Transmigrated mandibular canines increase the treatment complexity in terms of both anchorage and biomechanical planning. Additionally, a Class II malocclusion with a deep overbite and associated dental anomalies such as hypodontia can further increase the treatment complexity and the overall treatment time. This case report describes the successful interdisciplinary treatment of a patient, aged 12.5 years, with transmigrated and severely impacted mandibular canines and congenitally missing mandibular second premolars. The transmigrated mandibular right canine was extracted, and a maxillary second premolar was autotransplanted to the missing mandibular right second premolar site with the aid of a stereolithographic donor tooth replica fabricated with 3-dimensional cone-beam computed tomography and a rapid prototyping technique. Furthermore, the autotransplanted tooth was protracted by 4 to 5 mm to close the space caused by the extraction of the mandibular right canine. The impacted mandibular left canine was orthodontically guided into its normal position in the arch. Good esthetic outcome and functional occlusion were achieved.
Highlights
- •
Managing transmigrated and impacted canines with congenitally missing teeth is a challenge.
- •
A transmigrated mandibular right canine was extracted and autotransplantation performed.
- •
A 3D acrylic prototype of the donor tooth was used to prepare the recipient site.
- •
The autotransplant was mesially protracted by 4 to 5 mm.
- •
The contralateral impacted canine was erupted into the arch using mini-implants.
Transmigration is the term used by some authors to define an unerupted mandibular canine crossing the midline. The reported incidence of transmigrated mandibular canines ranges from 0.05% to 0.4%. The etiology of impacted mandibular canines is largely unknown or is multifactorial. Tumors, cysts, odontomas, premature loss of deciduous teeth, prolonged retention of deciduous canines, crowding, spacing, abnormally increased eruption force of the canines, and a genetic origin associated with hypodontia are some factors that have been suggested to play a role in the transmigration of mandibular canines.
The management of transmigrated mandibular canines is complicated and may preclude an ideal treatment outcome. Surgical extraction, transplantation, or autotransplantation and surgical exposure followed by orthodontic alignment are common approaches for the management of transmigrated canines. The deciding factor for selecting the most appropriate treatment plan depends on the position of the transmigrated canines. Additionally, the treatment complexity is further increased when transmigration is associated with congenitally missing teeth, especially in a Class II malocclusion. In these circumstances, it may be necessary to promote the eruption of the canines into the arch and replace the missing mandibular premolars with endosseous implants, close the edentulous space, or resort to autotransplantation.
Autotransplantation of a tooth is a highly sensitive procedure that involves the preparation of the recipient site with a trial-and-error method using a donor tooth as a template. This leads to increased extra-alveolar time and, more importantly, may damage the periodontal ligament cells of the donor tooth and cause pulpal necrosis. However, with the introduction of cone-beam computed tomography (CBCT) imaging and 3-dimensional (3D) printing of stereolithographic models with rapid prototyping technologies, these concerns can be addressed. It is now possible with 3D imaging to visualize the recipient site and the donor tooth. Additionally, the adaptability of the donor tooth to the recipient site in the buccolingual dimension can be evaluated on the CBCT images. Subsequently, this information can be exported into a software program for virtual planning and eventual printing of the donor tooth template with rapid prototyping techniques. The stereolithographic donor tooth template can aid in the recipient socket preparation and may reduce the manipulation of the donor tooth and the extra-alveolar time during the autotransplantation of the tooth.
This case report illustrates the treatment of a patient with a Class II malocclusion, congenitally missing mandibular second premolars, and severely impacted mandibular canines. An ipsilateral maxillary premolar was autotransplanted to the missing mandibular right second premolar site using 3D CBCT-based rapid prototyping techniques for stereolithographic donor tooth fabrication. Additionally, the autotransplanted tooth had to be significantly protracted after extraction of the transmigrated mandibular canine. The severely impacted mandibular left canine was erupted using direct and indirect anchorage from a miniscrew placed in the mandibular buccal ridge.
Etiology and diagnosis
An adolescent Hispanic girl, aged 12.5 years, reported to the orthodontic clinic at the University of Connecticut with the primary complaint that her canines were compressed in her jaw. Her extraoral examination showed a convex soft tissue profile with competent lips and an obtuse nasolabial angle ( Fig 1 ). Intraorally, the patient had retained deciduous second molars and canines with unerupted canines. Dentally, she had a Class II molar relationship on the right side and a Class I relationship on the left side, with an overbite of 5 mm and a normal overjet ( Fig 2 ).


The lateral cephalometric analysis ( Fig 3 ) showed a Class II skeletal base, a convex profile caused by a retrognathic mandible, and a hyperdivergent growth pattern. Dentally, the maxillary incisors were retroclined, and the mandibular incisors were flared. The upper and lower lips were protrusive in reference to the E-plane.
