Lymphoma is a general term for a complex group of heterogeneous lymphoreticular malignancies. Lymphoma is the sixth most common malignancy and the second most common neoplasm of the head and neck after squamous cell carcinoma and accounts for 50-59% of head and neck neoplasms in children. They constitute approximately 3-5% of all known malignancies and are generally divided into two morphologically distinct types: Hodgkin’s lymphoma (HL) and non-Hodgkin’s lymphoma (NHL). These malignancies typically arise within the lymphatic tissues and can progress to extranodal disease as in NHL. Cervical lymph node involvement can be present in any type of lymphoma. HL extends by means of contiguous nodal spread whereas NHL tends to disseminate hematogenously and is typically a systemic diagnosis. Within the head and neck, Waldeyer’s ring is the most common site of involvement, accounting for more than half of all extranodal head and neck lymphomas. Oral involvement by lymphoma may represent a localized disease process but is more often part of a systemic process that secondarily involves the cervical lymph nodes.
Lymphoma arising within the oral cavity accounts for less than 5% of all oral malignancies, and approximately 85% of these lesions involve the pharyngeal tonsil and the palate ( Figure 38-1 ). Extralymphatic sites include the salivary glands, paranasal sinuses, oral cavity, and larynx.

Lymphomas are currently classified based on morphologic, immunophenotypic, genetic, and clinical features. Several classification systems have been used to classify lymphomas, including the World Health Organization (WHO) classification, which is based on the principles defined in the Revised European-American Classification of Lymphoid Neoplasm (REAL). Both the WHO and REAL classifications subdivide lymphomas based on cell of origin ( Box 38-1 ) :
- •
B-cell lymphoma
- •
T-NK(natural killer)–cell lymphoma
- •
HL
- •
Others (histiocytic and dendritic cell processes, mastocytosis, etc.)
Hodgkin’s Lymphoma
- •
Classical Hodgkin’s lymphoma
- •
Nodular sclerosis
- •
Mixed cellularity
- •
Lymphocyte-rich
- •
Lymphocyte-depleted
- •
- •
Nodular lymphocyte predominant Hodgkin’s lymphoma
Non-Hodgkin’s Lymphoma
- •
Precursor B-cell neoplasms
- •
Mature B-cell neoplasms
- •
Small cell lymphoma/chronic lymphocytic leukemia
- •
Extranodal marginal zone B-cell lymphoma of mucosa associated lymphoid tissue (MALT-lymphoma)
- •
Follicular
- •
Mantle cell
- •
Diffuse large cell
- •
Burkitt (African and endemic)
- •
Others
- •
- •
Precursor T-cell
- •
Mature NK/T-cell
- •
Extranodal NK/T-cell lymphoma, nasal type
- •
Anaplastic large cell
- •
Mycosis fungoides
- •
Others
- •
DIAGNOSIS
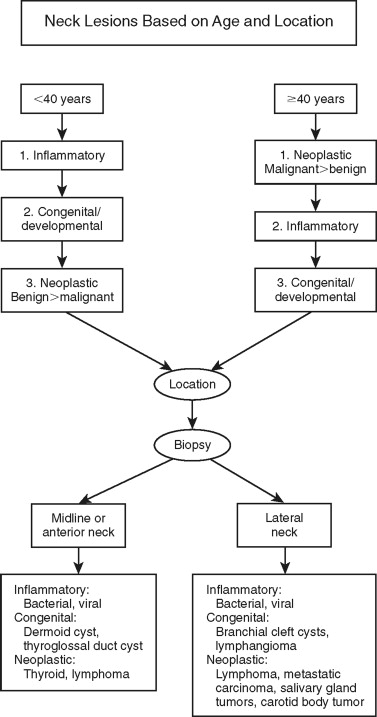
Patients often present with a neck mass to oral and maxillofacial surgeons ( Figure 38-2 ). Therefore, it is critical when assessing neck masses to have a well-developed algorithm for their evaluation. This will enable earlier stage diagnosis and expeditious treatment.

