Three-dimensional imaging offers many advantages in making diagnoses and planning treatment. This article focuses on cone beam CT (CBCT) for making diagnoses and planning treatment in trauma-related cases. CBCT equipment is smaller and less expensive than traditional medical CT equipment and is tailored to address challenges specific to the dentoalveolar environment. Like medical CT, CBCT offers a three-dimensional view that conventional two-dimensional dental radiography fails to provide. CBCT combines the strengths of medical CT with those of conventional dental radiography to accommodate unique diagnostic and treatment-planning applications that have particular utility in dentoalveolar trauma cases. CBCT is useful, for example, in identifying tooth fractures relative to surrounding alveolar bone, in determining alveolar fracture location and morphology, in analyzing ridge-defect height and width, and in imaging temporomandibular joints. Treatment-planning applications include those involving extraction of fractured teeth, placement of implants, exposure of impacted teeth, and analyses of airways.
Three-dimensional imaging offers many advantages in making diagnoses and planning treatment. This article focuses on cone beam CT (CBCT) for making diagnoses and planning treatment in trauma-related cases. CBCT equipment is smaller and less expensive than traditional medical CT equipment and is tailored to address challenges specific to the dentoalveolar environment. Like medical CT, CBCT offers a three-dimensional view that conventional two-dimensional dental radiography fails to provide. CBCT combines the strengths of medical CT with those of conventional dental radiography to accommodate unique diagnostic and treatment-planning applications that have particular utility in dentoalveolar trauma cases. CBCT is useful, for example, in identifying tooth fractures relative to surrounding alveolar bone, in determining alveolar fracture location and morphology, in analyzing ridge-defect height and width, and in imaging temporomandibular joints. Treatment-planning applications include those involving extraction of fractured teeth, placement of implants, exposure of impacted teeth, and analyses of airways.
In hospital settings, it is common to use CT in patients with trauma and pathologic conditions. However, in dental practice, practitioners depend almost entirely on two-dimensional plain films. The applications and advantages of the third dimension in dental medicine still remain largely unrealized.
In 1998, Mozzo and colleagues reported on the NewTom 9000 (Quantitative Radiology, Verona, Italy), the first CBCT unit developed specifically for dental use. Other similar devices introduced at around that time included the Ortho-CT, which was renamed the 3DX (J. Morita Mfg. Corp., Kyoto, Japan) multi-image micro-CT in 2000. In 2003, Hashimoto and colleagues reported that the 3DX CBCT produced better image quality with a much lower radiation dose than the then newest multidetector row helical CT unit (1.19 mSv versus 458 mSv per examination).
Two major differences distinguish CBCT machines from conventional hospital CT scanners (helical, spiral, fan). First, CBCT uses a low-energy fixed anode tube, similar to that used in dental panoramic radiograph machines. Second, CBCT machines rotate around the patient only once, capturing the data using a cone-shaped x-ray beam. These differences make possible a less-expensive, smaller machine that exposes the patient to approximately 20% of the radiation of a helical CT, which is equivalent to a typical exposure from a full-mouth periapical series. The volumetric capturing difference provides CBCT with a more focused beam, resulting in images with higher geometric accuracy, higher spatial resolution, and considerably less scattering in comparison with images from conventional CT scanners. One disadvantage of the volumetric capturing method is that the Hounsfield units, which provide density information, cannot currently be captured in a reliable fashion when using CBCT. Ongoing projects are working on such calibration, but no method is currently commercially available.
Due to CBCT’s volumetric data capturing method, related articles have referred to this technology with a variety of terms including cone beam volumetric tomography, cone beam computed volumetric tomography, cone beam volumetric radiography, dental CT, dental volume tomography, digital volumetric tomography, and cone beam 3D. This multiplicity of terms stems largely from disagreement over whether CBCT capturing methods can truly be called tomography. The result is a lack of terminology consensus in the literature, making it more difficult for researchers and clinicians to stay up to date with the latest projects and publications because different key words need to be searched.
All of the CBCT scanners on the market use the same volumetric capturing technology, but have significant hardware differences. Scanners can be categorized according to type of detector, patient position (sitting, standing, or supine), field of view, the use of fixed radiation settings or user-controlled settings, and whether or not the scanner is dedicated or hybrid. The detector can be either an amorphous silicon flat-panel detector or a combination of an image intensifier and a charge-coupled device camera. Both these technologies have been proven to be accurate and reliable and provide sufficient resolution for dental medicine needs. The field of view stands for the final image size produced by the scanner. Different scanners offer different field-of-view capabilities resulting in images ranging in size from 1 in to 12 in. To best accommodate collimation capabilities and reduced radiation exposure as much as possible, the field of view used should match the region of interest. In other words, if all the clinician wants is to evaluate an area of suspected fracture, the relationship of the alveolar ridge to an impacted tooth, or area of suspected pathology, there is no need to capture an image that would show the patient’s entire head. Some scanners offer both large and small field-of-view capabilities, while others, tailored for more specific applications, offer only small field-of-view capabilities.