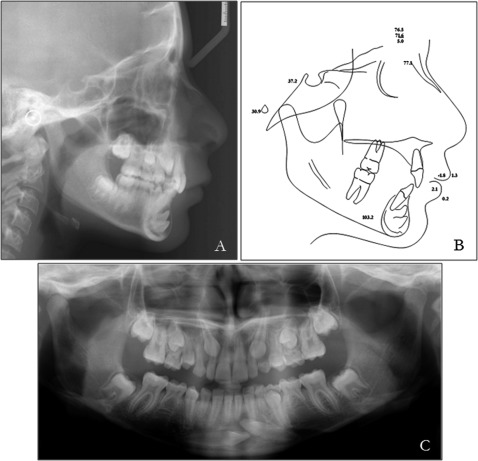
The panoramic radiograph showed transmigration of the mandibular right canine, a severely impacted left canine, and congenitally missing mandibular second premolars ( Fig 3 ). The oral radiologist reported a large radiolucent area arising from the cementoenamel junction of the impacted canines and recommended further evaluation with CBCT. A CBCT scan (6-in field of view, voxel size of 0.2 mm, exposure time of 10 seconds) was acquired. The impacted canine crowns were located labially, inferior to the apices of the mandibular incisors, and the crowns were surrounded by a well-defined round corticated radiolucent area. The radiolucent lesion from both impacted canines formed 1 large lesion with the greatest diameters of 14.2 mm vertically and 8.2 mm horizontally. The border of the lesion was attached to the cementoenamel junction of both impacted canines, and the radiographic features of the lesion suggested a dentigerous cyst ( Fig 4 , A-C ).
Treatment objectives
The primary treatment objectives were to (1) address her chief complaint of bringing the impacted canines into the arch, (2) replace the missing mandibular premolars with autotransplantation on the right and molar protraction on the left, (3) maintain the facial profile, and (4) achieve a normal overbite.
Treatment objectives
The primary treatment objectives were to (1) address her chief complaint of bringing the impacted canines into the arch, (2) replace the missing mandibular premolars with autotransplantation on the right and molar protraction on the left, (3) maintain the facial profile, and (4) achieve a normal overbite.
Treatment alternatives
The first alternative was extraction of the transmigrated mandibular right canine, bringing the mandibular left canine into the arch and retaining the mandibular deciduous second molars. However, with this approach, an implant-based restoration would be needed for the extracted mandibular right canine after completion of growth. Additionally, predicting the long-term survival of the mandibular deciduous second molars is difficult, although their average survival rate has been reported to be more than 90%. However, if the deciduous second molars were lost, at least 1 additional implant-based single crown might have been necessary, increasing the costs to the patient. Furthermore, an implant for the extracted transmigrated canine or significant protraction of the buccal segment would be required for an ideal occlusion.
The second alternative was extraction of the transmigrated mandibular right canine, bilateral extractions of the mandibular deciduous second molars, autotransplantation of the maxillary right canine to the position of the missing mandibular right canine, and eruption of the mesioangularly impacted mandibular left canine into the arch. Additionally, we would enhance the protraction of autotransplanted tooth and the posterior mandibular segment by 4 to 5 mm to close the extraction space of the mandibular right canine. Space closure of the mandibular left deciduous second molar would be accomplished by protraction of the mandibular left first molar. This biologic treatment approach would eliminate the need for prosthetic replacement, and the treatment plan could be executed irrespective of the patient’s growth status.
Both treatment options were discussed with the patient and her parents; they accepted the second option because it obviated the need for endosseous implants for the mandibular right canine.
Treatment progress
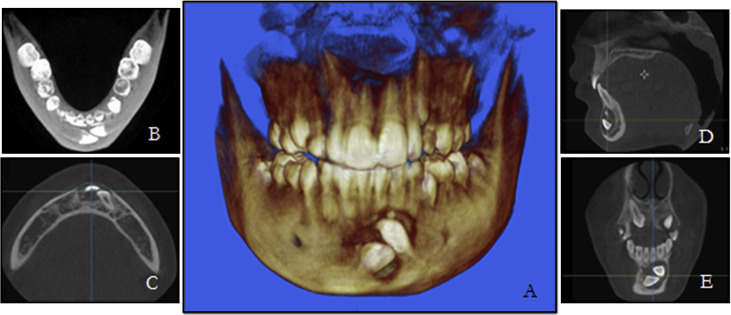
The patient was referred to the oral maxillofacial surgery clinic at the University of Connecticut for extraction of the mandibular right canine. After that, curettage was done to remove the cystic lining, and a specimen was sent for histopathology examination. The histologic features suggested a dentigerous cyst. Surgical exposure of the mandibular left canine was performed, the cystic lining was removed, and a gold chain was bonded to the crown. After 4 weeks, 0.022-in preadjusted edgewise brackets were bonded on the mandibular incisors, and the patient was referred for autotransplantation of the maxillary right second premolar to replace the missing mandibular right second premolar. The preoperative CBCT data were exported in DICOM format into software (Biomedical Modeling, Boston, Mass), and the donor tooth was segmented ( Fig 5 , A ) and finally converted into the virtual donor tooth prototype ( Fig 5 , B ). Subsequently, the virtual donor tooth was printed using a rapid prototyping machine ( Fig 5 , C ).
During the autotransplantation procedure, after extraction of the mandibular deciduous right second molar, the recipient socket was further prepared by removing the interseptal bone. The stereolithographic donor tooth template was used to check for the accuracy of fit during the recipient socket wall preparation. Once the accuracy was acceptable between the recipient socket and the stereolithographic donor tooth ( Fig 5 , D-F ), the maxillary deciduous right second molar was extracted. Then, the maxillary right second premolar was extracted atraumatically and transplanted immediately to the recipient site in the first attempt, with the recorded extra-alveolar time less than 2 minutes ( Fig 5 , G and H ). The accuracy of fit was good, and optimal contact was obtained with minimal mobility of the transplanted tooth. The autotransplanted tooth was splinted with sectional 0.020-in stainless steel segments ( Fig 5 , I ); the rigid splinting was removed after 4 weeks. A follow-up periapical radiograph was taken after 5 months to evaluate the autotransplanted premolar ( Fig 6 ). The radiograph showed an increase in root length and a normal periodontal ligament space, with a healed socket; clinically, the tooth tested positive in the vitality tests.




