage. Subgingival crown–root fractures in anterior teeth from indirect trauma are usually labially subgingival (see Fig. 6 B).
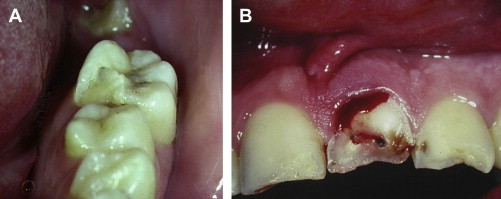
The damage occasioned to the teeth and surrounding tissues is influenced by the composition and resiliency of the impacting object. Impact with hard objects (eg, stones) results in localized site-specific injuries, with penetrating soft tissue injuries and tooth fractures in an area corresponding to the size of the object ( Fig. 7 A ).The extent of the injury is usually obvious.
The severity of the injury is directly related to the size and weight and speed of the object. Injuries that are accompanied by tooth fractures do not always result in severe damage to supporting structures or the pulp, because some of the energy of impact is absorbed by the fracture.
Resilient objects often cause more widespread injury, including displacement of soft tissues, luxation and avulsion of teeth, and bony fractures (see Fig. 7 B). The extent of the injury is less obvious and more widespread examination is required.
The direction of the impacting blow can be helpful in visualizing the extent of the injury. Dental injuries are situated distal (or away from) the point of first contact and depend on the direction of the impacting force ( Fig. 8 ). This assessment is sometimes helpful in legal reporting.
Radiographic examination
All teeth affected by the injury must be examined radiographically to ascertain the severity of the trauma, the stage of root development, injuries to the supporting structures, and the presence of root fractures. At least one “straight on” view is required for each tooth. When root fractures are suspected, several angulations are required. When supporting tissues and/or joint injuries are suspected, an orthopantomogram image is essential. Cone beam imaging is helpful for assessing intrusive injuries, bony fractures, and resorption.
Previous dental trauma
Patients often experience injuries to teeth on several occasions, as is commonly seen in patients who have a large overjet and incompetent lips. Whether any injured teeth have been previously traumatized is important to establish, because this can complicate diagnosis and influence prognosis.
The management of cracked and fractured teeth
Infraction
Infraction involves cracking of the enamel without loss of tooth structure, and is best seen with transillumination. Pulpal complications are rare (0%–3.5%) unless an associated luxation injury is present. No emergency treatment is necessary. Pulp treatment is unnecessary unless signs of irreversible pulpitis or pulp necrosis are present. Pulp sensibility testing should be performed after 3 and 12 months, and radiography performed at 12 months to assess intrapulpal calcification.
Uncomplicated Crown Fractures
In uncomplicated crown fractures, tooth structure is lost without exposure of the pulp. Pulpal complications rarely occur where only enamel is fractured (0%–1%), unless an associated luxation injury is present (8.5%). When both enamel and dentine are involved, pulpal complications are also infrequent (0%–6%), unless a concomitant luxation injury is present, wherein the incidence of necrosis can be as high as 25%.
Factors influencing pulp survival include type and site of fracture, presence of a luxation injury, type of treatment undertaken, and timing of treatment. Pulp necrosis occurs more often in deep angular fractures and deep fractures that remain untreated for more than 24 hours. Thus, dentine should be covered as soon as possible.
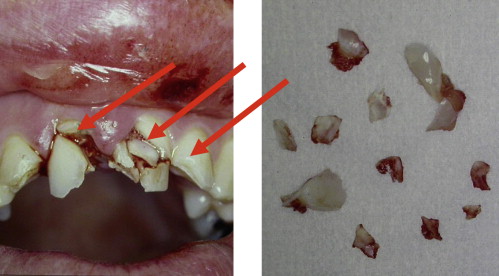
Lost tooth structure can be restored with restorative materials or through reattaching the fragment. Fragment reattachment can be a simple and very effective procedure with good longevity ( Fig. 9 ). Therefore, patients should be advised to bring fragments (and teeth) with them when presenting for treatment. Pulps can become necrotic several years after injury. Routine testing should be undertaken at to 8 weeks and then at yearly intervals.
