Facial asymmetry is a typical finding in the majority of individuals. When present, it is most often located in the lower third of the face. Consequently, correction of dentofacial deformities frequently involves the management of asymmetry. This is important to note when planning for orthognathic surgery in that patients are able to appreciate correction of their asymmetry more so than the change in profile achieved with surgery. When evaluating mandibular asymmetry, deviation of the chin is more easily recognized than a discrepancy involving the angles of the mandible. Therefore, surgical correction may involve only genioplasty to correct chin position, with maintenance of asymmetry of the mandibular angles being acceptable.
Long-standing skeletal asymmetry can lead to dental compensation and soft tissue changes. Some degree of abnormality in each dimension will occur as a result of warping, bending, or distortion of both the hard and soft tissues. A three-dimensional (3D) perspective is required when evaluating facial asymmetry. The terms roll , pitch , and yaw have been used to describe rotation of the dental arches in patients with asymmetry. Roll is frontal cant of the occlusal plane, whereas pitch is the angle of occlusion in a sagittal dimension and yaw is rotation of the arch of the maxilla and mandible to the cranial base. The midlines may be on the central axis, but excessive yaw creates increased fullness on one side of the face with the converse appearing flat. The shift in arch form creates full tooth show to the commissure and a void in the opposite buccal corridor.
Earlier surgical intervention may be aimed at correcting the cause of the asymmetry to prevent continued exacerbation of the deformity. A stable asymmetric deformity allows definitive management of the malocclusion with conventional osteotomies. Although subtle asymmetries may be corrected by routine orthodontic preparation and orthognathic surgery, complex asymmetries involve detailed treatment planning, increased orthodontic effort, and more extensive surgery to achieve satisfactory functional and esthetic results.
Mandibular Asymmetry
Deficiencies
Deviation of the mandible can result from either deficiency or excess. In the case of mandibular deficiency, the mandible will deviate to the affected side secondary to decreased growth, degenerative changes, or trauma. Decreased growth often occurs as a result of a congenital or developmental anomaly. Hemifacial microsomia and Parry-Romberg syndrome are two such examples that are characterized by decreased hard and soft tissue growth resulting in asymmetry.
Acquired anomalies such as osteoarthritis and progressive rheumatoid arthritis may cause degeneration of the condyle and result in collapse of mandibular length through resorption of the condyle. Such remodeling creates loss of height with decreased projection of the remaining mandible. The loss of vertical dimension typically results in an open bite on the contralateral side as the dentition fulcrums on the affected side.
Trauma to the mandibular condyle is an acquired defect to consider when evaluating facial asymmetry. Fractures involving the condyle and neck can decrease ramus height and create deviation of the mandible. Return of sound functioning following injury to the condyle is the most important principle in acute management, whether it be by open or closed reduction. Failure to establish range of motion can lead to progressive degenerative changes or restricted growth in an immature individual since translation of the condyle is responsible for growth in the mandible. Limited movement of the condyle within the fossa will result in restricted growth and lead to progressive asymmetry of the mandible.
Excessive Growth
Mandibular asymmetry may also result from excess growth. Increased unilateral growth often causes deviation of the skeletal and dental midline away from the affected side. Unilateral prognathism results in deviation in a horizontal vector. This simple excessive growth creates a class III malocclusion of the canine and molar on the affected side. Unilateral condylar hyperplasia is classified as either hemimandibular elongation or hemimandibular hyperplasia.
Hemimandibular Elongation
Hemimandibular elongation is associated with lengthening of the condyle and ramus. The affected side of the mandible is longer than the normal side but is not associated with prognathism. The progressive changes produced by overgrowth of the condyle result in deviation of the chin. Enlargement of the condyle is not evident, and despite the elongation, the height of the face on the affected and unaffected sides is similar. Minimal distortion of the remaining mandible and overlying soft tissue occurs with hemimandibular elongation. A midline discrepancy is evident secondary to the excessive unilateral growth, and a crossbite relationship can develop on the contralateral side as the mandible deviates laterally. Subtle compensation of the arches can occur with the elongation, although the arch forms are generally well aligned.
