A 19-year-old man with a skeletal Class III malocclusion was treated using minimal presurgical orthodontics. Orthodontic appliances and miniscrews were placed at the beginning of treatment, and the double-jaw-surgery was performed once the maxillary right and left first premolars were intruded, without worsening the concave profile and facial asymmetry presurgically. Different from the traditional combined orthodontic-orthognathic surgery, the jaw discrepancy was corrected first, followed by the orthodontic tooth movement. Miniscrews were used to intrude the premolars presurgically because of their interference and to provide the skeletal anchorage for intermaxillary elastics after the operation. The patient was pleased with the treatment results and satisfied with his facial and dental appearance, as well as his oral function. The 1-year follow-up photographs show a stable result both esthetically and functionally.
Highlights
- •
We treated a skeletal Class III patient with minimal presurgical orthodontics.
- •
We combined the surgery-first approach with miniscrews.
- •
This report includes records at pretreatment, progress, and posttreatment.
- •
The quality of the records was a high priority.
Patients with a skeletal Class III malocclusion always complain of an unharmonious profile and poor biting of their occlusion. Most of them are more concerned with their unpleasing dental and facial appearances than with a functional deficiency. It is well documented that these patients typically suffer from low confidence and even self-contempt, which affects their mental and social well-being.
Traditionally, combined orthodontic-orthognathic surgery was performed for patients with a severe Class III malocclusion, sequenced by presurgical orthodontics, orthognathic surgery, and postsurgical orthodontic treatment. However, aligning and leveling during preoperative treatment is a time-consuming process, and patients are subjected to progressive deterioration of their facial appearance and function caused by decompensation of the maxillary and mandibular anterior teeth.
To address the patients’ chief complaint, a surgery-first approach, involving surgical-orthodontic treatment without preoperative orthodontic treatment, was proposed. The surgery-first approach changes the facial appearance at the beginning but also increases the risk of relapse because of the lack of a relatively stable occlusion. It has been demonstrated that a stable occlusion is one of the most important factors for preventing postoperative relapse.
Considering these advantages and disadvantages, minimal presurgical orthodontics (0-6 months) has been proposed to eliminate the postsurgical occlusive interference and to produce a relatively stable postoperative occlusion. The treatment details vary among individual institutes.
In this article, we report on a comprehensive surgical-orthodontic treatment with minimal presurgical orthodontics for a skeletal Class III adult with mandibular asymmetry. Miniscrews were used as skeletal anchorage to correct minor surgical interferences to prevent relapse tendencies after the jaw operation.
Diagnosis and etiology
A 19-year-old man came with chief complaints of underbite and facial asymmetry. His medical and dental histories were not significant, but his mother had a protrusive mandible without an anterior crossbite. Heredity was considered one factor in the cause of the patient’s malocclusion.
The facial photographs showed a maxillary deficiency and severe mandibular protrusion with an unesthetic smile ( Fig 1 ). In the frontal view, the lower third of the face was elongated with the chin shifted to the right by 4 mm. The nasolabial angle and the mentolabial sulcus were unattractive.
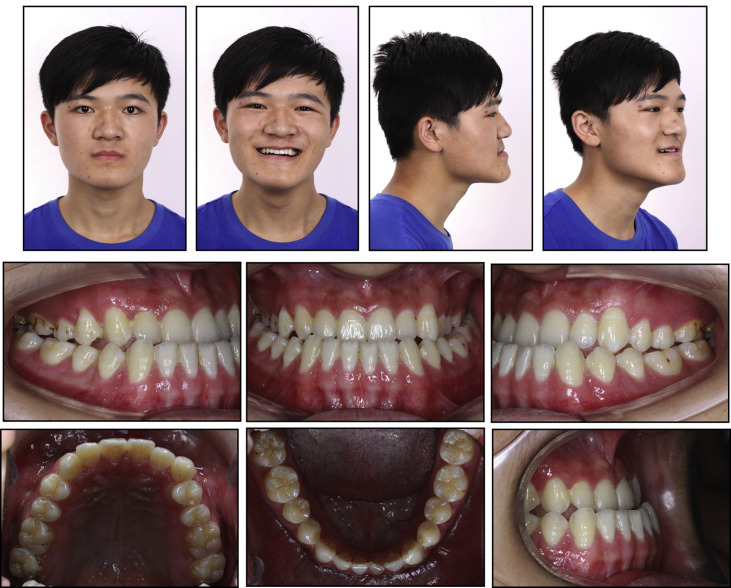
The intraoral examination of the molar relationships showed full Class III on the left side and cusp-to-cusp Class III on the right side ( Figs 1 and 2 ). The mandibular midline deviated 2 mm toward the right. Mild crowding in both arches and an anterior and transverse bilateral crossbite with a negative overjet (−4 mm) were evident. Extrusion of the maxillary first premolars was observed. There were no obvious clinical symptoms or signs in the temporomandibular joint examination.
