Introduction
The objective of this study was to evaluate the surface enamel after bracket debonding and residual resin removal.
Methods
Thirty patients (female, 20; male, 10; mean age, 18.4 years) who completed orthodontic treatment with fixed appliances (Twin Brackets, 3M Unitek, Monrovia, Calif) (n = 525) were included. The amounts of adhesive left on the tooth surfaces and the bracket bases were evaluated with the adhesive remnant index (ARI). ARI tooth (n = 498) was assessed on digital photographs by 2 operators. After resin removal and polishing, epoxy replicas were made from the maxillary anterior teeth (n = 62), and enamel surfaces were scored again with the enamel surface index. Elemental analysis was performed on the debonded bracket bases by using energy dispersive x-ray spectrometry mean area scanning analysis. The percentages of calcium and silicon were summed up to 100%. Tooth damage was estimated based on the incidence of calcium from enamel in relation to silicon from adhesive (Ca%) and the correlation between the ARI bracket and Ca%.
Results and Conclusions
While ARI tooth results showed score 3 as the most frequent (41%) ( P <0.05), followed by scores 0, 1, and 2 (28.7%, 17.9%, and 12.4%, respectively), ARI bracket results showed score 0 more often (40.6%) than the other scores ( P <0.05). Maxillary anterior teeth had significantly more scores of 3 (49%) than the other groups of teeth (10%-25%) (chi-square; P <0.001). There were no enamel surface index scores of 0, 3, or 4. No correlation between the enamel surface index and ARI tooth scores was found (Spearman rho = 0.014, P = 0.91). The incidence of Ca% from the scanned brackets showed significant differences between the maxillary and mandibular teeth (14% ± 8.7% and 11.2% ± 6.5%, respectively; P <0.05), especially for the canines and second premolars (Kruskal-Wallis test, P <0.01). With more remnants on the bracket base, the Ca% was higher (Jonckheere Terpstra test, P <0.05). Iatrogenic damage to the enamel surface after bracket debonding was inevitable. Whether elemental loss from enamel has clinical significance is yet to be determined in a long-term clinical follow-up of the studied patient population.
After orthodontic therapy with fixed appliances, from the clinical standpoint, a major concern is to avoid cohesive failures in the enamel during debonding brackets and at the same time to obtain tooth surfaces without adhesive. Bonding onto and removal of brackets from the enamel surfaces are potential risks for topographic changes in the form of cracks, scarring, scratches, or loss of enamel. The dilemma in adhesion of brackets in orthodontics is that it should be strong enough to prevent failure during all treatment but also low enough so that enamel damage would be none or minimal during bracket removal after treatment.
Debonding forces can be influenced by many factors: type of enamel conditioning agents (phosphoric acid, self-etching primers, polyacrylic acid), adhesive resin, cement, polymerization methods, bracket type, or bracket base architecture. Usually, an increase in debonding force causes an increased risk of enamel damage. Even though the dental literature contains many studies looking at these possible factors on bracket adhesion, their clinical significance remains scarce, since, in in-vitro studies, data are usually obtained without considering major intraoral factors—eg, saliva, masticatory forces, temperature, and pH changes. Furthermore, clinical debonding with pliers creates a combination of shear, tensile, and torque forces. Therefore, 1 test method (shear or tensile) in vitro might not represent in-vivo debracketing techniques and, consequently, in-vivo bond strengths and failure types. Several debonding techniques were introduced, but there were insufficient data regarding diverse susceptibility to debonding damage in the maxillary or mandibular dental arches or in specific tooth groups. Bracket debonding strength for incisors in vitro requires significantly higher shear strength compared with molars. However, the effect of enamel damage relative to the tooth type is unknown. Because of variations in enamel thickness or enamel prism orientation, different failure types could be expected depending on the tooth type. Since etched anterior teeth have greater mean areas than do posterior teeth, it can be expected that anterior teeth have greater potential for enamel damage than do posterior teeth.