The radiographic findings accompanying hemimandibular elongation can be subtle. The panoramic radiograph may illustrate dental and skeletal deviation with respect to the midline structures of the maxilla (nasal crest and septum). Elongation of the condyle and ramus may be identified in pronounced cases. Lateral cephalometric films will demonstrate superimposition of the dentition and inferior borders of the lower jaw as the elongation is expressed horizontally. The posteroanterior (PA) cephalometric image is the most diagnostic plain film for identification of hemimandibular elongation. The image provides skeletal assessment of the asymmetry since chin deviation, midline shift, and contrasting length of the mandibular rami are visualized.
Hemimandibular Hyperplasia
Hemimandibular hyperplasia is enlargement of one side of the mandible involving the condyle, neck, ramus, and body. A pronounced vertical discrepancy of the mandible is evident clinically as the increased growth creates downward bowing. The opposite half of the mandible is affected by the unilateral hyperplasia as the inferior border is rotated laterally and upward. The result is a distorted facial appearance created by increased length on the affected side with decreased height on the normal side ( Fig. 80-1 ). The skeletal asymmetry results in soft tissue distortion, with an oblique appearance created by the commissure of the lip similarly being displaced inferiorly.


The dentition is affected by the increased vertical growth of the mandible. An accentuated curve of Spee develops on the ipsilateral side as downward growth of the mandible drags the teeth inferiorly ( Fig. 80-2 ). The rapid vertical development typically creates an open bite because compensatory maxillary growth cannot keep pace. Development of the hyperplasia before puberty may allow the development of a canted occlusal plane if not controlled with a functional hybrid appliance. Hemimandibular hyperplasia is typically identified following the adolescent growth spurt as a result of continued growth of the affected mandible after growth on the opposite side has ceased.


Unilateral enlargement of the body, ramus, and condyle is seen radiographically on a panoramic film ( Fig. 80-3 ). A dramatic increase in bone volume is noted with hemimandibular hyperplasia. The appearance of the inferior border of the mandible is characteristic, with the affected side illustrating the downward bowing and the opposite side possessing a straighter slope running from the angle to the symphysis. The rounded angle is accentuated as the broad curvature extends from the ramus to the body. The body of the mandible opposite the hyperplasia possesses a flattened and thinned shape, as though it is being stretched by the overgrowth. The contrast between the enlarged, thickened, rounded hyperplastic half and the shortened, thinned, straight side exacerbates the warped contrast of the asymmetry.

A lateral cephalometric film will illustrate failure of the dentition and inferior borders of the mandible to superimpose as a single entity as a result of the vertical disparity ( Fig. 80-4 ). The increased vertical growth evident skeletally is typically greater than that appreciated in the occlusion. This information is valuable in guiding surgical treatment in that management of the occlusion by traditional mandibular ramus surgery will require additional correction via inferior border recontouring or augmentation efforts on the opposite side.

Diagnosis
The examination should detail the dentofacial deformity and the influence of asymmetry on the skeleton, dentition, and soft tissue. The changes directly associated with the asymmetry should be noted, in addition to effects that are the result of skeletal and dental compensation.
Imaging plays a valuable role in assessing skeletal asymmetry. Plain films, including a Panorex, lateral cephalogram, PA cephalogram, and submental vertex image, aid in characterizing the anatomic changes associated with the asymmetry and are valuable resources for planning treatment. Severe asymmetries may warrant additional imaging studies, including computed tomography (CT) and 3D reconstructions. The detailed imaging improves visualization of the condyle, where the source of the asymmetry typically arises.
Panoramic radiographs provide an opportunity to evaluate the condylar architecture and discrepancies within the ramus or body of the mandible. One must be aware, however, that distortion of the image may occur as a result of inappropriate positioning in the radiographic unit and create the impression of an enlarged mandible. Staff experience in obtaining routine panoramic films makes the likelihood of an artifact slim. An imaging artifact can be excluded if the size of the mandibular molars is comparable on the affected and unaffected sides.
