Zygomatic fractures are common in facial trauma and, as is the case with other facial fractures, occur primarily among men in their third decade of life. These fractures occur most commonly as the result of assaults or motor vehicle collisions.
Displaced fractures of the zygoma cause obvious deformities of the midface related to the projection of the malar eminence, lateral projection of the arch, and position of the globe, which can affect vision. For these reasons, the appropriate diagnosis and treatment of these fractures are important for the functional and cosmetic outcome of facial trauma patients.
ANATOMY
Because of its prominent position on the facial skeleton, the zygomatic bone is responsible for the anterior and lateral projection of the midface and thus is a very important part of facial aesthetics. Its outer (lateral) surface is convex; its inner (temporal) surface, concave. It is quadrilateral in shape and articulates with four other bones: maxilla, sphenoid, temporal, and frontal bones. Because it forms part of the lateral wall and floor of the orbit, fractures of the body of the zygoma usually involve fractures of the floor or the lateral wall of the orbit, or both ( Figure 12-1 ).
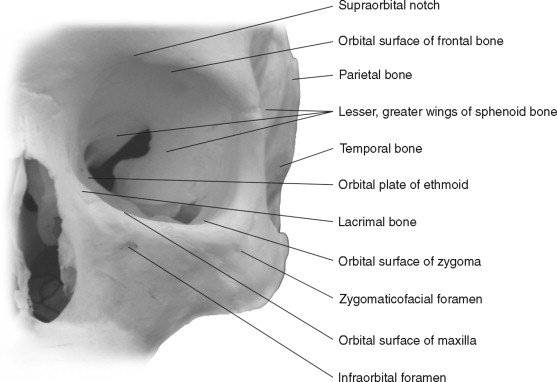
The four processes of the zygoma are the frontal, maxillary, temporal, and sphenoid. The frontal process is sturdy; however, it narrows superiorly as it articulates with the zygomatic process of the frontal bone. It forms a large portion of the orbit and, together with the sphenoid bone, forms part of the orbital floor. The temporal process is narrow and thin. It articulates with the zygomatic process of the temporal bone, and together they make up the zygomatic arch. The body of the zygoma is sturdy, but its articulations are frequently the site of fracture.
Five muscles attach to the zygoma: the masseter muscle originates from its temporal surface; the zygomaticus major, the zygomaticus minor, and the levator labii superioris originate from its malar surface. The temporalis muscle and the temporalis fascia attach at the temporal process, specifically its posterolateral edge.
Two foramina arise from this bone. On the malar surface is the zygomaticofacial foramen, which provides exit to the nerve and vessels of the same name. The zygomaticotemporal foramen on its medial side transmits the zygomaticotemporal nerve and vessels.
From a frontal view, the ideal position of the zygomatic prominence is 10 mm lateral and 20 mm inferior to the lateral canthus. From a lateral perspective, the globe should be 1 mm anterior to the most prominent portion of the zygoma. Because these ideal measurements are not always found, an examination of the contralateral zygoma will determine the correct position of the injured zygoma in every patient who has no craniofacial anomalies.
For complex zygomatic fractures, multiple approaches are often needed for visualizing the fracture sites and applying internal fixation. The anatomy of the eyelids and scalp is briefly discussed here for later reference.
The upper eyelid consists of five distinct layers from skin to conjunctiva: the skin, the orbicularis oculi muscle, the orbital septum above or the levator palpebrae superioris aponeurosis below, the Müller muscle/tarsus complex, and the conjunctiva. The lower eyelid consists of at least four distinct layers: the skin and subcutaneous tissue, the orbicularis oculi muscle, the tarsus (upper 4 to 5 mm of the eyelid) or orbital septum, and the conjunctiva.
The layers of the scalp can be remembered with the simple mnemonic SCALP: S = skin, C = subcutaneous tissue, A = muscularis aponeurotica, L = loose areolar connective tissue (subgaleal fascia or subaponeurotic plane), and P = pericranium (periosteum). The skin and subcutaneous tissue of the scalp are surgically inseparable, unlike these same structures elsewhere in the body. The musculoaponeurotic layer consists of the paired frontalis (epicranius) and occipitalis muscles, the auricular muscles, and a broad aponeurosis. The aponeurosis is the true galea and has two portions, an extensive intermediate aponeurosis between the frontalis and occipitalis muscles and a lateral extension into the temporoparietal region known as the temporoparietal fascia. The superficial temporal artery lies on or in this layer.
