Bacterial infections
Publisher Summary
Specific bacterial infections of the mouth are uncommon, with tonsillitis in children caused by Strep. pyogenes being the most common. Other bacterial causes of pharyngitis that are rarely diagnosed include C. diphtheriae and the fusospirochaetal complex associated with Vincent’s angina. Specific infections of the oral mucosa that are rare, and are usually manifestations of systemic infections, include diseases such as tuberculosis, syphilis, and gonorrhea. Sore throat is a common symptom of a number of specific infections and is accompanied by a variable degree of constitutional upset. Gonorrhea is a venereal infection with a worldwide distribution that has reached epidemic proportions in some countries. Although, at present, syphilis is not encountered frequently, it is an important disease with a variety of oral manifestations. Human-type and bovine-type tuberculosis are caused in man by Mycobacterium tuberculosis and Mycobacterium bovis, respectively. Other opportunist mycobacteria might also cause human infections. Leprosy is caused by an acid-alcohol-fast bacillus, Mycobacterium leprae, which in general prefers to grow near the cooler body surfaces of man. Tetanus is caused by a strictly anaerobic spore-bearing Gram-positive bacillus, Clostridium tetani.
Tonsillitis and pharyngitis
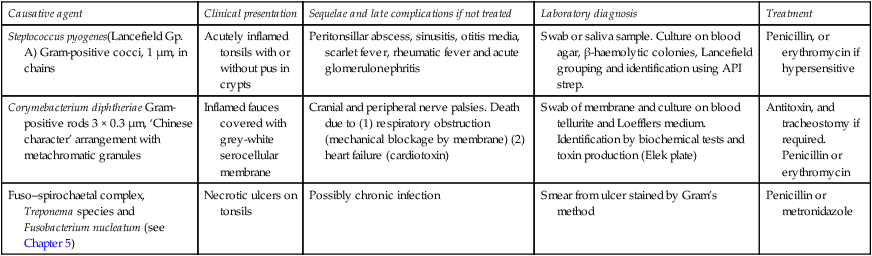
Sore throat is a common symptom of a number of specific infections and is accompanied by a variable degree of constitutional upset. Although a specific diagnosis may be assisted by the clinical presentation, it is often necessary to perform laboratory tests. At least two-thirds of these infections are caused by viruses, the remaining one-third by bacteria, almost all due in the developed countries to Strep. pyogenes. It is noteworthy that Strep. pyogenes may cause rheumatic fever and carditis in susceptible individuals. Consequently, they may be at a higher risk of contracting infective endocarditis due to bacteraemias associated with surgical procedures such as tooth extractions. A summary of the clinical presentation, causative agents and microbial diagnosis of tonsillitis/pharyngitis is shown in Table 8.1.
Table 8.1
Bacterial causes of tonsillitis – pharyngitis
| Causative agent | Clinical presentation | Sequelae and late complications if not treated | Laboratory diagnosis | Treatment |
| Steptococcus pyogenes(Lancefield Gp. A) Gram-positive cocci, 1 μm, in chains | Acutely inflamed tonsils with or without pus in crypts | Peritonsillar abscess, sinusitis, otitis media, scarlet fever, rheumatic fever and acute glomerulonephritis | Swab or saliva sample. Culture on blood agar, β-haemolytic colonies, Lancefield grouping and identification using API strep. | Penicillin, or erythromycin if hypersensitive |
| Corymebacterium diphtheriae Gram-positive rods 3 × 0.3 μm, ‘Chinese character’ arrangement with metachromatic granules | Inflamed fauces covered with grey-white serocellular membrane | Cranial and peripheral nerve palsies. Death due to (1) respiratory obstruction (mechanical blockage by membrane) (2) heart failure (cardiotoxin) | Swab of membrane and culture on blood tellurite and Loefflers medium. Identification by biochemical tests and toxin production (Elek plate) | Antitoxin, and tracheostomy if required. Penicillin or erythromycin |
| Fuso–spirochaetal complex, Treponema species and Fusobacterium nucleatum (see Chapter 5) | Necrotic ulcers on tonsils | Possibly chronic infection | Smear from ulcer stained by Gram’s method | Penicillin or metronidazole |
Syphilis
The course of syphilis when acquired after birth can be split into three main stages.
Oral manifestations
The normal site for the chancre is on the genitalia but extragenital primary lesions occur in some 10% of patients with syphilis. A chancre of the lip is the most common extragenital lesion and may present at the angles of the mouth. Other sites affected are the tongue and, to a lesser extent, the gingivae and tonsillar area (Table 8.2). Intraoral chancres are usually slightly painful due to secondary bacterial infection. The lesions are infectious and transmission may occur by kissing, unusual sexual practices and even by intermediate contact with cups, glasses and eating utensils. The chancre heals spontaneously about one to five weeks after appearing. The regional lymph nodes (submaxillary, submental and cervical) are enlarged. The differential diagnosis of primary syphilis includes ruptured vesicles of herpes simplex, traumatic ulcers and carcinoma.
Table 8.2
Oral manifestations and infectivity of syphilis
| Stage | Oral manifestations | Infectivity |
| Primary | Chancre of lip, tongue gingiva | + + + |
| Secondary | Mucous patches on tonsils, tongue, soft palate, cheek. ‘Snail track’ ulcers. Rubbery, enlarged cervical lymph nodes | + + |
| Tertiary | ‘Gumma’ of palate. Rarely osteomyelitis. Syphilitic leukoplakia leading to carcinoma | ± |
| Congenital | Hutchinson’s incisors. ‘Mulberry’ molars. Facial deformities with open bite or dish face | – |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


