This article overviews the diagnosis and management of traumatic injuries to primary teeth. The child’s age, ability to cooperate for treatment, and the potential for collateral damage to developing permanent teeth can complicate the management of these injuries. The etiology of these injuries is reviewed including the disturbing role of child abuse. Serious medical complications including head injury, cervical spine injury, and tetanus are discussed. Diagnostic methods and the rationale for treatment of luxation injuries, crown, and crown/root fractures are included. Treatment priorities should include adequate pain control, safe management of the child’s behavior, and protection of the developing permanent teeth.
Dental injuries to preschool children can be challenging to manage because of the child’s and parents’ anxiety and the potential for damage to the developing permanent tooth buds. A conservative treatment approach that minimizes the potential emotional trauma to the child while prioritizing the healthy development of the permanent incisors is advised.
Etiology and epidemiology
Differences in study design and sampling criteria make it difficult to accurately determine the incidence and prevalence of traumatic injuries to the primary dentition. Reports indicate that 30% to 40% of preschool children suffer injuries to the primary dentition with the prevalence equal between boys and girls. This probably underestimates the actual occurrence of trauma as many apparently minor injuries go unreported.
The teeth most commonly injured are the maxillary central incisors. Predisposing factors include increased overjet and incompetent lip closure. Falls are the most common cause of injuries to young children particularly in the toddler stage as they develop mobility skills. A disturbing cause of oral injuries in children is child abuse. Up to 75% of all injures of abused children occur in the head and neck region. Signs of abuse include tears of labial frena, injuries in various stages of healing, and injuries whose clinical presentation is inconsistent with the history provided by the caregiver. Other signs include bruising of the labial sulcus in patients who are not walking, bruising of the soft tissues of the cheek or neck (accidental falls are more likely to bruise the forehead or chin), and human hand marks or pinch marks on the cheeks and ears.
Examination and diagnosis
History
A thorough medical and dental history is required to accurately diagnose the injured child’s condition. The potential severity of the injury is determined by knowing when, where, and how it occurred. The time elapsed since the injury affects the treatment and, most often, the prognosis. Knowledge of the mechanism of the injury helps determine its severity and the risk of associated injuries.
The child’s medications and drug allergies should be determined with particular attention paid to immunizations. Tetanus prophylaxis is significant when the child suffers wounds that are contaminated by dirt as can occur with avulsions, intrusions, or deep lacerations. Reports indicate that increasing numbers of children in the United States are not getting appropriate immunizations because their parents believe that vaccinations are harmful or because of their growing cost. Children can achieve immediate passive immunity to tetanus with an injection of tetanus toxoid and tetanus immune globulin so any question about the adequacy of a child’s tetanus protection should prompt a medical referral.
Severe head injury should also be ruled out. If there is a history of loss of consciousness, confusion, vomiting, headache, personality change, nausea, seizure or disorientation, patients should be referred for immediate neurologic evaluation.
Clinical Examination
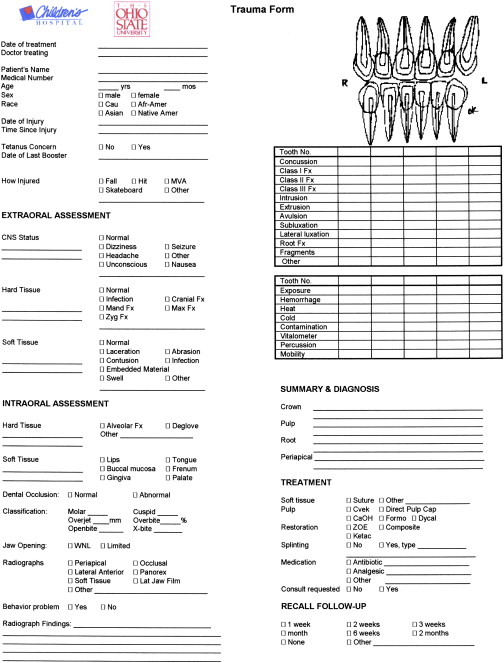
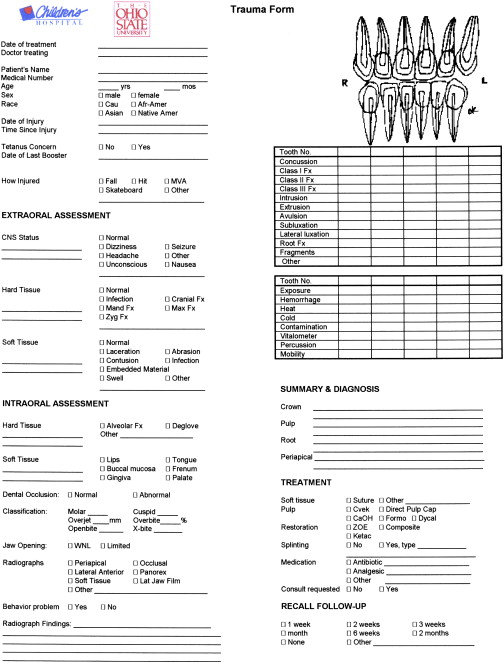
It is essential that the clinician conduct a comprehensive and thorough extraoral and intraoral examination. Many clinicians find it helpful to use a trauma assessment form to record data and to organize the management of care ( Fig. 1 ). An injured preschool child is frequently unable to cooperate and lay passively in a dental chair for the examination. In some cases a thorough examination can be obtained by using the knee-to-knee technique with the parent or an assistant ( Fig. 2 ). On rare occasions it may be necessary to use techniques of protective stabilization using a restraining device ( Fig. 3 ). Informed consent from the parent is required before protective stabilization is employed.