The subgaleal fascia is usually referred to as the loose areolar layer or the subaponeurotic plane. This layer cleaves readily, allowing the skin, subcutaneous tissue, and musculoaponeurotic layers to be stripped from the pericranium. The loose tissue of the subgaleal fascia allows free movement of the skin over the periosteum when the frontalis muscle is contracted. This fascial layer is used only for its ease of cleavage. Anteriorly the subgaleal fascia is continuous with the loose areolar layer deep to the orbicularis oculi muscles. Laterally the subgaleal fascia is attached to the frontal process of the zygoma and continues along the superior surface of the zygomatic arch, above the external auditory meatus, and over the mastoid process. The subgaleal fascia terminates as it fuses with the periosteum along the superior nuchal line. The pericranium is the periosteum of the skull and can be elevated from the skull, although it is more firmly attached along cranial sutures.
HISTORY AND PHYSICAL EXAMINATION
The patient’s medical history is always important, because many of these injuries will require operative intervention. As is often the case, medical and surgical problems may need to be managed in concert. The patient’s mechanism of injury most often provides the initial indications of a possible zygomatic fracture. Indications for surgery are cosmetic deformities and functional deficits ( Box 12-1 ).
-
Depressed arch
-
Depressed malar eminence
-
Diplopia
-
Enophthalmos
-
Paresthesia in V2 distribution
-
Trismus
Because of the prominent position of the zygoma on the face, zygomatic fractures can result in cosmetic deformities because of flattening of the malar eminence, widening or depression of the arch, orbital dystopia, or enophthalmos. These deformities can occur without severe impairment of function. However, fractures of the zygomatic arch can cause functional impairment by impinging on the temporalis muscle or obstructing the path of the coronoid and causing trismus. Zygomatic fractures impinging on the infraorbital nerve cause paresthesia or dysesthesia of the second division of the trigeminal nerve (V2). Disruption of the position of the globe can cause diplopia. Therefore an examination of the orbit and the globe—including assessment of extraocular movements, evaluation of the maxillary sinus, determination of V2 sensation, and examination of the range of motion of the mandible—is essential in diagnosing zygomatic injuries ( Figure 12-2 ).

Signs of zygomatic fracture are periorbital or maxillary vestibular ecchymosis, periorbital edema, flattened arch or malar prominence, deformity or displacement, trismus, displacement of palpebral fissure, enophthalmos, exophthalmos, chemosis, and conjunctival hemorrhage ( Figures 12-2 and 12-3 ). Symptoms that indicate zygomatic injury are pain, sensory deficit, crepitus from air emphysema, and diplopia.

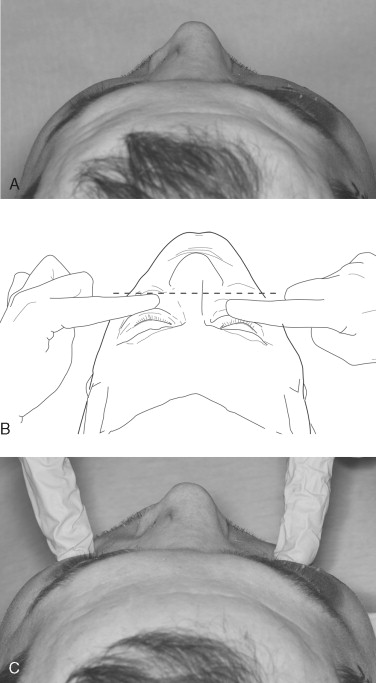
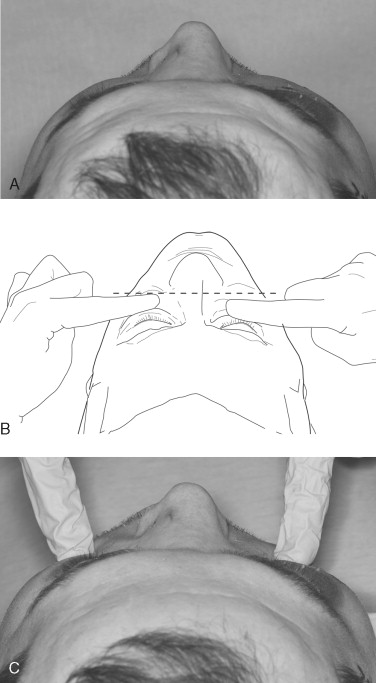
Once the examination of the patient has been completed, the anatomic dislocation of the zygoma can best be evaluated by digital exploration. The patient should be in the cephalad position during the examination; the surgeon should compare the right and left sides simultaneously, beginning at the zygomaticofrontal suture and palpating inferiorly and medially along the infraorbital rim. Then the zygomatic arch should be evaluated for dislocation, comminution, or pain. The buccal vestibule and antral wall should be palpated intraorally for detection of crepitus or bony disruption. Palpation is important because acute swelling after an injury can mask the displaced fracture ( Figure 12-4 ).