The diagnosis of lymphoma is based on the histopathologic examination of enlarged cervical lymph nodes or from extralymphatic tissue. Immunophenotyping of lymphomas, either by immunohistochemistry or flow cytometry, is critical for accurate classification of a lymphoma. The majority of B-cell lymphomas express the pan-B cell antigen CD20, whereas T-cell lymphomas express the T-cell antigen CD3. Both sets are positive for the leukocyte common antigen CD45. HL is a particular type of lymphoma with its own immunoprofile.
Nodal presentation of a lymphoma typically presents with a neck mass of small to medium-sized lymph nodes with a rubbery consistency that progressively becomes larger. Lymph nodes greater than 1 cm that persist for more than 4-6 weeks in the absence of infection should be evaluated histologically. There are several specific criteria for biopsy of suspected lymphoma. It is preferable that the largest accessible lymph node be removed for histologic diagnosis, with excisional biopsy providing the highest yield diagnostically. The excised lymph node should be preferably intact and undistorted. Fine-needle aspiration (FNA) may on occasion be diagnostic when augmented with immunophenotyping studies and is a useful diagnostic modality for intra-abdominal, thoracic, or retroperitoneal lymph nodes. FNA is often used to obtain tissue for surveillance in the post-treatment setting.
The clinical staging of NHL and HL is based upon a combination of clinical, radiologic, and surgical findings. In order to appropriately stage lymphoma, a complete medical history, physical examination, urinalysis, blood chemistries, complete blood count with differential, and a bone marrow biopsy are required. Imaging modalities are also required, and this centers on obtaining a CT scan with intravenous contrast, which should include the head and neck, mediastinum, abdomen, and pelvis. A bone marrow biopsy is typically performed from the iliac crest, since approximately 18% of non-HLs involve the bone marrow. If CNS involvement is suspected, a lumbar puncture is indicated. For patients with head and neck lesions, a nasopharyngoscopy should also be performed. The immunohistochemical analysis of the tumor is essential for diagnosis and for targeting novel therapies.
The Ann Arbor staging system ( Figure 38-3 ) is applicable to both HL and NHL and provides the basis for staging. The Ann Arbor system for staging depends upon the number of lymph node regions involved, the presence of extranodal disease, the presence of disease above and below the diaphragm, and the existence of concomitant constitutional symptoms ( category A for those patients without systemic symptoms; category B for patients with defined systemic symptoms including fever, chills, night sweats, and greater than 10% weight loss). These symptoms are more commonly associated with HL and are prognostically significant if present for both NHL and HL. In addition to routine histologic examination, the presence of genetic and chromosomal abnormalities is common in lymphoma. Aneuploidy occurs in HL, and translocations such as c-myc gene may be seen in Burkitt’s lymphoma and bcl-2 may often be found in follicular lymphomas. Infection such as Epstein-Barr virus, HIV-1, Helicobacter pylori , hepatitis B and C, and human herpesvirus 8 may all be implicated in the pathogenesis of lymphoma. The presence of chronic inflammation also increases the risk of developing lymphoma as is seen with mucosa-associated lymphoid tissue (MALT) lymphoma in patients with Sjögren syndrome and rheumatoid arthritis.
