Key points
- •
Preoperative planning is crucial to a successful lower eyelid procedure. The surgeon must decide between transconjuctival approach, transcutaneous approach, or a combination of both to address lower lid dermatochalasis and steatoblepharon.
- •
Lower lid horizontal laxity must be identified before surgery so that it may be properly addressed. This can be accomplished with the eyelid distraction test and the eyelid snap test.
- •
A deep nasojugal fold or tear trough deformity must be addressed for optimum esthetic outcome. This can be accomplished with the use of fillers, autologous fat grafting, resuspension of orbital fat, or facial implants.
Introduction
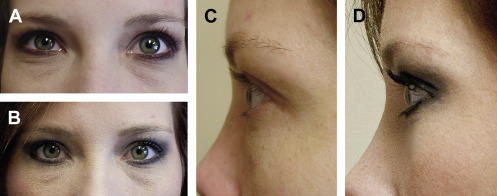
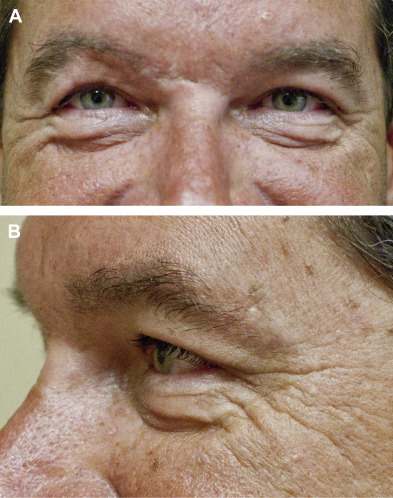
Restoration of the aging periorbita to a more refreshed, youthful appearance is arguably one of the most rejuvenating facial cosmetic procedures performed. Blepharoplasty is one of the most frequently performed procedures in the rapidly growing field of cosmetic surgery with more than 200,000 cases documented in 2014, ranking fourth of all procedures. Most patients seeking cosmetic surgery of the lower eyelid are most concerned with dark circles underneath their eyes and “looking tired.” A youthful lower eyelid should have a gentle convexity that blends into the upper cheek mound. As the midface ages, periorbital fat can herniate or prolapse through a weakened orbital septum. Known as steatoblepharon or pseudoherniation, this can even be troublesome for young patients ( Fig. 1 ). This, combined with a descent of the malar fat pad, can lead to a double convexity deformity and a deep nasojugal fold. Treatment of the lower eye is aimed at eliminating or tightening redundant skin and muscle, correcting lid laxity, and resecting or redraping retroseptal fat to create a smooth lid-cheek junction ( Figs. 2–5 ). Lower eyelid surgery, however, can be technically challenging, and significant functional defects can result if proper surgical technique and preoperative assessment is not performed.

Introduction
Restoration of the aging periorbita to a more refreshed, youthful appearance is arguably one of the most rejuvenating facial cosmetic procedures performed. Blepharoplasty is one of the most frequently performed procedures in the rapidly growing field of cosmetic surgery with more than 200,000 cases documented in 2014, ranking fourth of all procedures. Most patients seeking cosmetic surgery of the lower eyelid are most concerned with dark circles underneath their eyes and “looking tired.” A youthful lower eyelid should have a gentle convexity that blends into the upper cheek mound. As the midface ages, periorbital fat can herniate or prolapse through a weakened orbital septum. Known as steatoblepharon or pseudoherniation, this can even be troublesome for young patients ( Fig. 1 ). This, combined with a descent of the malar fat pad, can lead to a double convexity deformity and a deep nasojugal fold. Treatment of the lower eye is aimed at eliminating or tightening redundant skin and muscle, correcting lid laxity, and resecting or redraping retroseptal fat to create a smooth lid-cheek junction ( Figs. 2–5 ). Lower eyelid surgery, however, can be technically challenging, and significant functional defects can result if proper surgical technique and preoperative assessment is not performed.
Preoperative planning
Before any cosmetic surgical procedure, a thorough history and physical examination should be performed. A contraindication to a general surgical procedure is most likely a contraindication to eyelid surgery. Specific to blepharoplasty, ocular history should be elicited from the patient, including history of previous eye surgeries, visual disturbances, use of corrective lenses or contacts, thyroid eye disease, and dry eyes. Lower lid blepharoplasty can be performed in the presence of dry eye syndrome with less risk of potential complications; however, the patient should be informed of the risk before surgery.