Many surgeons consider an ophthalmologic examination an essential part of the examination for zygomatic fracture. Depending on the mechanism of injury, as many as 28% of patients with zygomatic injuries may have moderate to severe ocular injuries.
HISTORY AND PHYSICAL EXAMINATION
The patient’s medical history is always important, because many of these injuries will require operative intervention. As is often the case, medical and surgical problems may need to be managed in concert. The patient’s mechanism of injury most often provides the initial indications of a possible zygomatic fracture. Indications for surgery are cosmetic deformities and functional deficits ( Box 12-1 ).
-
Depressed arch
-
Depressed malar eminence
-
Diplopia
-
Enophthalmos
-
Paresthesia in V2 distribution
-
Trismus
Because of the prominent position of the zygoma on the face, zygomatic fractures can result in cosmetic deformities because of flattening of the malar eminence, widening or depression of the arch, orbital dystopia, or enophthalmos. These deformities can occur without severe impairment of function. However, fractures of the zygomatic arch can cause functional impairment by impinging on the temporalis muscle or obstructing the path of the coronoid and causing trismus. Zygomatic fractures impinging on the infraorbital nerve cause paresthesia or dysesthesia of the second division of the trigeminal nerve (V2). Disruption of the position of the globe can cause diplopia. Therefore an examination of the orbit and the globe—including assessment of extraocular movements, evaluation of the maxillary sinus, determination of V2 sensation, and examination of the range of motion of the mandible—is essential in diagnosing zygomatic injuries ( Figure 12-2 ).

Signs of zygomatic fracture are periorbital or maxillary vestibular ecchymosis, periorbital edema, flattened arch or malar prominence, deformity or displacement, trismus, displacement of palpebral fissure, enophthalmos, exophthalmos, chemosis, and conjunctival hemorrhage ( Figures 12-2 and 12-3 ). Symptoms that indicate zygomatic injury are pain, sensory deficit, crepitus from air emphysema, and diplopia.

Once the examination of the patient has been completed, the anatomic dislocation of the zygoma can best be evaluated by digital exploration. The patient should be in the cephalad position during the examination; the surgeon should compare the right and left sides simultaneously, beginning at the zygomaticofrontal suture and palpating inferiorly and medially along the infraorbital rim. Then the zygomatic arch should be evaluated for dislocation, comminution, or pain. The buccal vestibule and antral wall should be palpated intraorally for detection of crepitus or bony disruption. Palpation is important because acute swelling after an injury can mask the displaced fracture ( Figure 12-4 ).
Many surgeons consider an ophthalmologic examination an essential part of the examination for zygomatic fracture. Depending on the mechanism of injury, as many as 28% of patients with zygomatic injuries may have moderate to severe ocular injuries.
INDICATIONS FOR RADIOGRAPHS AND SURGERY
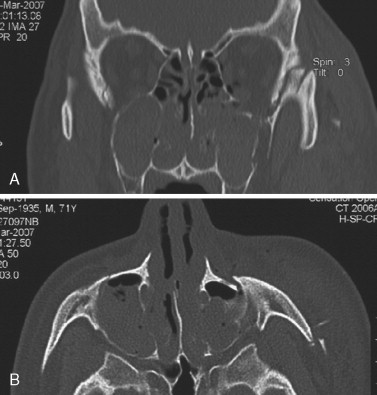
After the primary and secondary trauma survey, when life-threatening injuries have been ruled out or managed, radiographic imaging should be considered. Currently, computed tomography (CT) is the gold standard for diagnosing bony injuries of the face. Images (either direct or reformatted) should be obtained in the axial and coronal dimensions ( Figure 12-5 ).