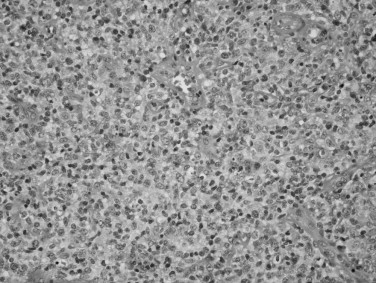
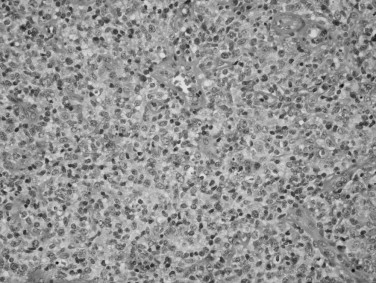
HODGKIN’S LYMPHOMA
HL is a disorder that is localized to the lymph nodes in greater than 90% of cases. HL can be divided into two forms: classical HL (CHL) and nodular lymphocyte predominant HL (NLPHL). CHL is further subtyped into nodular sclerosis, mixed cellularity, lymphocyte-rich, and lymphocyte-depleted forms. Distinguishing CHL from NLPHL is the most important breakpoint because of their differing clinical presentation, behavior, and immunohistologic features. The majority of cases (95%) are of the classical form, with the nodular sclerosis subtype accounting for 70% of these. This type of classic lymphoma has a bimodal age distribution with a peak incidence between 20 and 25 years and a second peak in the eighth decade. In the majority of cases (98%) the malignant cells of CHL arise from a mature B-cell. The uninucleated forms are referred to as Hodgkin cells or Reed-Sternberg cell variants, whereas the multinucleated, diagnostic cells are referred to Reed-Sternberg cells ( Figure 38-4 ). All Hodgkin cells in CHL have a similar immunophenotype: CD30(+), CD45(−), and CD20(−/+) (typically negative). Approximately 5% of HL cases are of the NLPHL type, which may occur at any age with a peak between 30 and 50 years old. Like CHL, NLPHL also arises from a mature B-cell. However, the neoplastic cells in this type are characterized as large cells with convoluted nuclei. Hence, they are referred to as popcorn or L&H cells (lymphocytic and/or histiocytic Reed-Sternberg cell variants). In contrast to classic RS cells, L&H cells are typically CD30(−), CD45(+), and CD20(+). HL is very uncommon in children less than 5 years of age.
HL accounts for approximately 14% of all lymphomas, making it significantly less common than NHL. HL presents rarely as extranodal disease (1-4%), whereas NHL occurs in extranodal sites in up a third of cases. Classically, HL occurs in a single lymph node that then progressively involves contiguous lymph node structures. This pattern is in contrast to NHL where noncontiguous spread to lymphatic structures or extranodal sites is more commonly seen. Clinically, HL causes generalized symptoms or laboratory abnormalities in 41% of patients as compared with 27% of patients with NHL. The distinction between HL and NHL can only be made histopathologically, since clinical and radiographic presentation often fail to distinguish between these two groups of lymphomas. The distribution of lymph node involvement between HL and NHL varies, with 24% of patients with HL versus 33% of patients with NHL presenting with cervical lymphadenopathy.
HODGKIN’S LYMPHOMA
HL is a disorder that is localized to the lymph nodes in greater than 90% of cases. HL can be divided into two forms: classical HL (CHL) and nodular lymphocyte predominant HL (NLPHL). CHL is further subtyped into nodular sclerosis, mixed cellularity, lymphocyte-rich, and lymphocyte-depleted forms. Distinguishing CHL from NLPHL is the most important breakpoint because of their differing clinical presentation, behavior, and immunohistologic features. The majority of cases (95%) are of the classical form, with the nodular sclerosis subtype accounting for 70% of these. This type of classic lymphoma has a bimodal age distribution with a peak incidence between 20 and 25 years and a second peak in the eighth decade. In the majority of cases (98%) the malignant cells of CHL arise from a mature B-cell. The uninucleated forms are referred to as Hodgkin cells or Reed-Sternberg cell variants, whereas the multinucleated, diagnostic cells are referred to Reed-Sternberg cells ( Figure 38-4 ). All Hodgkin cells in CHL have a similar immunophenotype: CD30(+), CD45(−), and CD20(−/+) (typically negative). Approximately 5% of HL cases are of the NLPHL type, which may occur at any age with a peak between 30 and 50 years old. Like CHL, NLPHL also arises from a mature B-cell. However, the neoplastic cells in this type are characterized as large cells with convoluted nuclei. Hence, they are referred to as popcorn or L&H cells (lymphocytic and/or histiocytic Reed-Sternberg cell variants). In contrast to classic RS cells, L&H cells are typically CD30(−), CD45(+), and CD20(+). HL is very uncommon in children less than 5 years of age.
