Fig. 23.1
Emergency cards (Photo credit: Dr. Joshua Yanover)
-
Team Member 1
-
Call 911.
-
Stay on phone with dispatcher until told to hang up.
-
-
Doctor
-
Confirm emergency medical call was placed.
-
Place supplemental oxygen.
-
Confirm open airway.
-
Assess breathing.
-
Check pulse, blood pressure, and respirations.
-
Initiate basic life support if indicated.
-
Administer medications if indicated.
-
Provide pertinent information to paramedics.
-
-
Team Member 2
-
Get emergency kit.
-
Open emergency drug kit.
-
Draw up drugs as instructed by doctor.
-
-
Team Member 3
-
Obtain AED.
-
Place AED pads if instructed.
-
Assist Doctor.
-
-
Team Member 4
-
Record sequence of events: blood pressure and pulse; drugs administered including dose and time.
-
-
Team Member 5
-
Clear room and hallways for emergency medical services (EMS) personnel
-
Wait for EMS outside, near elevator, or at point of entry
-
Take EMS to emergency scene
-
23.1.2 Adult Cardiopulmonary Resuscitation (CPR) (AHA 2015)
In most states, training on CPR needs renewal on a biennial basis. Each member of the dental team should be trained to do CPR and use of the automated external defibrillator (AED) (Fig.23.2). There are online training courses that can be used as refreshers on a regular basis. In addition to formal training, mock drills in the office that simulate true emergencies would be a wise decision.
Fig. 23.2
(a, b) Use of the AED is essential when a patient is in cardiac arrest. Instructions for use are given by the voice commands that the AED is equipped with
In the Event of an Emergency
-
Make sure environment is safe for rescuers and victim.
-
Check responsiveness: no breathing or only gasping (no normal breathing), no definite pulse felt within 10 s.
-
Activate emergency response system: Send someone to get AED and begin CPR immediately; use the AED as soon as it is available.
-
Begin cycles of 30 compressions and 2 breaths at compression rate of 100–120/min; Compressions are approximately 2 in. or 5 cm in depth.
-
Regardless of the cause of the cardiac arrest, the 2015 guidelines stress the need for continuous compressions with 10 breaths/min.
-
Once AED arrives, turn it on, attach the pads; the AED will check if a shock is necessary and will direct you.
23.1.3 Child and Infant CPR (Infant to Puberty)
-
Compression-ventilation ratio 15:2
23.2 What Should Be in Every Office’s Emergency Kit? (Fig. 23.3)
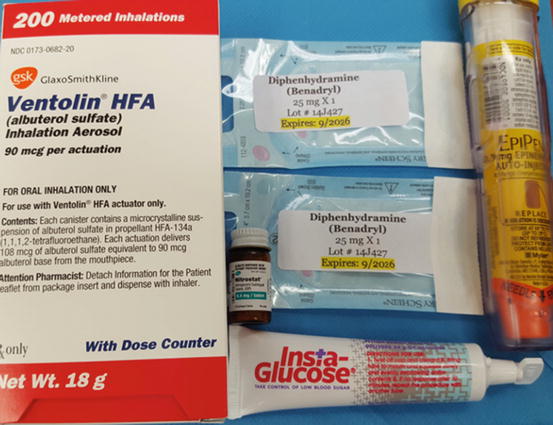
Fig. 23.3
The location of the emergency medications should be known to everyone who works at the dental practice. A designated person in the office should be in charge of checking these medications on a regular basis to insure that they are not expired
The emergency medications needed in a dental office are included in Table 23.1. Use of these medications should be reviewed on a regular basis. Familiarity with the patient’s medical history prior to treatment and making special arrangements are the best ways to avoid injury to the patient.