In the unlikely event that obtaining CT scans is impossible, plain radiography can be used: the images that should be obtained are a lateral skull view, a Waters’ (posteroanterior oblique) or a reverse Waters’ (anteroposterior oblique) view, and a submental vertex view of the skull. The Waters’ or posteroanterior view provides visualization of the inferior or lateral rims, or both, and of the floor of the orbits, as well as the maxillary sinuses. Often the zygomatic arch can also be visualized. If patients cannot be placed in a supine or upright position, the modified or reverse Waters’ view (anteroposterior oblique) may be used. With this technique the structures are farther from the film; thus the structures are not as well-defined as in the classic Waters’ view. The lateral skull view provides detail about the paranasal sinuses and the presence of air intracranially.
CT scanning provides finely detailed views of the bony architecture and pinpoints even the smallest fractures. Because CT scanning uses less radiation and provides views more rapidly than plain radiography, it is now the procedure of choice. The best evaluation of suspected zygomatic and orbital fractures is provided by 1.5-mm slices in the axial plane (for information about the medial and lateral walls) and the coronal plane (for specific information about the orbital floor). Many scanners provide reconstructed coronal images, which are usually adequate with axial slices of 1.5 mm or less. Sagittal images provide useful information about the posterior extent of a floor defect and the amount of posterior bone that remains. Sagittal scans are not routinely performed and must be specifically requested. Three-dimensional reconstructions can be created and are often useful for diagnosing and planning the treatment of complex fractures.
CT scanning also provides information about soft tissues. It can visualize orbital injuries such as a ruptured globe, a dislocated lens, and a vitreous hemorrhage and can demonstrate a retrobulbar hemorrhage or a disruption of the optic nerve. The extraocular muscles are clearly visible, and the clinical assessment of entrapped muscles can be confirmed. Preseptal and postseptal hematomas can also be differentiated.
TREATMENT
During the consideration of treatment for zygomatic injuries, the patient’s interests should be paramount. The patient’s age and medical history should be factored into the decision-making process. If, after being informed about the risks and benefits of surgery or observation, the patient elects for surgery, the decision about how to treat and when to treat can be addressed.
Fracture patterns are classified by anatomic location and by the pattern of segmentation and displacement seen on CT scans. Fractures can be described as high-energy or low-energy injuries. A low-energy fracture typically results in mild to moderate displacement and is not comminuted. High-energy fractures often result in more severe displacement and comminution of the body of the zygoma. These injuries commonly require orbital reconstruction.
The main reason not to treat zygomatic fractures surgically is the clinical absence of functional and aesthetic compromise. Another consideration is the degree of vision in the unaffected eye. Visceral and neurologic damage always takes precedence over a fractured facial bone. Although the risk to vision associated with the repair of a zygomatic fracture is low (<1%), it may be unwise to risk affecting the sight in the remaining functional eye.
Once the decision has been made to proceed with surgical treatment, the surgeon must address the decision of when to operate. Waiting for residual edema to resolve, approximately 2 weeks, is usually acceptable. This delay allows time for adequately assessing and planning the case; in addition, findings associated with the injury manifest themselves during this time. Waiting longer than 2 weeks may complicate the surgical reduction of the fracture because early bone healing may begin during this time and may make osteotomy of the fracture site necessary. If soft tissue lacerations are present over the fracture sites, soft tissue fibrosis and contracture can make the soft tissue envelope more difficult to expand. Evidence of muscle entrapment on CT scan or on physical exam is an indication for immediate surgery. Pressure on the muscle from bone margins can lead to muscle necrosis and fibrosis, causing a permanent restriction of movement.
SURGICAL APPROACHES FOR FRACTURES OF THE ZYGOMATIC COMPLEX
The technique used to approach the facial skeleton depends on the individual fracture pattern and on the displacement of the fracture. For high-energy, comminuted fractures, or for multiple facial fractures, multiple approaches are necessary. For isolated zygomatic fractures, stable reduction can sometimes be achieved with less exposure. The order of the following approaches is based on the order in which they might be used for reducing an isolated, noncomminuted fracture of the zygoma.