The lateral cephalometric film is a mainstay in preparing for orthognathic surgery. Simple unilateral prognathism or hemimandibular elongation isolated to a horizontal plane is not readily identified on the lateral image, however. Vertical asymmetries are depicted as superimposition of distinct inferior borders and an occlusal plane discrepancy with multiple rows of teeth. The difference in the inferior borders is often greater than that noted in the occlusal plane, thus indicating the potential need for recontouring of the inferior border in addition to ramus surgery to correct the occlusion. Caution is also necessary to avoid radiographic artifact with the lateral cephalometric image. Clinicians should be mindful that individuals may have ear canals at varying heights creating the misperception of asymmetry. Finally, periodic interpretation of lateral cephalographic tracings will also aid in determining the timing of surgical intervention, whether it be related to documenting skeletal maturity or progressive change.
The PA cephalometric film will generally highlight the skeletal discrepancy in both its horizontal and vertical dimensions ( Fig. 80-5 ). The positioning of the mandibular dental midline against the opposing arch and the central skeletal axis of the mandible will be illustrated. Corresponding dental and skeletal midline asymmetry may allow surgical correction to be isolated to ramus osteotomies. The addition of an anterior segmental osteotomy of the inferior border to further correct chin positioning may be warranted if the imaging illustrates greater skeletal deviation than noted dentally. The PA cephalometric film allows interpretation of any dental compensation attributed to the asymmetry in the transverse plane, similar to incisor angulation on a lateral cephalometric image. The transverse orientation of the teeth as a result of natural and orthodontic efforts can be appreciated as the dentition attempts to keep up with the skeletal skewing.

The submental vertex image helps identify anatomic characteristics associated with the asymmetry. The bowing and warping of the mandible as a result of asymmetric growth can be visualized for both diagnostic and treatment considerations. The submental vertex film ( Fig. 80-6 ) aids in selection of osteotomy design for mandibular setback based on the shape of the ramus. A U-shaped mandible is best suited for a sagittal osteotomy, whereas a vertical ramus osteotomy is recommended with a divergent V-shaped ramus. A divergent ramus allows passive positioning of the condylar segment lateral to the mandible on a setback. Performance of sagittal osteotomy on a flared V-shaped mandible will create segment interference and lateral displacement of the proximal segments following mandibular repositioning.

CT provides extensive information on dentofacial deformities. The images provided in a CT scan help augment information gathered through examination and plain films. The ability to view an asymmetry in multiple dimensions helps in understanding the anatomic distortion that has occurred. The capacity to distinguish alterations in the architecture of the ramus and body of the mandible on both the affected and unaffected sides aids in identifying possible challenges that may exist intraoperatively. The improved visualization of the condyle helps one understand the cause of the mandibular asymmetry, such as excessive growth or condylar remodeling. In addition, imaging may reveal previously unidentified injuries to the condyle not readily discernible on plain films.
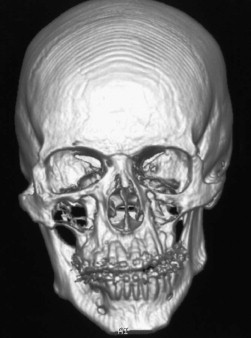
Reconstructed CT images provide perspective on the deformity and the influence that the asymmetry has on the skeletal and dental elements. 3D reconstructed images can illustrate the anatomic changes on the affected side and associated compensation ( Fig. 80-7 ). The visual representation provides an opportunity to demonstrate the deformity to the patient, as well as the necessary movements required to produce symmetry. Continuing advancements in radiology and CT afford the opportunity to develop treatment predictions and create templates for surgical guidance.
Stereolithographic models may be obtained from the reconstructed images to gain additional insight into the deformity. The model allows a reference for calculating the movements necessary to achieve symmetry. The decision to perform additional surgery consisting of resection or augmentation of the inferior border in the body or angle may be guided by the anatomic reproduction. The stereolithographic model can also be used for model surgery to assist in planning the need for additional skeletal correction of any bony asymmetry that may persist after addressing the malocclusion.