To minimize the risk of bleeding, preoperative assessment should include an investigation of medications and herbal supplements that possess anticoagulation properties. Although not an exhaustive list, patients should discontinue aspirin, clopidogrel, nonsteroidals, warfarin, vitamin E, fish oil, and herbal preparations, including St. Johns wort and gingko biloba before surgery. As with any medication, obtain medical consultation as necessary before discontinuation. Alcohol consumption can also increase the risk of bleeding and should be discontinued 2 weeks before surgery.
Horizontal lid laxity should be documented before surgery, because this will guide treatment. Quantitative measures including a snap and distraction test must be documented. A positive lid snap test is defined as greater than 1 second of time elapse for the eyelid returning to its normal position following inferior displacement. The lid distraction test is performed by pulling the lid in an anterior direction away from the globe. Laxity of greater than 6 to 7 mm is considered abnormal, and a lid tightening procedure should be considered ( Fig. 6 ). Lid retraction can be measured quantitatively using margin reflex distance. Margin reflex distance is defined as the distance from the corneal eye reflex to the central portion of the lower lid. Typically this distance is 5 mm with lid retraction increasing this measurement. Simplified, the lower lid should rest at the level of the lower limbus without scleral show. In addition, the surrounding architecture of the periorbita is a predictor of lid position following surgery. Patients with a negative vector as defined by the most anterior portion of the globe lying anterior to the orbital rim are candidates for operative lid support.
Excess or pseudoherniated fat should also be evaluated preoperatively. Gentle ballotement of the globe with the patient in the upright position will determine the location and need for fat removal. Patients should also be evaluated in full smile because hypertrophic orbicularis oculi may be mistaken for excess fat and must be addressed appropriately.
Preparation and patient markings
Standardized and high-quality preoperative and postoperative photographs are an absolute necessity in cosmetic surgery. A standard blepharoplasty series should include full-face frontal, lateral, and three-quarter views as well as close-ups of the same views. In addition, a frontal photograph should be taken with the eyes gazing upward. The authors’ preference is to take these photographs at the preoperative appointment with makeup on and on day of surgery without makeup. The photographs should also be taken following surgical markings.
Although the patient is in the upright position and in upward gaze, prominent prolapsed orbital fat is marked for removal with an indelible marker. In addition, for the transcutaneous skin muscle flap approach, an incision line is marked 2 to 3 mm inferior to the lash line. This incision should begin 1 mm lateral to the inferior punctum and extend laterally approximately 6 to 8 mm lateral to the lateral canthus. The incision line should be tailored into a lateral rhytid in the area of the crow’s feet ( Fig. 7 ). For a skin pinch blepharoplasty, cotton forceps are used to pinch a roll of skin below the lash line, producing slight lash eversion. The redundant tissue is then marked for excision ( Fig. 8 ).
Patient positioning and surgical technique
General anesthesia is preferred for most cosmetic procedures; however, isolated lower lid blepharoplasty can easily be performed with local anesthesia, conscious sedation, or intravenous sedation. Whichever route is used, local anesthesia is a key component. The patient is placed in a supine position before initiation of sedation. One to 2 drops of 0.5% proparacaine or tetracaine ophthalmic are placed into each eye. Corneal eye shields are then placed bilaterally ( Fig. 9 ). Local anesthesia is injected into the lower eye conjunctiva into medial, central, and lateral fat pads using a 30-gauge needle. A measure of 1% lidocaine (Xylocaine) with 1:100,000 epinephrine can be mixed with a 1:10 dilution of sodium bicarbonate to lessen the initial discomfort of injection through alkalinization of the solution. Local anesthesia should also be injected in a subcutaneous, premuscular plane along the subciliary incision line. If canthopexy/canthoplasty is planned, additional local anesthesia should be injected along the lateral and inferior orbital rim ( Fig. 10 ). The patient is then prepared with betadine or comparable antiseptic solution and draped in sterile fashion. This step allows appropriate time for the hemostatic effect of the epinephrine. If fat grafting is planned, abdominal fat harvest can be performed at this time ( Figs. 11 and 12 ).