CARROLL-GIRARD SCREW
The most direct approach in reducing a zygomatic fracture is to insert a Carroll-Girard screw. This is a T-shaped device that has a handle at one end with a sharp screw portion perpendicular to it. This device must be placed into the body of the zygoma, thus requiring an incision directly over the malar prominence. This requirement is the main drawback of this approach; however, if the incision is performed properly, the scar is virtually invisible within 6 months. Alternatively, if an infraorbital incision is used as an approach to the orbital rim, the screw can be placed through it. This screw is a very useful device and provides traction in any direction. Some surgeons recommend placing this screw regardless of any other methods of reduction used ( Figure 12-6 ).

VESTIBULAR APPROACH
This technique can be used for a wide variety of midfacial procedures. It allows safe access to the entire facial surface of the midfacial skeleton, from the zygomatic arch to the infraorbital rim and the frontal process of the maxilla. With regard to zygomatic injuries specifically, this approach is required for visualization of the zygomaticomaxillary buttress. The greatest advantage of this approach is that the scar can be hidden. This rapid and simple approach is associated with few complications.
The path to the underlying facial skeleton is through mucosa, submucosa, facial muscles, and periosteum. The only important neurovascular structure encountered during this dissection is the infraorbital nerve, which is located approximately 7 to 10 mm inferior to the infraorbital rim and just medial to the zygomaticomaxillary suture.
After submucosal injection of a vasoconstrictor, the incision is placed approximately 3 to 5 mm superior to the mucogingival junction. This placement leaves a cuff of unattached mucosa at the inferior extent that must be closed at the end of the procedure. The incision extends as far posteriorly as is necessary for exposure, usually up to the first molar tooth. Extension of the incision past the midline depends on whether the fractures are bilateral. The initial incision is perpendicular to the mucosa and then is angled perpendicular to the bone. The incision is carried through the periosteum, and a subperiosteal dissection is performed first anteriorly, then along the piriform aperture, and then posteriorly behind the zygomaticomaxillary buttress. Careful dissection at the buttress is advised so that the buccal fat pad is not exposed; such exposure is more of a nuisance than a complication of surgery.
The unilateral maxillary vestibular incision is closed simply in one layer with a 3-0 resorbable suture. If a circumferential maxillary vestibular incision is made, the closure is more complex. An alar cinch with V-Y closure is performed, and the midline is then tacked; this technique creates a linear incision. The vestibule is then closed in a continuous fashion to the midline from both sides.
APPROACHES TO THE ZYGOMATICOFRONTAL REGION
When the fracture remains unreduced or unstable after a closed reduction and a vestibular approach have been attempted, the surgeon might then address the zygomaticofrontal region. It is not uncommon to find significant overlap of bone, with the inferior lateral orbital rim having been displaced medially and superiorly.
LATERAL CANTHOTOMY
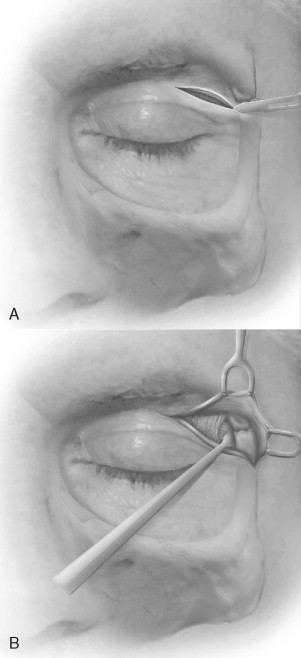
If a lateral canthotomy is indicated (because exposure of the zygomaticofrontal suture is necessary), this is the initial incision. The initial incision is made with a No. 15 blade through the skin and dermis and proceeds for only approximately 1 cm. An anesthetic with a vasoconstrictor should then be administered under the conjunctiva and in the lateral canthotomy site as an aid to hemostasis. Administering the anesthetic after this incision helps avoid distortion of the tissue as the procedure progresses. The incision is completed with pointed scissors to the depth of the lateral orbital rim (7 to 10 mm). The layers that are incised are skin, orbicularis oculi muscle, orbital septum, lateral canthal tendon, and conjunctiva. Mobilizing the lower eyelid may require releasing the anterior limb of the lateral canthal tendon. Subperiosteal dissection is then continued on the lateral surface of the superior lateral orbital rim and is followed by reduction and placement of fixation.
