A transverse maxillary deficiency in an adult is a challenging problem, especially when it is combined with a severe anteroposterior jaw discrepancy. The demand for nonsurgical maxillary expansion might increase as patients and clinicians try to avoid a 2-stage surgical procedure—surgically assisted rapid palatal expansion followed by orthognathic surgery—and detrimental periodontal effects and relapse. In this regard, a miniscrew-assisted rapid palatal expansion was devised and used to treat a 20-year-old patient who had severe transverse discrepancy and mandibular prognathism. Sufficient maxillary orthopedic expansion with minimal tipping of the buccal segment was achieved preoperatively, and orthognathic surgery corrected the anteroposterior discrepancy. The periodontal soundness and short-term stability of the maxillary expansion were confirmed both clinically and radiologically. Effective incorporation of orthodontic miniscrews for transverse correction might help eliminate the need for some surgical procedures in patients with complex craniofacial discrepancies by securing the safety and stability of the treatment, assuming that the suture is still patent.
Transverse maxillary deficiency is a relatively common clinical problem. It has been reported that 9.4% of whole populations and nearly 30% of adult orthodontic patients have a maxillary transverse deficiency related to a posterior crossbite. Although rapid palatal expansion (RPE) has been a reliable treatment modality in prepubertal patients, there have been controversies regarding nonsurgical expansion in adults. Surgically assisted RPE (SARPE) has been the treatment of choice to resolve the high resistance from the bony palate and the zygomatic buttress, in contrast to reports of successful nonsurgical expansion in young adults. The difficulties in dealing with the transverse discrepancy are associated with the limited range of tooth movement in the transverse dimension, described by Proffit et al as the “transverse envelope of discrepancy.”
Maxillary constriction combined with severe anteroposterior discrepancy is challenging, because it usually requires 2 surgeries: SARPE followed by orthognathic surgery. Since many patients are reluctant to undergo multiple surgical procedures, the demand for nonsurgical treatment might increase. However, even though nonsurgical palatal expansion is feasible, ample orthopedic expansion of the basal bone rather than dentoalveolar tipping is essential to prevent detrimental periodontal effects such as bony dehiscence and to establish proper posterior occlusion. In this regard, the appliance should be designed appropriately to maximize the skeletal effects.
Since conventional rapid palatal expanders that are either tooth-borne (hyrax type) or tooth-and-tissue-borne (Haas type) cause questionable effects on the basal bone, a rigid element that delivers the expansion force directly to the basal bone could be a solution. For this purpose, a miniscrew-assisted rapid palatal expander (MARPE) was designed and used in an adult patient. This case report shows the treatment effects and stability of the MARPE in a patient with severe maxillary constriction and mandibular prognathism.
Diagnosis
A 20-year-old man had severe mandibular prognathism. His past medical and dental histories were not remarkable. Initial intraoral and extraoral views shiwed a severe Class III malocclusion and a concave profile with a protrusive mandible and a retrusive maxilla ( Fig 1 ). The severe bilateral buccal crossbite was associated with relative constriction of the maxilla ( Fig 2 ). The crossbite remained when the casts were repositioned to a Class I molar relationship, indicating an absolute transverse deficiency. Maxillary and mandibular intermolar widths were 42.0 and 44.5 mm, respectively, indicating that about 8 mm of maxillary expansion was needed to establish proper buccal occlusion. Excessive buccal tipping of the maxillary second molars was also noted. Incisor overbite was +4.5 mm, and overjet was –7.0 mm ( Fig 3 ).
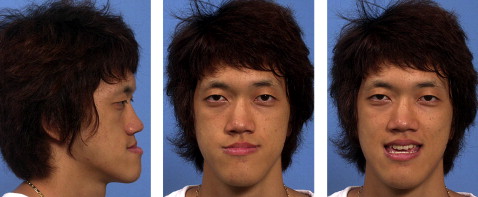

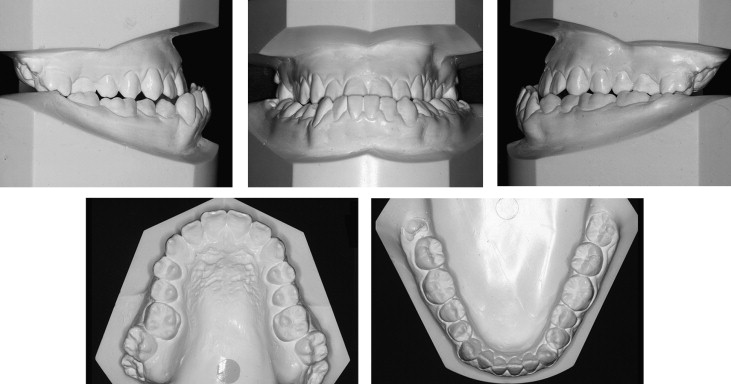
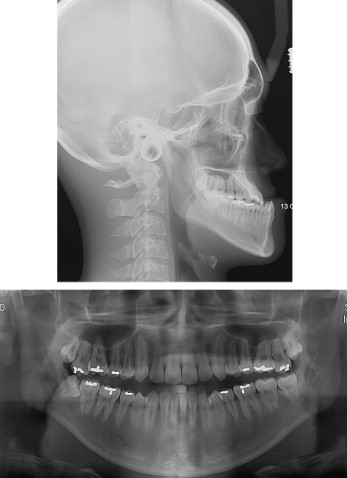
The initial lateral cephalometric analysis showed a severe anteroposteior discrepancy with an ANB of –9.0°, SNA of 82.9°, and SNB of 91.9°, and dental compensation represented by U1 to SN of 117.0° and IMPA of 74.0°. The Wits appraisal was –20.5 mm. The SN-MP angle was relatively low (28.7°) ( Fig 4 , Table ).
