Maxillary protraction headgear has been used in the treatment of Class III malocclusion with maxillary deficiency. However, loss of dental anchorage has been reported with tooth-borne anchorage such as lingual arches and expansion devices. This side effect can be minimized with skeletal anchorage devices such as implants, onplants, mini-implants, and miniplates. The use of miniplates for maxillary protraction in the mixed dentition has not been reported in the literature. This case report describes the treatment of an 8-year-old girl with a Class III malocclusion and maxillary deficiency. Miniplates were used as skeletal anchorage for maxillary protraction followed by phase 2 orthodontic treatment with fixed appliances. Skeletal, dental, and facial changes in response to orthopedic and orthodontic treatment are reported to illustrate the esthetics, function, and stability of treatment with this new technique.
Maxillary protraction headgear has been used in the treatment of Class III patients with maxillary retrusion. Clinical studies have shown that 2 to 4 mm of maxillary advancement can be obtained with 8 to 12 months of maxillary protraction. This is the result of a combination of forward movement of the maxilla, downward and backward rotation of the mandible, labial tipping of the maxillary incisors, and lingual tipping of the mandibular incisors. Most of these studies used tooth-borne anchorage devices such as a lingual arch, quad helix, or maxillary expansion appliance. The disadvantages of tooth-borne anchorage devices are loss of anchorage, especially when preservation of arch length is necessary, and the inability to apply orthopedic force to the maxilla directly. Many investigators have attempted to design an absolute anchorage system for maxillary protraction including the use of intentionally ankylosed maxillary deciduous canines, osseointegrated titanium implants, onplants, miniscrews, and miniplates. Each implant system has strengths and weaknesses. Miniplates, for example, have been used with success for a variety of orthodontic anchorage needs including intrusion of posterior molars, correction of anterior open bite, retracting mandibular molars, and treatment of patients with maxillary hypoplasia. Surgical or titanium miniplates are gaining popularity as an orthodontic implant anchor because they have been proven safe and effective for fractures and osteotomies, and they can be placed above the tooth roots to facilitate orthodontic tooth movement. The use of miniplates in the treatment of maxillary hypoplasia in growing Class III patients has not been reported in the literature. This case report illustrates the use of surgical miniplates as anchorage for maxillary protraction in the mixed dentition.
Diagnosis and etiology
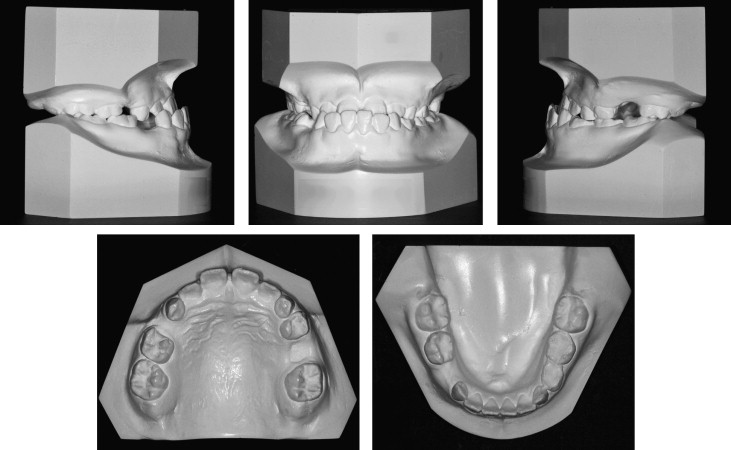
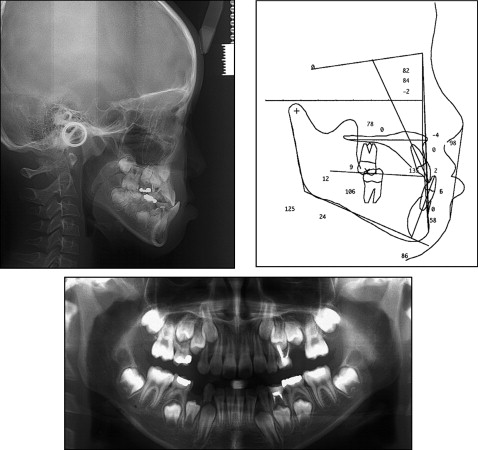
The patient, an 8-year-old girl, came to the Kangnung National University Orthodontic Clinic in Gangneung, South Korea, with a chief concern of “my bite is not right.” Clinically, she had a concave facial profile, and acute nasolabial angle, and a protrusive mandible ( Fig 1 ). Intraorally, she had an anterior crossbite and a low anterior tongue posture. The maxillary right first deciduous molar and left second deciduous molar had exfoliated prematurely, and midarch crowding was noted on the dental casts and panoramic radiograph. The cephalometric radiograph and tracing showed a skeletal Class III malocclusion with maxillary deficiency, mandibular prognathism (ANB, –2.2°), and a normal mandibular plane angle (FMA, 23°). The maxillary incisors were proclined (U1 to FH, 109°), and the mandibular incisors were retroclined (IMPA, 86°), compensating for the skeletal malocclusion ( Figs 2 and 3 , Table ). There was no family history of mandibular prognathism.