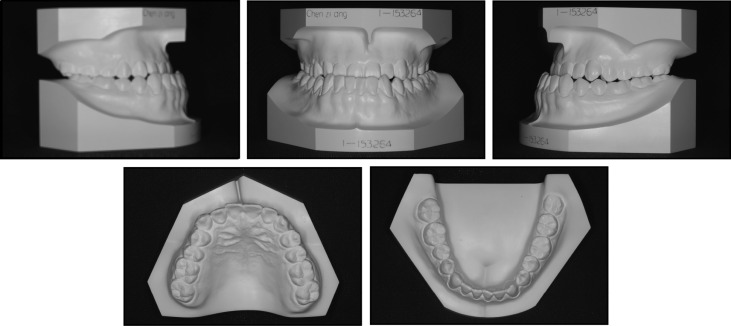
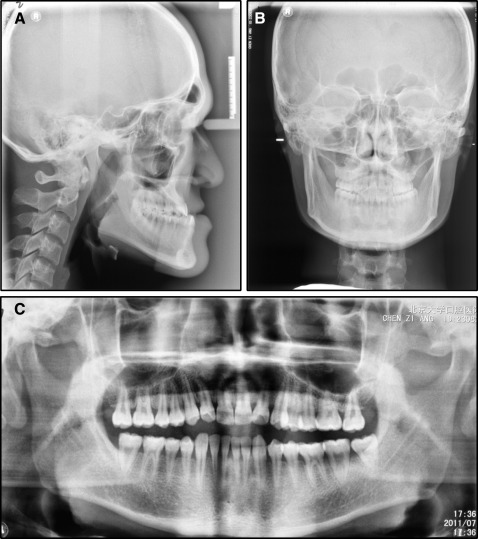
The lateral cephalometric analysis indicated a skeletal Class III relationship with a decreased ANB angle of −9.01° ( Fig 3 ; Table I ). Compensating for the Class III skeletal pattern, the maxillary incisors were proclined, and the mandibular incisors were retroclined. A posteroanterior radiograph showed mandibular asymmetry, with the chin deviated to the right. The panoramic film and regional cone-beam computed tomography image suggested no pathologic changes of the temporomandibular joint.
| Measurement | Norm | Pretreatment | Posttreatment |
|---|---|---|---|
| SNA (°) | 82.80 ± 4.00 | 81.04 | 83.71 |
| SNB (°) | 80.10 ± 3.90 | 90.71 | 82.86 |
| ANB (°) | 2.70 ± 2.00 | −9.67 | 0.85 |
| FH-NP (mm) | 85.40 ± 3.70 | 98.02 | 88.32 |
| NA/PA (°) | 6.00 ± 4.40 | −23.70 | −8.87 |
| U1-NA (mm) | 3.50 ± 6.50 | 8.80 | 6.24 |
| U1/NA (°) | 22.80 ± 5.70 | 36.57 | 33.02 |
| L1-NB (mm) | 6.70 ± 2.10 | 0.26 | 4.56 |
| L1/NB (°) | 30.50 ± 5.80 | 2.22 | 15.39 |
| U1/L1 (°) | 124.20 ± 8.20 | 150.88 | 130.75 |
| U1/SN (°) | 105.70 ± 6.30 | 117.61 | 116.73 |
| MP/SN (°) | 32.50 ± 5.20 | 25.22 | 24.78 |
| MP/FH (°) | 31.10 ± 5.60 | 19.85 | 24.48 |
| L1/MP (°) | 93.90 ± 6.20 | 66.29 | 87.75 |
| Y (°) | 66.30 ± 7.10 | 56.42 | 64.22 |
| Pg-NB (mm) | 1.00 ± 1.50 | 4.00 | 10.43 |
Treatment objectives
Because the patient was eager to alter his facial appearance without experiencing progressive deterioration, we proposed a minimal presurgical orthodontic treatment. In terms of facial esthetics, the objectives were to (1) improve upper lip projection and paranasal support, (2) reduce the lower facial height, and (3) and create a straight profile. The overall objectives aimed at function and stability, in addition to esthetics, were to (1) eliminate any prominent occlusal interferences before surgery, (2) advance the maxilla, (3) set the mandible back and correct facial asymmetry simultaneously, (4) level and align both the maxillary and mandibular dentitions, (5) relieve the compensation, (6) and establish a Class I molar and canine relationship with ideal overjet and overbite.