UPPER EYELID APPROACH
The upper eyelid approach can also be used to access the lateral orbital rim, the lateral orbital wall, and the superior orbital rim. This approach is also known as the upper blepharoplasty, upper eyelid crease, and supratarsal fold approach. A natural skin crease in the upper eyelid excellently camouflages the scar. If there is no eyelid skin crease, a curvilinear incision should be along the supratarsal fold and should tail off laterally over the lateral orbital rim. Protection of the cornea is critical during surgery and can be achieved with a tarsorrhaphy or a corneal shield placed at the beginning of the procedure. When the location of the incision has been determined, the incision is made through the skin only. After the initial incision, a local anesthetic with vasoconstrictor should be administered. Making the initial skin incision before administering the anesthetic is beneficial because distortion of the tissues after infiltration can make correct placement of the incision difficult. The incision should be placed at least 10 mm superior to the upper eyelid margin and 6 mm above the lateral canthus as it extends laterally ( Figure 12-7, A,B ).
The incision is made through the skin and the orbicularis oculi muscle. The vasculature of the muscle maintains the viability of the skin; elevating this vasculature with the skin creates a skin-muscle flap. This flap can be developed laterally, superiorly, and, if necessary, medially. Dissection continues superiorly just below the muscle and superficial to the orbital septum. Once the periosteum has been identified over the superior orbital rim, it is incised, and the periosteum is dissected up for exposure of the fracture. Care should be taken near the superior-lateral orbital rim, because the lacrimal fossa and gland are located just inside the rim.
After the fracture has been fixated, closure is performed in layers: periosteum, muscle, and skin.
EYEBROW APPROACH
This approach to the lateral orbital rim is straightforward and rapid and offers a relatively well-camouflaged scar. No important neurovascular structures are encountered during this approach. If the patient has undergone cosmetic eyebrow removal, or if exposure of the inferior lateral orbital rim is also necessary, the scars may be more apparent, and the extent of exposure may be limited.
This approach is rarely indicated; when it is, the eyebrow is not shaved. An incision of approximately 2 cm is made; the inferior extent of the incision should stop at the end of the eyebrow and parallel to the hair of the eyebrow so that no hair shafts are cut. The incision should not be extended inferiorly along the orbital rim, because such an extension may cross the lines of resting skin tension ( Figure 12-8 ).
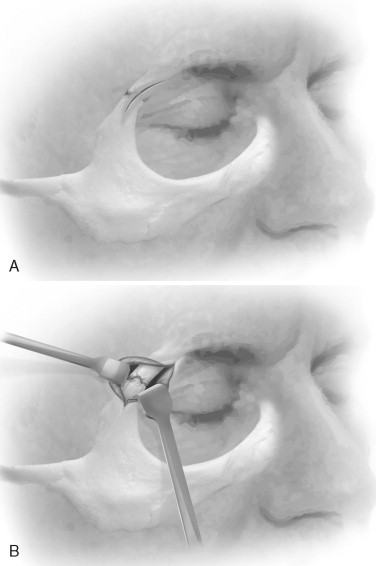
Once undermining has been performed in a supraperiosteal plane, the skin is retracted over the area of interest and a periosteal incision is made. Dissection is performed in a subperiosteal plane, but, again, access is limited. Closure is performed in a layered fashion.
APPROACHES TO THE INFRAORBITAL RIM AND THE ORBITAL FLOOR
LOWER EYELID APPROACHES
Lower eyelid approaches provide excellent exposure of the inferior orbital rim, the floor of the orbit, the lateral orbit, and the inferior portion of the medial orbital rim and wall. Placing the incision in the thin skin of the eyelid and in the natural resting lines of the skin results in a scar that becomes inconspicuous with time; transconjunctival incisions are perhaps the best hidden. Several external incisions exist and are named according to the inferior or superior position at which they are placed on the skin and also according to the level at which the muscle is transected for exposure of the periosteum. The subciliary incision, also known as the infraciliary or blepharoplasty incision, is made just below the eyelashes. The subtarsal approach, also known as the mid eyelid or skin crease approach, is made 4 to 7 mm below the eyelid margin ( Figure 12-9 ).