| Measurements | Mean | T0 | T1 | T2 |
|---|---|---|---|---|
| Lateral cephalogram | ||||
| SNA (°) | 81 | 82.9 | 82.9 | 84.5 |
| SNB (°) | 78 | 91.9 | 92.0 | 83.0 |
| ANB (°) | 3 | –9.0 | –9.1 | 1.5 |
| Wits (mm) | –2 | –20.5 | –19.5 | –4.5 |
| SN-GoGn (°) | 35 | 28.7 | 29.7 | 37.7 |
| U1 to SN (°) | 106 | 116.4 | 111.4 | 106.5 |
| L1 to GoGn (°) | 94 | 74.0 | 80.0 | 80.1 |
| Upper lip to E-line (mm) | 1 | –8.8 | –8.3 | –0.2 |
| Lower lip to E-line (mm) | 2 | 2.5 | 3.5 | 2.0 |
| PA cephalogram | ||||
| Nasal cavity width (mm) | NA | 66.8 | 69.0 | 68.4 |
| Maxillary basal bone width (mm) | NA | 34.0 | 36.5 | 36.0 |
From the posteroanterior (PA) cephalometric analysis, the maxillary basal bone width measurement was 66.8 mm, and interantegonial notch width was 96.0 mm, with resultant a maxillomandibular differential of 29.2 mm ( Table ).
Treatment objectives
The treatment objectives were to (1) correct the maxillary deficiency with sufficient maxillary expansion, (2) maintain sound periodontal support in the maxillary arch throughout treatment, (3) establish an esthetic profile with maxillomandibular orthognathic surgery, and (4) establish proper buccal occlusion.
Treatment objectives
The treatment objectives were to (1) correct the maxillary deficiency with sufficient maxillary expansion, (2) maintain sound periodontal support in the maxillary arch throughout treatment, (3) establish an esthetic profile with maxillomandibular orthognathic surgery, and (4) establish proper buccal occlusion.
Treatment alternatives
Because of the severe anteroposterior jaw relationship, orthognathic surgery was inevitable. Accordingly, several treatment options were suggested to deal with the transverse discrepancies.
A SARPE before orthognathic surgery can be a reliable treatment option. Because of the severe maxillomandibular discrepancy and the midface deficiency, 2-jaw surgery with a LeFort I osteotomy was indicated. However, since SARPE and maxillary LeFort I osteotomy cannot be performed simultaneously, the patient would require 2 stages of surgery. The possible increases in surgical trauma and costs were concerns.
Maxillary segmental osteotomy for bilateral expansion of the maxillary posterior segments with the mandibular surgery was also considered to correct both the transverse and anteroposterior skeletal discrepancies in 1 surgery. However, lateral movements of the maxillary segment have been shown to be considerably unstable.
Extraction of the maxillary premolars can be a solution to reduce the relative discrepancy between the maxillary and mandibular buccal segments, since it results in a full-step Class II molar relationship. In this patient, however, the transverse discrepancy at the molar width was still there when the diagnostic casts were repositioned in a Class II relationship. Furthermore, incisor retraction would have prolonged the overall treatment. The increase in the negative overjet after maxillary incisor retraction would then necessitate excessive surgical jaw movement that could be detrimental for the stability of the surgery.
Sufficient orthopedic expansion of the maxilla could eliminate the need for invasive surgery, if appropriately performed. However, in this patient, maximum skeletal expansion without severe dental tipping and undesired periodontal side effects would be necessary, and the results would need to be stable after treatment. Special considerations were needed in designing the appliance for nonsurgical expansion.
Treatment progress
A MARPE was fabricated with some modification of the conventional RPE. An impression was made with the bands on the first premolars and first molars, and a conventional hyrax expander was constructed on the cast. Four rigid connectors of stainless steel wire with helical hooks were soldered on the base of hyrax screw body. Two anterior hooks were positioned on the rugae region, and the other 2 posterior hooks were placed on the parasagittal area ( Fig 5 , A ). The hooks were adjusted for passive contact with the underlying tissues. The MARPE was then placed and cemented on the patient’s first premolars and molars. Orthodontic miniscrews (Orlus, Ortholution, Seoul, Korea) with a 1.8-mm collar diameter and a 7-mm length were placed in the center of the helical hooks under local infiltration anesthesia. The wires were adjusted to maintain passive contact with the collar of the miniscrews. Nonsteroidal anti-inflammatory drugs were prescribed for pain control ( Fig 5 , B ).




