Microbiology of dental caries
Publisher Summary
Dental caries can be thought of as a chronic infection in which the microbial agents are members of the normal commensal flora. Lesions result from the demineralization of enamel and later of dentine by acids produced by plaque microorganisms as they metabolize dietary carbohydrates. Once the surface layer of enamel has been lost, the infection invariably progresses via dentine with the pulp becoming firstly inflamed and later necrotic. Dental caries is ubiquitous, and while its prevalence is falling in most developed countries, the opposite is true in the underdeveloped countries where recent changes in diet, especially with respect to carbohydrate content, have occurred.There is a vast literature about the aetiology, diagnosis, management and prevention of dental caries; in this short chapter only the main factors can be discussed.
Clinical presentation and diagnosis
The earliest clinical appearance of caries is a well-demarcated chalky-white lesion (Figure 4.1), in which the surface continuity of enamel is still intact. This so called ’white spot’ lesion can heal or remineralize with the result that this stage of the disease is reversible. However, as the lesion develops, the surface becomes roughened and cavitation occurs. If the lesion is untreated, microorganisms extend the disease into dentine and often finally destroy the dental pulp.

Aetiology
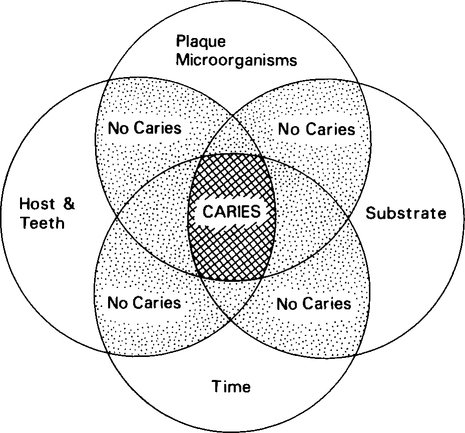
The four main factors involved in dental caries are the host, supragingival plaque, diet and the time necessary for caries development (Figure 4.2). These complex factors can interact in numerous different ways but all are required for the initiation and progression of carious lesions. It is important to realize that the way in which these factors interact is of prime importance in determining if an early carious lesion will occur and if it will subsequently heal or progress.
Host factors
Saliva performs a number of important roles in maintaining dental health, some which are related to dental caries (see Chapter 3). For example, the mechanical washing action of saliva is a very effective mechanism in removing food debris and unattached oral microorganisms from the mouth. The importance of this factor is highlighted in patients with severe Sjögren’s syndrome (a degenerative disease of salivary glands) who have a very low salivary flow rate, retain food debris in their mouth for long periods and suffer from rampant dental caries. Saliva has a high buffering capacity which tends to neutralize acids produced by plaque bacteria on tooth surfaces. It is also supersaturated with calcium and phosphorus which are important in the remineralization of white spot lesions; fluoride is also important in this process.
The roles of the other salivary antimicrobial factors in dental caries, e.g. lysozyme, the lactoperoxidase system and immunoglobulins (see Chapter 3), are not clear.
Microbiology
Dental caries does not occur in vivo if microorganisms in the form of dental plaque are absent. The different types of plaque and the factors involved in their development have been described in Chapter 3 and will not be repeated here. Over the years there has been debate about whether one or more specific bacteria are principally involved in the initiation of caries or if the disease is caused by a non-specific mixture of bacteria. At present, a number of different opinions exist, for example: (1) Strep. mutans is involved in the initiation of almost all carious lesions in enamel; (2) Strep. mutans is important, but not essential, in the aetiology of the disease; and (3) the association of Strep. mutans and caries is weak and no greater than for other bacteria in supragingival plaque. The evidence advanced to support or disprove these different opinions is incomplete and it is likely that all three may be correct in specific circumstances. Given the extreme variation found in the microbial composition of supragingival plaque collected from the same site in the same mouth with respect to time, it seems unlikely that the initiation and progression of all carious lesions are associated with identical or even similar plaques. However, there is evidence that overall some bacteria (Strep. mutans, Lactobacillus spp. and Actinomyces spp.) are more important than others.
Streptococcus mutans
A substantial volume of research has been carried out to investigate the role of Strep. mutans in dental caries. Surprisingly, few other bacterial species have been investigated in the same depth during the past 10–15 years, and this fact may partly explain the apparently overwhelming evidence of the prime importance of Strep. mutans in caries. Strep. mutans is a group name; in fact the group consists of six different species (Strep. mutans, Strep. sobrinus, Strep. cricetus. Strep. ferus, Strep. rattus and Strep. macacae) and eight serotypes (a–h). Strep. mutans (serotypes c/e/f) and Strep. sobrinus (serotypes d/g) are the species most commonly found in humans, with serotype c strains being most frequently isolated, followed by d and e, the others being rarely encountered. The evidence for the aetiological role of Strep. mutans in dental caries is shown in Table 4.1.
Table 4.1
Factors related to the cariogenicity of Streptococcus mutans
Significant correlations in humans between Strep, mutans counts in sahva and plaque with the prevalence and incidence of caries
Strep, mutans can often be isolated from the tooth surface before the development of caries
Correlation between the progression of carious lesions and Strep, mutanscounts Produces extracellular polysaccharide from sucrose which may help to ‘cement’ the plaque microflora together and to the tooth surface
Most effective streptococcus in experimental caries in animals (rodents and non-human primates)
Ability to initiate and maintain microbial growth and to continue acid production at low pH values
Rapid metabolism of sugars to lactic and other organic acids Can attain the critical pH for enamel demineralization more rapidly than other common plaque bacteria
Produces intracellular polysaccharide which may act as a food store for use when dietary carbohydrate is low
Immunization of animals with Strep, mutans significantly reduces the incidence of caries
It must be stressed that not all strains of Strep. mutans possess the complete range of properties described in Table 4.1. Therefore, strains of Strep. mutans will very likely vary in their potential to produce dental caries. It is possible that certain strains of Strep. mutans are more pathogenic than others and that, in a small number of individuals, caries may be an infectious disease, with a highly pathogenic strain being transmitted from one individual to another, e.g. during kissing. However, there is little evidence to support this hypothesis.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