Table 23.1
Emergency medications for a dental office
|
Drug name
|
Category
|
Indications
|
Quantity/dose
|
Side effects
|
|---|---|---|---|---|
|
Injectable
|
||||
|
Epinephrine
|
Allergy, anaphylaxis
|
Acute allergic reaction, bronchospasm
|
Two (2) preloaded autoinjector syringes (EpiPen) of 1:1000 epinephrine (0.3 mg per dose) for patients weighing 30 kg (66 lbs) or greater
|
Tachydysrhythmias; decreases placental blood flow and may induce premature labor
|
|
Diphenhydramine/Benadryl
|
Allergy, histamine blocker
|
Delayed-onset allergic reactions only involving skin
|
Two (2) 1 mL ampules of diphenhydramine (50 mg/mL)
|
Central nervous system (CNS) depression, decreased blood pressure, thickening of bronchial secretions (not for use in acute asthmatic episodes)
|
|
Non-injectable
|
||||
|
Oxygen
|
Oxygen
|
Respiratory distress, O2 should be used during all medical emergencies
|
E cylinder with nasal cannula at 6 L
|
Not indicated in the treatment of hyperventilating patient but will not cause any adverse effects
|
|
Nitroglycerine
|
Vasodilator
|
Angina pectoris (chest pain)
|
Metered spray bottle (0.4 mg) or sublingual tablets
|
Headache, facial flushing, hypotension, severe hypotension in patients taking erectile dysfunction drugs
|
|
Albuterol
|
Bronchodilator, β2 agonist
|
Bronchospasm (acute asthmatic episodes), allergic reactions with bronchospasm component
|
1 metered-dose inhaler
|
Tachycardia, ventricular dysrhythmias
|
|
Glucose source
|
Antihypoglycemic
|
Hypoglycemia secondary to diabetes mellitus or fasting hypoglycemia in the conscious patient
|
Orange juice, non-diet soda, Gatorade, glucose gel, icing/frosting
|
Not for use in patients without active gag reflex or unable to drink without assistance
|
|
Aspirin
|
Platelet aggregation inhibitor
|
Suspected myocardial infarction (MI) or unstable angina
|
Powdered or chewable aspirin (325 mg)
|
Not indicated for patients with aspirin allergy, predisposition to major hemorrhage, recent bleeding peptic ulcer
|
23.3 What to Ask for in a Medical Consult
-
Medical condition or disease of concern including severity, stability, and how well the patient is controlled
-
Explanation of planned dental treatment and systemic consequences (avoid dental jargon)
-
Outline planned procedures
-
Invasiveness
-
Length of appointments
-
Surgical procedures
-
Anticipated blood loss
-
Possible complications
-
Anesthetic use – with or without epinephrine? Local or sedation?
-
Pre- and postop medications
-
-
Request patient’s most recent:
-
History and Physical (H and P)
-
Laboratory data
-
Current cardiovascular condition
-
Coagulation status
-
Status of chronic diseases
-
Use of bisphosphonates, receptor activator of nuclear factor-kB ligand (RANKL) inhibitors, etc.
-
Any other recommendations
-
-
Patient’s signature authorizing the release of information, dentist’s signature, dental office’s address, phone number, fax number, and email address
23.3.1 Surgical Risk Assessment
No one can “clear” a patient for surgery. Being “cleared” for surgery implies there is no risk. The provider should evaluate the risks and benefits of a procedure and discuss these with the patient prior to any procedure.
23.4 Most Common Medical Conditions and the Necessary Precautions
A thorough review of the patient’s medical history and a complete list of medications are necessary prior to dental treatment. These should all be noted in the patient chart. Medical consults where appropriate should be completed as well to insure safety of the patient. The following is meant as a guideline for the most common medical conditions that a patient may present with (Table 23.2).
|
The American Society of Anesthesiologists (ASA) classification
|
ASA I
|
Normal healthy patient
|
||
|
ASA II
|
Patient with mild systemic disease. No significant impact on daily activity; unlikely to have an impact on anesthesia and surgery (mild asthma, well-controlled hypertension (HTN))
|
|||
|
ASA III
|
Patient with significant or severe systemic disease that limits daily activity. Significant impact on daily activity; probable impact on anesthesia and surgery (hemodialysis, class 2 heart failure)
|
|||
|
ASA IV
|
Patient with severe systemic disease that is a constant threat to life or that requires intensive therapy. Serious limitation of daily activity; likely major impact on anesthesia and surgery (acute MI, respiratory failure requiring mechanical ventilation)
|
|||
|
ASA V
|
Moribund patient not expected to survive the next 24 h
|
|||
|
Stress reduction guidelines
|
Normal, healthy, anxious patient (ASA 1):
Recognize patient’s level of anxiety
Consider premedication the evening prior to the operation
Consider premedication immediately before appointment
Schedule morning appointments
Short appointments
Minimize patient’s wait time
Consider sedation during therapy
Administer adequate pain control during therapy
Follow up with postop pain and anxiety control
Telephone patient later the same day that treatment was delivered
Medical-risk patient (ASA 2, 3, 4):
Recognize patient’s degree of medical risk
Consider medical consultation before dental therapy
Schedule morning appointments
Short appointments
Monitor and record preop and postop vitals
Consider sedation during therapy
Administer adequate pain control during therapy
Follow up with postop pain and anxiety control
Telephone patient later the same day that treatment was delivered
|
|||
|
Cardiovascular disease
|
Limit dental care in patient with low metabolic equivalent
|
|||
|
Emergency dental care: benefit received by intervention outweighs the risk of cardiovascular complications: pain relief, treatment of infection, hemostasis
Stay updated, free dental videos. Join our Telegram channel
VIDEdental - Online dental courses
 Get VIDEdental app for watching clinical videos
Get VIDEdental app for watching clinical videos

| ||||