Possible failure types after bracket debonding are either adhesive between the enamel and the adhesive resin, partially adhesive and cohesive in the adhesive resin (mixed), or adhesive between the bracket base and the adhesive resin, where the latter 2 require removal of the remnants. Unfortunately, remnant removal can eventually cause further unwanted damage in the enamel because it is often done with rotating instruments. Various methods are available to remove adhesive remnants: pliers, scalers, abrasive disks, diamond or tungsten carbide burs, stones, or ultrasonic instruments. Although consensus is lacking in the dental literature, the most common and efficient way of removing adhesive remnants in daily practice is with tungsten carbide burs in a low-speed rotating hand piece. Potential detrimental effects of bracket debonding from enamel or elemental loss from surface enamel either during bracket debonding or removal of the remnants is an iatrogenic problem. Calcium loss from the enamel surface particularly can result in dental erosion, which is a localized loss of dental hard tissues.
Although enamel surface morphology after bracket debonding has been the topic of some in-vitro studies, quantitative information relevant to enamel damage after bracket debonding in vivo is limited. Therefore, the objective of this study was to evaluate the surface morphology and the elemental loss from surface enamel by using a semidirect method in an in-vivo and ex-vivo study.
Material and methods
Thirty consecutive patients (20 female, 10 male; mean age, 18.4 years) who completed orthodontic treatment with fixed appliances (Twin Brackets, 3M Unitek, Monrovia, Calif) were included in this study. The surface areas of the brackets provided by the manufacturer were as follows: maxillary central incisor, 10.52 mm 2 ; maxillary lateral incisor, 8.97 mm 2 ; maxillary canine, 10.19 mm 2 ; maxillary premolar, 9.61 mm 2 ; maxillary molar, 10.21 mm 2 ; mandibular incisor, 9.81 mm 2 ; mandibular canine, 10.129 mm 2 ; mandibular premolar, 9.61 mm 2 ; and mandibular molar, 10.21 mm 2 . During the orthodontic treatment, the patients received the corresponding stainless steel brackets on all teeth in the mandible and the maxilla except on the second molars. Direct bracket bonding was done by 5 operators. A standardized protocol was followed for adhering the brackets to the tooth surfaces. Enamel surfaces were cleaned with water and fluoride-free pumice (Zircate Prophy Paste, Dentsply Caulk, Milford, Del) with a prophylaxis brush (Hawe Prophy-Cup Latch-Type, KerrHawe SA, Bioggio, Switzerland), rinsed with water, and dried with an air syringe. Each tooth surface was etched with 37% H 3 PO 4 (Total etch, Ivoclar Vivadent, Schaan, Liechtenstein) for 30 seconds, rinsed thoroughly with an oil-free air-water spray for 20 seconds, and air dried until they appeared frosty. The bonding adhesive (Heliobond, Ivoclar Vivadent) was applied with a microbrush, air thinned, and photo-polymerized for 10 seconds (Ortholux, 3M Unitek, St Paul, Minn). Then the brackets were bonded by using adhesive cement (Transbond XT, 3M Unitek). After removal of the excess around the bracket margins with the tip of a probe, they were photo-polymerized from 5 directions: above the bracket, cervico-incisal, inciso-cervical, mesial, and distal for 20 seconds each (Ortholux, 3M Unitek) (light output, 430-480 nm).
At the end of treatment, all brackets were debonded by placing the debonding pliers (Dentronix E231, Konstanz, Germany) at the outer wings of the bracket. One clinician carried out all debonding procedures. After debonding, the gross adhesive remnants were removed with a tungsten carbide bur (Komet H22 AGK 016, Lemgo, Germany) in a slow-speed hand piece under water cooling. Subsequently, the remaining resin was removed with a fine tungsten carbide bur (Komet H46 204 012) in a slow-speed handpiece. After removing the resin, the tooth surfaces were polished with a polish cup (Hawe Prophy-Cup, white 967) and polishing paste (Zircate Prophy Paste, Dentsply, Konstanz, Germany). Final polishing was achieved with rubber points (Ceramiste Midipoint, Shofu, Ratingen, Germany).
The amounts of adhesive remnants were scored by using the adhesive remnant index (ARI) on all debonded bracket bases (n = 525). The ARI bracket scoring system consists of a 4-point scale from 0 to 3: 0, no adhesive left on the bracket base; 1, less than half of the adhesive remained on the bracket; 2, more than half of the adhesive remained on the bracket; and 3, all adhesive was left on the bracket.