Treatment objectives
Because the patient was eager to alter his facial appearance without experiencing progressive deterioration, we proposed a minimal presurgical orthodontic treatment. In terms of facial esthetics, the objectives were to (1) improve upper lip projection and paranasal support, (2) reduce the lower facial height, and (3) and create a straight profile. The overall objectives aimed at function and stability, in addition to esthetics, were to (1) eliminate any prominent occlusal interferences before surgery, (2) advance the maxilla, (3) set the mandible back and correct facial asymmetry simultaneously, (4) level and align both the maxillary and mandibular dentitions, (5) relieve the compensation, (6) and establish a Class I molar and canine relationship with ideal overjet and overbite.
Treatment alternatives
According to the treatment objectives, the treatment alternatives proposed to the patient were the following.
- 1.
Camouflage treatment was possible to correct the dental anteroposterior discrepancy by maximizing the maxillary and mandibular dentoalveolar compensation. This protocol could involve extracting the mandibular third molars to permit uprighting the posterior teeth and retracting the anterior teeth. Miniscrews in the retromolar region might be considered to further distalize the entire mandibular dentition. Although the risk and cost of this option were lower, the patient’s main concern about esthetic improvement would not be addressed. Moreover, for a severe skeletal malocclusion, the outcome with compensating treatment would be unstable.
- 2.
Routinely combined surgical and orthodontic treatment with maxillary advancement and mandibular setback was proposed to obtain the overall objectives. However, the patient would experience progressive deterioration of his facial appearance during the leveling, aligning, decompensating, and space-closing stages before surgery could be carried out. This could have negative effects on his psychological well-being.
- 3.
In the surgery-first approach, no active presurgical orthodontic alignment would be performed. The patient would have surgery to correct the skeletal discrepancy at the beginning, without degrading his facial appearance. However, there could be instability, and the outcome would be unpredictable.
- 4.
Minimal presurgical orthodontic treatment with the aid of miniscrews was proposed to eliminate the obvious occlusal interferences on the study model, decrease the instability of the postsurgical occlusion, and increase the predictability of the surgical results. Most of the orthodontic treatment, including aligning, leveling, decompensating, space closing, and detailing, would be done postoperatively.
Informed of the positive and negative reasons of these treatment alternatives ( Table II ), the patient chose the fourth option because he wanted his facial appearance improved quickly. Therefore, minimal presurgical orthodontics followed by surgery was performed to correct his facial esthetics and malocclusion.
| Advantages | Disadvantages | |
|---|---|---|
| Camouflage treatment | 1. To correct the dental anteroposterior discrepancy 2. To avoid a surgical insult 3. To decrease treatment risk and cost |
1. No positive effect on esthetic and psychosocial well-being 2. Unstable outcome for a severe skeletal malocclusion |
| Routinely combined surgical and orthodontic treatment | 1. To significantly change the facial appearance and malocclusion 2. To establish a stable occlusion after the operation |
1. Progressive deterioration of facial appearance and oral function during presurgical orthodontics 2. Negative effect on psychosocial well-being |
| Surgery-first approach | 1. To obtain a major improvement in the profile at the beginning 2. To eliminate an exaggerated anterior crossbite by incisor decompensation 3. To perform postoperative decompensation more effectively and efficiently |
1. Difficulty in obtaining a stable occlusion immediately after the operation 2. Difficulty in predicting the postsurgical results |
| Minimal presurgical orthodontics | 1. To correct a skeletal discrepancy at an earlier stage and minimize deterioration of facial profile 2. To eliminate obvious occlusal interferences, decrease postsurgical instability and unpredictability 3. To perform postsurgical decompensation more effectively and efficiently |
1. Dependence on experienced and skilled surgeons and orthodontists |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