TRANSCONJUNCTIVAL APPROACH
The transconjunctival approach can be used to expose the infraorbital rim and the floor of the orbit. However, when a lateral canthotomy is used in conjunction with this approach, exposure of the zygomaticofrontal suture and the lateral wall of the orbit can be obtained. Also with medial extension of the transconjunctival incision posterior to the caruncle (i.e., transcaruncular incision), the medial wall of the orbit can be exposed. Some authors separate the transconjunctival approach from the transconjunctival approach with medial extension (i.e., transcaruncular approach) and from the transconjunctival approach with lateral canthotomy extension. In this chapter, all of these will be described under the transconjunctival approach.
The main advantage of this approach is that the scar is hidden; if a lateral canthotomy is used, an inconspicuous scar remains, usually in a skin crease. This approach is also rapid because it is not necessary to create a skin or a skin-muscle flap during dissection. With improper technique, the main disadvantage of this approach is entropion, which is more difficult to correct than the sequela of an improper skin incision (i.e., ectropion).
As is necessary with the previously described techniques, a forced duction test should be performed preoperatively and a corneal shield should be placed for protection. Two or three traction sutures, using 3-0 silk, can be placed into the lower eyelid approximately 5 mm inferior to the lid margin so that the tarsal plate is included in the suture.
The transconjunctival approach is begun by creating a small incision in the lateral conjunctiva with tenotomy scissors or with an electrocautery device. A subconjunctival plane is then bluntly dissected with the scissors, followed by completion of the conjunctival incision. This plane is easily found when this approach is combined with a lateral canthotomy. The incision is placed halfway between the inferior conjunctival fornix and the inferior margin of the tarsal plate. This incision can be placed as far medially as necessary as long as the lacrimal sac is not violated. This medial extension is called a transcaruncular incision because it was originally described as a 12- to 15-mm vertical incision through the conjunctiva and the lateral third of the caruncle. However, the incision can also be placed temporal to the caruncle. Either incision is carried superiorly through the conjunctiva to the level of the levator palpebrae aponeurosis, thereby exposing the underlying periorbita. Placing traction sutures in the vestibular conjunctiva can help hold the corneal shield in place and also help preserve the conjunctiva for closure at the end of the case ( Figure 12-10 ).
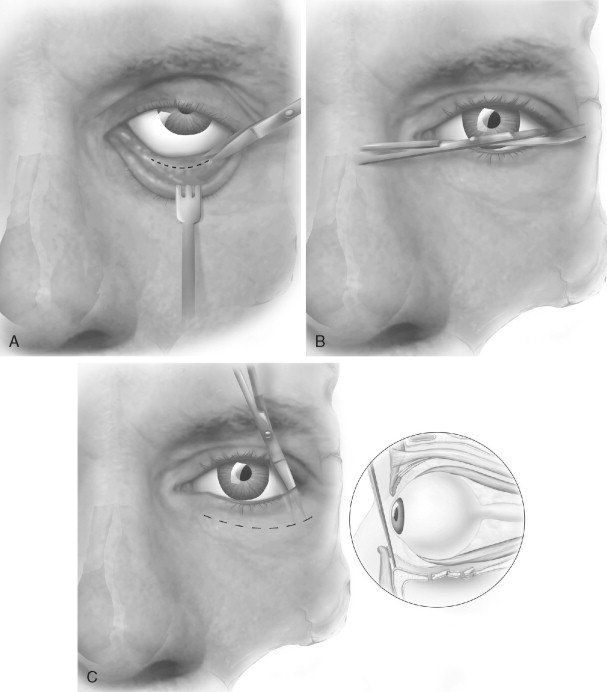
After the incision has been made through the conjunctiva, the surgeon must decide whether to perform a preseptal or a retroseptal approach to the orbital rim. The advantages of the retroseptal approach are that it is more direct and may help avoid the scarring within the lower eyelid that is associated with the preseptal approach. However, with the retroseptal approach, periorbital fat will be encountered. Other than being bothersome throughout the case, no serious risk is associated with exposing this adipose tissue. With the retroseptal approach, the surgeon sharply incises the periorbita immediately posterior to the orbital rim, paying special attention to avoiding the lacrimal sac medially. This incision can be made with electrocautery or with a No. 15 blade. If a preseptal approach is used, blunt tenotomy scissors are used after the incision through the conjunctiva for dissection through the septum and the inferior lid retractor muscles. The dissection is continued anterior to the septum to the lower rim approximately 2 mm inferior to the superior border of the infraorbital rim. The periosteum is then incised sharply.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