To evaluate the adhesive remnants on the tooth surfaces, after debonding the brackets, before removing the remaining resin, the enamel surfaces were subjected to the disclosing medium (GUM Red-cote, Chicago, Ill). This allowed better contrast between the tooth-colored adhesive remnant and the enamel for the failure-site evaluation. Then standardized digital photographs (DX1 with a micro 60-mm lens, Nikon, Tokyo, Japan) were taken of the dyed tooth surfaces (n = 498). These photographs were examined by 2 calibrated observers who were blinded to the objectives of the study. The sites of the failure types were recorded by using the ARI (ARI tooth ) scoring system. In cases of conflict, consensus was reached. ARI tooth scores ranged from 0 to 3: 0, no adhesive left on the tooth; 1, less than half of the adhesive remained on the tooth; 2, more than half of the adhesive remained on the tooth; and 3, all adhesive was left on the tooth, with a distinct impression of the bracket mesh.
Possible damage to the enamel was evaluated in the maxillary anterior teeth (n = 62) only, according to the enamel surface index (ESI) described by Zachrisson and Årtun. The ESI consists of a 5-point scale from 0 to 4: 0, perfect surface with no scratches and distinct intact perikymata; 1, satisfactory surface with fine scratches and some perikymata; 2, acceptable surface with several marked and some deeper scratches with no perikymata; 3, imperfect surface with several distinct deep and coarse scratches but no perikymata; and 4, unacceptable surface with coarse scratches and deeply marked appearance. For ESI scoring, immediately after the residual adhesive removal and polishing, impressions (President, Colténe/Whaledent, Altstätten, Switzerland) were made from the entire labial surface and thereafter epoxy resin (Epofix Resin, Struers, Ballerup, Denmark) replicas were obtained. Secondary mode images were made with cold field emission scanning electron microscope (FE-SEM 6301F, Jeol, Tokyo, Japan) (magnification, 10 times) at 25 kV from epoxy replicas that were sputter-coated with 200 A° Au (BAL-TEC sputter coater; type 07 120B, Balzers, Liechtenstein) and fixed to the specimen holder with a photo-polymerized dental composite (Kulzer TransLUX EC, Wehrheim, Germany).
Enamel damage was also quantified ex vivo from the debonded brackets that received ARI bracket scores 1, 2, or 3 (n = 306). Energy dispersive x-ray spectrometry (EDX) mean area scan analysis (JSM-6400, Jeol) (accelerating voltage, 20 kV; beam current, 6.1 nA; type of detector, Si(Li)-liquid N 2 cooled, secondary mode, ThermoNoran System Six, SelectScience Ltd, Bath, UK); spectra acquisition time, 100 seconds; detector dead time, 25%; resolution, 143 eV; magnification, between 25 and 30 times; scan mode, area; type of correction, ZAF; type of analysis, standardless) was performed on the entire surface of the bracket base. The percentages of calcium (from enamel) and silcon (from adhesive) were summed up to 100%, and calcium incidence was calculated in relation to silicon in percentages (Ca%). In addition, the correlation between ARI bracket and Ca% was determined. No materials used contained calcium ( Table I ). Therefore, the calcium found on the resin was assigned to enamel loss.
| Brand name | Composition | Manufacturer | Batch number |
|---|---|---|---|
| Twin Brackets | 17-4 stainless steel alloy | 3M Unitek, Monrovia, Calif | 3017-916 3017-917 3017-918 3017-9200 |
| Heliobond | Monomer matrix: dimethacrylate <60% Bis-GMA <40% triethyleneglycol |
Ivoclar Vivadent, Schaan, Liechtenstein | H29583 154518 |
| Transbond XT | Silane-treated quartz (70-80 wt%) silane-treated silica <2% BisDMA 10-20wt% BisGMA 5-10wt% |
3M Unitek, Monrovia, Calif | 147 |
Statistical analysis
The statistical analysis was performed with the SPSS software package (version 11.5, SPSS, Chicago, Ill). Descriptive results for ARI, ESI, and Ca% were calculated and expressed as frequencies, percentages, means, and standard deviations. The frequencies of ARI tooth and ARI bracket scores were compared by using the chi-square test. Mann-Whitney U and Kruskal-Wallis tests were applied to analyze the differences in Ca% between the maxillary and mandibular teeth, and the tooth types. Ca% in relation to ARI bracket scores was analyzed by using the Jonckheere Terpstra test. Furthermore, the nonparametric Spearman correlation test was used to examine the correlation between ESI scores and ARI tooth scores. Statistical significance was defined as P <0.05 in all tests.