Extraoral examination
All extraoral injuries to the head and neck region, including bruises, contusions, swelling, and lacerations, should be recorded. Facial bone fractures can be detected by careful palpation to determine discontinuities. Mandibular function and range of motion in all excursive movements should be checked. Neck stiffness or pain can signal cervical spine injury and immediate medical referral is indicated.
Intraoral examination
A soft-tissue examination should be completed to rule out lacerations and perforations. Careful attention should be paid to the presence of foreign bodies embedded in lacerated tissues as lack of thorough debridement can cause chronic infection and scarring.
Each tooth should be checked for mobility, fracture, and dislocation. Gently percussing each tooth is an excellent way to detect periodontal ligament (PDL) inflammation, though a frightened child provides an exaggerated response to any stimulus. For this reason, vitality tests are not routinely performed on primary teeth.
Radiographic examination
Radiographs are critical to an accurate diagnosis of an injured tooth. Films taken soon after an injury detect acute changes, such as dislocations, root fractures, foreign bodies, alveolar fractures and, possibly, injuries to developing permanent teeth. Follow-up radiographs taken at 3 to 4 weeks postinjury can help detect inflammatory root resorption, apical osteitis and calcific changes in the pulpal lumen.
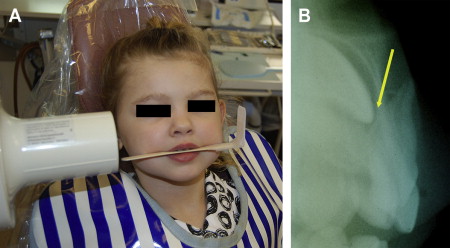
The standard occlusal view is a simple and reliable exposure to detect injuries to anterior primary teeth ( Fig. 4 ). In cases of multiple tooth injuries or suspected root fractures, additional occlusal views taken from slightly different horizontal angles can improve the accuracy of the diagnosis. A lateral anterior view can also be helpful to determine the relationship between an intruded primary incisor and its permanent successor, or to localize foreign bodies embedded in soft tissues ( Fig. 5 ). Exposure times will vary according to the radiographic equipment used but doubling the exposure time is usually adequate for the lateral anterior film. A reduction to one third of the normal exposure time may be necessary to secure an adequate soft-tissue film.

Examination and diagnosis
History
A thorough medical and dental history is required to accurately diagnose the injured child’s condition. The potential severity of the injury is determined by knowing when, where, and how it occurred. The time elapsed since the injury affects the treatment and, most often, the prognosis. Knowledge of the mechanism of the injury helps determine its severity and the risk of associated injuries.
The child’s medications and drug allergies should be determined with particular attention paid to immunizations. Tetanus prophylaxis is significant when the child suffers wounds that are contaminated by dirt as can occur with avulsions, intrusions, or deep lacerations. Reports indicate that increasing numbers of children in the United States are not getting appropriate immunizations because their parents believe that vaccinations are harmful or because of their growing cost. Children can achieve immediate passive immunity to tetanus with an injection of tetanus toxoid and tetanus immune globulin so any question about the adequacy of a child’s tetanus protection should prompt a medical referral.
Severe head injury should also be ruled out. If there is a history of loss of consciousness, confusion, vomiting, headache, personality change, nausea, seizure or disorientation, patients should be referred for immediate neurologic evaluation.
Clinical Examination
It is essential that the clinician conduct a comprehensive and thorough extraoral and intraoral examination. Many clinicians find it helpful to use a trauma assessment form to record data and to organize the management of care ( Fig. 1 ). An injured preschool child is frequently unable to cooperate and lay passively in a dental chair for the examination. In some cases a thorough examination can be obtained by using the knee-to-knee technique with the parent or an assistant ( Fig. 2 ). On rare occasions it may be necessary to use techniques of protective stabilization using a restraining device ( Fig. 3 ). Informed consent from the parent is required before protective stabilization is employed.


Extraoral examination
All extraoral injuries to the head and neck region, including bruises, contusions, swelling, and lacerations, should be recorded. Facial bone fractures can be detected by careful palpation to determine discontinuities. Mandibular function and range of motion in all excursive movements should be checked. Neck stiffness or pain can signal cervical spine injury and immediate medical referral is indicated.
Intraoral examination
A soft-tissue examination should be completed to rule out lacerations and perforations. Careful attention should be paid to the presence of foreign bodies embedded in lacerated tissues as lack of thorough debridement can cause chronic infection and scarring.
Each tooth should be checked for mobility, fracture, and dislocation. Gently percussing each tooth is an excellent way to detect periodontal ligament (PDL) inflammation, though a frightened child provides an exaggerated response to any stimulus. For this reason, vitality tests are not routinely performed on primary teeth.
Radiographic examination
Radiographs are critical to an accurate diagnosis of an injured tooth. Films taken soon after an injury detect acute changes, such as dislocations, root fractures, foreign bodies, alveolar fractures and, possibly, injuries to developing permanent teeth. Follow-up radiographs taken at 3 to 4 weeks postinjury can help detect inflammatory root resorption, apical osteitis and calcific changes in the pulpal lumen.
The standard occlusal view is a simple and reliable exposure to detect injuries to anterior primary teeth ( Fig. 4 ). In cases of multiple tooth injuries or suspected root fractures, additional occlusal views taken from slightly different horizontal angles can improve the accuracy of the diagnosis. A lateral anterior view can also be helpful to determine the relationship between an intruded primary incisor and its permanent successor, or to localize foreign bodies embedded in soft tissues ( Fig. 5 ). Exposure times will vary according to the radiographic equipment used but doubling the exposure time is usually adequate for the lateral anterior film. A reduction to one third of the normal exposure time may be necessary to secure an adequate soft-tissue film.