Complicated Crown Fractures
Complicated fractures are those in which the pulp is exposed. In the absence of an associated luxation injury, pulp necrosis does not usually occur immediately, although this is the inevitable outcome if exposed pulps remain untreated. Except in immature teeth, most traumatically exposed pulps will become necrotic and infected if left untreated for 1 month. Recommended treatment procedures include pulp capping, partial pulpotomy, pulpotomy, and pulpectomy.
In young patients in whom root development is not complete, the goal of treatment is to maintain pulp vitality to allow closure of the root apex and promote root development. Preferred treatment consists of using partial pulpotomy procedures, removing a portion of the pulp (2–3 mm) with a gentle technique (high-speed diamond bur with copious water spray), eliminating blood clots (using irrigation), and capping with calcium hydroxide or mineral trioxide aggregate (MTA) ( Fig. 10 ).
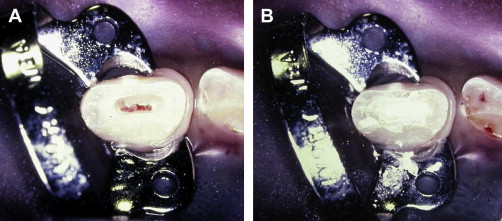
Proponents of MTA highlight that, although success rates are similar to those with calcium hydroxide, its placement is easier, it sets, it can act as a permanent restoration with a superior seal, it is unlikely to dissolve away, and it does not have to be removed later. Medicaments must be placed directly onto healthy noninflamed tissue, and the site then protected against bacteria. Regular review (at 6–8 weeks and then yearly) is recommended to assess pulp vitality and continued root development.
Although root therapy is often considered preferred treatment for mature teeth with closed apices, partial pulpotomy techniques can be useful for all traumatically fractured teeth, regardless of patient age and degree of apical closure of the teeth. This can represent considerable practical and economic advantages. Definitive restorations can be placed immediately, avoiding problems associated with temporary restoration breakdown and reinoculation of the exposure site with bacteria. The fragment can be reattached before or after root canal treatment or partial pulpotomy where possible.
Crown–root Fractures
Crown–root fractures involve enamel, dentine, and the root surface, and usually pass subgingivally. The pulp is often exposed. Factors that influence treatment planning include position and circumferential extent of the fracture, severity of the fracture in a subgingival direction, root maturity, and pulp exposure. Treatment options reviewed by Heithersay and Moule include periodontal surgery to expose crown margins; reattachment of the fragment; restorative management only with extension of margins of the restoration below the level of the gingival margin; orthodontic extrusion; intentional replantation; surgical repositioning; autotransplantation; root submergence; extraction and replacement; and orthodontic space closure. Although treatment of crown–root fractures can be complex and time consuming, many teeth can be predictably retained. Implant replacement is a viable alternative in adult patients who have severe fractures.
In younger patients, treatment priority should be development of the root rather than restoration of aesthetics and function. Dressing an exposed pulp and restoring lost tooth structure with a temporary denture is sometimes better until the root matures and restoration is practical. Reattaching the fragment (before or after pulp therapy) can stabilize the crown until the tooth erupts, bringing the subgingival margin into a more favorable position, sometimes without the need for further intervention, or until the patient reaches an age at which more definitive treatment is practical.
When a tooth is deemed unrestorable in a growing patient, decoronation ( Fig. 11 ) may be indicated to preserve bone. This procedure allows normal alveolar development before implant placement when growth is complete, and preserves labiopalatal width, which may negate the need for ridge augmentation procedures.