A significant lack of standardization found in the commercially available CBCT scanners has to do with the radiological settings. Depending on the scanner, the milliamperage used may range from 1 mA to 15 mA, with most scanners using around 6 mA. Often the radiological settings are fixed and cannot be changed without the intervention of the manufacturer’s engineers. So radiation exposure depends largely on the scanner used, since it plays an important role on the settings used.
Effective CBCT radiation dose depends on the settings used (kilovolt [peak] and milliampere), collimation, and exposure time. The use of lower settings reduces the radiation dose received by the patient, but could also diminish image quality. The choice should always be the lowest possible settings that also accommodate a diagnostic-quality image. However, specific settings for different clinical applications have yet to be determined. This can only be done by considering the image quality because radiation exposure information without image quality control is just half the story. The settings, including milliampere, kilovolt (peak), and field of view, are going to be different for different clinical applications. For example, as the settings for diagnostic screening will differ from those for implant planning. Settings should be consistent among imaging centers, and the scanners should have such settings as options. This is the only way to efficiently apply the ALARA (as low as reasonably achievable) principle.
Within every field, the introduction of new technology raises several fundamental questions, such as: For what practical applications can the new technology be used? and: Is the new technology truly superior to existing modalities? These questions are not easily answered, but require research and comparison. CBCT diagnostics in posttraumatic clinical applications appear to offer advantages over medical CT and conventional dental radiography.
Because all images can be taken in around 10 seconds with a single rotation of the x-ray source, CBCT is useful in trauma, intraoperative, and sedation cases.
Clinical applications in trauma diagnosis: overcoming conventional CT diagnostic challenges and adding a new dimension to conventional radiography
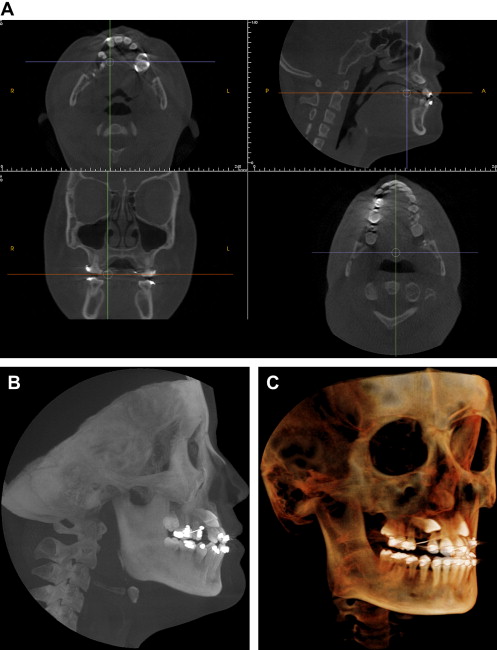
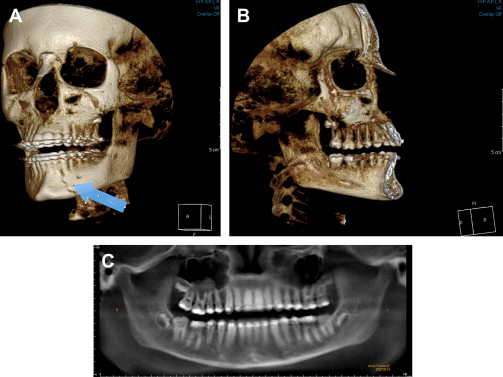
CBCT equipment is smaller and less expensive than medical CT equipment and is particularly well suited to evaluating the jaws because of a lower level of metal artifacts in reconstructions versus its helical predecessor. In a conventional CT, for instance, an area of the jaws close to a metallic restoration, a crown, or an implant is difficult to analyze because of the artifacts and distortions that the metal in the region of interest creates. On a CBCT image, the area around metal is usually of diagnostic quality, and with little scattering and no distortion ( Fig. 1 ). When compared with dental panoramic radiograph, CBCT is useful in identifying the location of cortical plate fracture that is not through and through ( Fig. 2 ). Additionally, CBCT is more sensitive and accurate in imaging the maxilla and mandible. It is reported that mandibular fractures not evident in conventional CT can be identified using CBCT. Also, when using CBCT, as compared to CT and conventional radiograph, information about dentoalveolar fractures is more detailed. This makes CBCT uniquely useful in alveolar fracture diagnosis.