Results
Overall, while ARI tooth results showed that score 3 (204 of 498) was the most frequent (41%) ( P <0.05), followed by 0, 1, and 2 (28.7%, 17.9%, and 12.4%, respectively). ARI bracket results showed score 0 (213 of 525) most often (40.6%) ( P <0.05), followed by 3, 2, and 1 (29.1%, 18.1%, and 12.2%, respectively) ( Table II ). The highest incidence of ARI tooth score 3 (29%) was observed in the central incisors, and the lowest percentage of score 0 in the first molars (3%).
| ARI tooth/bracket n = 498/525 |
Score 0 (n = 143/213) % tooth /% bracket |
Score 1 (n = 89/64) % tooth /% bracket |
Score 2 (n = 62/95) % tooth /% bracket |
Score 3 (n = 204/153) % tooth /% bracket |
|---|---|---|---|---|
| Central incisor | 16/28 | 12/22 | 19/11 | 29/14 |
| Lateral incisor | 18/22 | 16/28 | 32/17 | 23/16 |
| Canine | 21/22 | 20/22 | 26/22 | 22/18 |
| First premolar | 20/14 | 33/14 | 13/27 | 16/18 |
| Second premolar | 22/10 | 18/6 | 10/17 | 9/23 |
| First molar | 3/4 | 1/8 | 0/6 | 1/11 |
The maxillary anterior teeth had significantly more scores of 3 (49%) than other groups of teeth (16%-25%) (chi-square, P <0.001) ( Table III ). Typical failure types after bracket debonding are shown in Figure 1 .
| ARI tooth | Score 0 (n = 143) % tooth |
Score 1 (n = 89) % tooth |
Score 2 (n = 62) % tooth |
Score 3 (n = 204) % tooth |
|---|---|---|---|---|
| Maxillary anterior | 20 | 25 | 45 | 49 |
| Mandibular anterior | 36 | 23 | 33 | 25 |
| Maxillary posterior | 31 | 26 | 6 | 10 |
| Mandibular posterior | 13 | 26 | 16 | 16 |
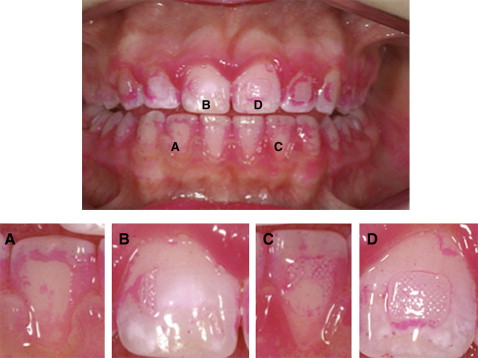
In the 62 teeth of the maxilla (28 central incisors, 28 lateral incisors, 6 canines), there were no ESI scores of 0, 3, or 4. Both scores 1 (8%) and 2 (14%) were observed the least in the canines ( Table IV ). In general, all cleaned teeth had acceptable to satisfactory enamel surfaces after debonding, with ESI scores of either 1 or 2 ( Fig 2 ). No correlation between ESI and ARI tooth scores was found (Spearman rho = 0.014, P = 0.91).
| ESI | Score 0 (n = 0) % tooth |
Score 1 (n = 40) % tooth |
Score 2 (n = 22) % tooth |
Score 3 (n = 0) % tooth |
Score 4 (n = 0) % tooth |
|---|---|---|---|---|---|
| Maxillary central incisors | 0 | 40 | 55 | 0 | 0 |
| Maxillary lateral incisors | 0 | 53 | 32 | 0 | 0 |
| Maxillary canines | 0 | 8 | 14 | 0 | 0 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