HL accounts for approximately 14% of all lymphomas, making it significantly less common than NHL. HL presents rarely as extranodal disease (1-4%), whereas NHL occurs in extranodal sites in up a third of cases. Classically, HL occurs in a single lymph node that then progressively involves contiguous lymph node structures. This pattern is in contrast to NHL where noncontiguous spread to lymphatic structures or extranodal sites is more commonly seen. Clinically, HL causes generalized symptoms or laboratory abnormalities in 41% of patients as compared with 27% of patients with NHL. The distinction between HL and NHL can only be made histopathologically, since clinical and radiographic presentation often fail to distinguish between these two groups of lymphomas. The distribution of lymph node involvement between HL and NHL varies, with 24% of patients with HL versus 33% of patients with NHL presenting with cervical lymphadenopathy.
NON-HODGKIN’S LYMPHOMA (NHL)
NHL represents a diverse group of lymphoreticular neoplasms, which may be divided broadly into B-cell and T-cell forms. Mature B-cell lymphomas constitute over 85% of NHL worldwide. Some forms include follicular lymphoma, B-cell chronic lymphocytic leukemia/small lymphocytic lymphoma, diffuse large B-cell lymphoma, lymphoplasmacytic lymphoma, splenic marginal zone lymphoma, extranodal marginal zone B-cell lymphoma of MALT lymphoma, mantle cell lymphoma, and Burkitt’s lymphoma. All of these lymphomas share expression of the pan-B-cell marker CD20. In addition, many of them also have other specific immunophenotypic profiles that allow for definitive classification. Plasma cell proliferations, such as myeloma or plasmacytoma, also fall under the category of mature B-cell neoplasms, but these are typically CD20(−).
The gastrointestinal system is the most frequently involved extranodal site, which occurs in over 50% of patients. This is followed by the head and neck, which is affected in 11-33% of patients. NHL of the head and neck arises in lymph nodes in 65% of cases and in extranodal sites in 25-30%. NHL of the head and neck occurs predominantly in patients between the ages of 50 and 60. NHL may spread to regional and distant lymphatic sites as well as parenchymal organs including liver, spleen, and bone marrow.
Follicular lymphoma (FL) occurs in an older population, has a relatively indolent course, and constitutes approximately 40% of NHL in adults. It typically manifests as painless lymphadenopathy, splenomegaly, and bone marrow involvement. This lymphoma has a follicular center cell origin and histologically has nodular effacement of the lymph node. The lymphoma cells are CD20, CD10, BCL6, and BCL2(+). BCL2 is an anti-apoptosis gene, which is expressed in FL and allows for distinction from reactive follicular hyperplasia, which is BCL2(−).
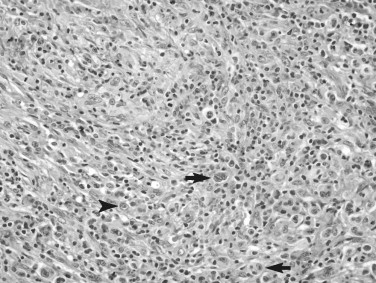
Extranodal marginal zone B-cell lymphoma of MALT lymphoma also displays an indolent clinical evolution. This type of lymphoma is commonly seen within the head and neck and in particular extralymphatic sites such as the thyroid and salivary glands and is commonly associated with other autoimmune diseases such as Hashimoto’s thyroiditis and Sjögren’s syndrome. This lymphoma forms characteristic lymphoepithelial lesions in which the neoplastic lymphocytes infiltrate and injure ducts and glands of the involved organ ( Figure 38-5 ).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