Root Fractures
Root fractures usually occur in a horizontal or oblique direction, and in a subgingival or infrabony position. Although they can present without clinical signs of crown displacement, the crown is usually extruded and lingually displaced. The radiographic appearance is influenced by the position of the fracture and the direction of the beam. Fractures can be single or multiple and appear radiographically as single or multiple lines across the root. Multiple radiographic views at different angles may be required to obtain clear images of the fracture. A high oblique or occlusal view is useful.
The presence of a root fracture is not an indication for endodontic treatment; this is only required if pulp necrosis has occurred. Many root-fractured teeth survive without treatment. Pulp survival rates are higher in root-fractured teeth than in traumatized teeth without fracture. Many heal without intervention in one of three modalities: hard tissue interposition; interposition of bone and periodontal ligament; and interposition of periodontal ligament alone. Healing is more favorable in incompletely formed teeth and when displacement of the coronal fragment is minimal. The occurrence of pulp necrosis is significantly higher if the fragments are separated more than 1 mm (suggesting that 1 mm is the limit to which the pulpal tissue can be stretched before the neural and vascular components become compromised). Calcification of the pulp canal, often erroneously called “pulp canal obliteration,” is a common feature that may develop in root-fractured teeth. This condition is rarely a problem in the long-term and can only develop if tissues in the pulp maintain their vitality.
A nonhealing inflammatory process associated with pulp necrosis and infection of the coronal fragment can also occur. The probability of this occurring is affected by apical maturation, location of the fracture, extent of dislocation, and separation between the fragments. If necrosis develops (20%–44% of cases), it is generally detectable after 2 to 5 months. Invariably, only the coronal fragment becomes necrotic as the blood supply to the apical fragment remains intact.
Responses to thermal and electrical tests immediately after trauma are an unreliable means of predicting final outcomes. Diagnosis of pulp status occurs later and is based on development of radiolucency at the fracture site and presence of a sinus or coronal discoloration. Resorption apically or at the fracture site does not indicate necrosis.
Root fractures rarely occur in immature teeth; these teeth are more likely to be luxated or avulsed. Root fractures in immature teeth are often irregular and have a vertical and horizontal component. As the pulp is large and developmentally active, calcific healing usually occurs without the need for any intervention.
Appropriate treatment for root fractured teeth is assessed in two stages: at initial presentation to determine communication, displacement, and mobility, and several months later to assess pulp status mobility and healing of root-fractured teeth.
Initial presentation
If the fracture line is communicating with the oral cavity, the coronal fragment is removed and the remaining tooth structure treated on its merits. If the fracture line is not communicating with the oral cavity, the coronal fragment is assessed for displacement and mobility. If the fragment is mobile or displaced, it should be splinted immediately. Early and accurate repositioning reduces the likelihood of pulp necrosis. Radiographic confirmation of the accuracy of repositioning is helpful. Splinting should be non-rigid, atraumatically placed and removed after 4 weeks, except in teeth that have fracture occurring in the coronal third, which may need splinting for up to 4 months.
If the fracture does not communicate with the gingiva and is not mobile or displaced, no treatment is necessary. Endodontic management is not part of the initial treatment of root-fractured teeth. Percussion-sensitive root-fractured teeth can be splinted to alleviate symptoms. Pulp removal from a percussion-sensitive, vital root-fractured tooth will not generally relieve discomfort.
Later assessment
Unless symptoms dictate, assessment of the pulp status and healing of root-fractured teeth can be delayed for several months. Important considerations at this review appointment are pulp vitality and tooth mobility.
If signs of pulp necrosis and infection (radiographic evidence of bone loss at the fracture site, development of a sinus or tooth discoloration) are present, the pulp is removed down to the fracture site and apexification procedures involving the use of calcium hydroxide and/or MTA are instituted. Initial endodontic procedures should not extend beyond the fracture line. If the tooth remains mobile, long-term splinting is considered. In the absence of mobility or pulp necrosis, no treatment is undertaken.
Follow-up radiographs should be taken at 1 month, 2 months, and 6 months, and then at yearly intervals.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