| Measurement | Pretreatment | After protraction headgear treatment | After fixed appliance treatment | 27 months after fixed appliance treatment |
|---|---|---|---|---|
| SNA (°) | 81.8 | 89.1 | 91.3 | 92.3 |
| SNB (°) | 84.0 | 82.4 | 87.4 | 89.4 |
| ANB (°) | −2.2 | 6.7 | 3.9 | 3.0 |
| SNO (°) | 63.0 | 70.0 | 67.0 | 70.0 |
| A to N⊥ FH (mm) | 0 | 8.1 | 7.7 | 9.1 |
| Angle of convexity (NAPog) (°) | −4.1 | 12.8 | 7.4 | 5.4 |
| Mandibular length (Co-Pog) (mm) | 106.5 | 113.1 | 120.1 | 122.7 |
| Midfacial length (Co-A) (mm) | 77.9 | 89.0 | 90.8 | 93.6 |
| MP-FH (°) | 24.0 | 25.3 | 22.4 | 19.4 |
| PP-FH (°) | 0.4 | −2.9 | 0.0 | −1.5 |
| U1-FH (°) | 109.8 | 109.0 | 118.4 | 122.8 |
| IMPA (°) | 86.1 | 92.5 | 93.3 | 92.6 |
| Nasolabial angle (°) | 97.6 | 105.2 | 92.7 | 97.8 |
| UL-RE line (mm) | −0.8 | 4.8 | 2.6 | 0.7 |
| LL-RE line (mm) | 5.4 | 5.5 | 6.9 | 5.5 |
Treatment objectives
In determining our treatment objectives, we asked the patient whether she was willing to undergo a surgical operation. She was willing if necessary. For that reason, our treatment consisted of phase 1 orthopedic treatment to protract the maxilla with a skeletal anchorage system. Surgical miniplates were used as anchorage instead of the conventional tooth-borne appliances to prevent possible mesial movement of the posterior dentition. The objective of this early phase of treatment was to induce harmonious growth of the maxilla with improvement in facial esthetics. Overcorrection of the maxilla to an overjet of 3 to 4 mm was desirable to anticipate excessive growth of the mandible during the pubertal growth spurt. The patient was followed for a period of time to determine whether the malocclusion could be camouflaged by orthodontic tooth movement. The phase 2 treatment was initiated at 11 years of age for 18 months to correct the remaining crowding, overjet, and overbite problems. The patient was placed in retention for 27 months after fixed appliance therapy to determine the stability of treatment without orthognathic surgery.
Treatment objectives
In determining our treatment objectives, we asked the patient whether she was willing to undergo a surgical operation. She was willing if necessary. For that reason, our treatment consisted of phase 1 orthopedic treatment to protract the maxilla with a skeletal anchorage system. Surgical miniplates were used as anchorage instead of the conventional tooth-borne appliances to prevent possible mesial movement of the posterior dentition. The objective of this early phase of treatment was to induce harmonious growth of the maxilla with improvement in facial esthetics. Overcorrection of the maxilla to an overjet of 3 to 4 mm was desirable to anticipate excessive growth of the mandible during the pubertal growth spurt. The patient was followed for a period of time to determine whether the malocclusion could be camouflaged by orthodontic tooth movement. The phase 2 treatment was initiated at 11 years of age for 18 months to correct the remaining crowding, overjet, and overbite problems. The patient was placed in retention for 27 months after fixed appliance therapy to determine the stability of treatment without orthognathic surgery.
Treatment alternatives
Based on the objectives, 2 treatment options were proposed. The first option was an early phase of orthopedic treatment to induce harmonious skeletal growth and improve facial esthetics followed by phase 2 treatment to correct the remaining crowding, overjet, and overbite problems. This option would not eliminate the necessity for orthognathic surgery. The patient would be followed to determine the stability of treatment. The second option would be to wait until all growth was completed and determine whether the malocclusion could be camouflaged by orthodontic treatment or a combination of surgical and orthodontic treatment.
Treatment progress
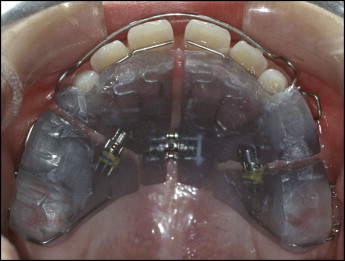
Phase 1 treatment was started at age 8 years 4 months with a maxillary removable appliance to regain space lost from the early loss of the deciduous molars ( Fig 4 ). After 6 months of observation, a surgical miniplate was placed. Local infiltration anesthesia was administered to the maxillary left and right buccal vestibular areas after surgical disinfection. A vestibular incision around the canine area was performed. After an atraumatic subperiosteal dissection to the infrazygomatic crest, a curvilinear miniplate was adapted, bent to the zygomatic buttress’s bony surface, and fixated with 3 self-tapping miniscrews per side ( Fig 5 , A ). From our experience, at least 3 to 4 screws should be placed to resist the maxillary protraction force of about 300 to 400 cN per side. Screw placement should be in a posterior-superior direction to prevent damage to the premolar tooth follicles ( Fig 5 , B ). The end of the miniplate entered the oral cavity between the canine and first premolar area in the keratinized attached gingiva to prevent gingival irritation. The oral portion of the miniplate was modified into a hook for elastic traction.

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