Diagnostic stone models of the dentition record the skeletal malocclusion that exists as a result of asymmetric mandibular growth. The variation in arch form and compensation within both the mandibular and maxillary arches can be assessed. Horizontal asymmetry of the mandible will result in lingual tipping of the dentition as the bone deviates laterally from the central axis. The maxillary arch will flare laterally to compensate for the skeletal change in the mandible. Progress models provide an indication of the orthodontic decompensation, as well as arch compatibility for correction of the malocclusion. Mounted diagnostic models are valuable when attempting to determine the status of the asymmetry. Progression of the asymmetry can be plotted through records of the occlusion. Persistent changes in the occlusion over an interval (12 to 18 months) indicate continued progression of the asymmetry, and surgery should be delayed until stability can be confirmed. An occlusal record with minimal change in an individual who has achieved skeletal maturity is probably an indication that surgical treatment may proceed.
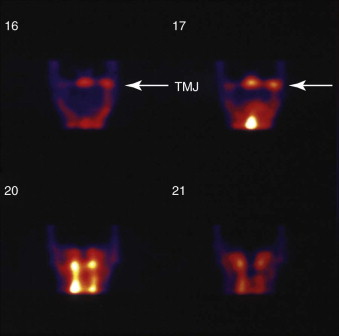
Imaging to evaluate progression of the asymmetry is accomplished through a nuclear medicine bone scan. A technetium-99m bone scan is frequently used to determine metabolic activity in the condyles ( Fig. 80-8 ). The bone scan is sensitive to increased activity but is not specific for degeneration or excessive growth. The imaging study serves as a guide for determining the status of the asymmetry for planning treatment. Increased uptake of the labeled marker on the affected side indicates activity and probably continued progression of the asymmetry. The presence of increased uptake may warrant delaying surgical correction until stability of the asymmetry can be documented. Activity on the scan with persistent worsening of the deformity may indicate that earlier surgical efforts are necessary to address the source of the excessive growth at the head of the condyle or to stabilize a degenerative process.
Diagnosis
The examination should detail the dentofacial deformity and the influence of asymmetry on the skeleton, dentition, and soft tissue. The changes directly associated with the asymmetry should be noted, in addition to effects that are the result of skeletal and dental compensation.
Imaging plays a valuable role in assessing skeletal asymmetry. Plain films, including a Panorex, lateral cephalogram, PA cephalogram, and submental vertex image, aid in characterizing the anatomic changes associated with the asymmetry and are valuable resources for planning treatment. Severe asymmetries may warrant additional imaging studies, including computed tomography (CT) and 3D reconstructions. The detailed imaging improves visualization of the condyle, where the source of the asymmetry typically arises.
Panoramic radiographs provide an opportunity to evaluate the condylar architecture and discrepancies within the ramus or body of the mandible. One must be aware, however, that distortion of the image may occur as a result of inappropriate positioning in the radiographic unit and create the impression of an enlarged mandible. Staff experience in obtaining routine panoramic films makes the likelihood of an artifact slim. An imaging artifact can be excluded if the size of the mandibular molars is comparable on the affected and unaffected sides.
The lateral cephalometric film is a mainstay in preparing for orthognathic surgery. Simple unilateral prognathism or hemimandibular elongation isolated to a horizontal plane is not readily identified on the lateral image, however. Vertical asymmetries are depicted as superimposition of distinct inferior borders and an occlusal plane discrepancy with multiple rows of teeth. The difference in the inferior borders is often greater than that noted in the occlusal plane, thus indicating the potential need for recontouring of the inferior border in addition to ramus surgery to correct the occlusion. Caution is also necessary to avoid radiographic artifact with the lateral cephalometric image. Clinicians should be mindful that individuals may have ear canals at varying heights creating the misperception of asymmetry. Finally, periodic interpretation of lateral cephalographic tracings will also aid in determining the timing of surgical intervention, whether it be related to documenting skeletal maturity or progressive change.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


