Introduction
The objective of this study was to evaluate the long-term stability of open-bite surgical-orthodontic correction.
Methods
Thirty-nine patients at an initial mean age of 20.83 years were evaluated cephalometrically at pretreatment (T1), immediately after treatment (T2), and at the last recall (T3), with a mean follow-up time of 8.22 years. The surgical protocol included single-jaw or double-jaw surgery. Because the patients had different anteroposterior malocclusions, the sample was divided into a Class I and Class II (I-II) subgroup (3 Class I, 20 Class II malocclusion patients) and a Class III subgroup (16 patients). The dentoskeletal characteristics of the total sample and the subgroups were compared at T1, T2, and T3 with dependent analysis of variance (ANOVA).
Results
Overbite relapse in the posttreatment period was statistically significant in the whole sample and the Class I-II subgroup. Fourteen patients of the whole sample (35.9%) had clinically significant open-bite relapse (negative overbite).
Conclusions
There was a statistically significant open-bite relapse in the overall sample and in the Class I-II subgroup. The clinically significant values of long-term open-bite correction stability were 64.11%, 47.82%, and 87.50% in the overall sample, the Class I-II subgroup, and the Class III subgroup, respectively.
Long-term stability of anterior open-bite correction is a challenging problem. Several treatment protocols have been proposed to correct anterior open-bite malocclusions that can distinctly influence long-term stability. Conventional orthodontic treatment is marked by significant open-bite relapse that is greater in nonextraction treatment. On the other hand, some studies have shown that orthodontic-surgical correction of open-bite malocclusion has greater long-term stability. Because of this, sometimes orthodontic treatment of skeletal open bite in nongrowing patients has been combined with orthognathic surgery to obtain more stable results, although acceptable facial balance and occlusion can be frequently achieved with a nonsurgical open-bite approach.
Despite the smaller relapse reported with orthodontic-surgical correction, few studies have systematically evaluated the stability of open-bite surgical treatment beyond 5 years posttreatment with a significant sample size and adequate evaluation intervals. Dentoskeletal posttreatment changes seem to continue toward open-bite relapse. Some studies have evaluated the stability of open-bite correction immediately after surgery, without specifying whether treatment was completed; this could underestimate the relapse of open-bite orthodontic-surgical correction because the patient could still be having the finishing procedures of orthodontic treatment. Thus, orthodontic-surgical correction stability was evaluated considering only dentoskeletal changes after treatment in a significant open-bite sample followed in the long term.
Material and methods
The sample included 39 patients (17 male, 22 female) with open-bite malocclusion at an initial mean age of 20.83 years (range, 13.64-43.39 years), who were retrospectively selected from the files of 4 private orthodontic offices belonging to 1 orthodontist (F.A.M.).
The chief selection criterion was that the patients had an initial anterior open-bite malocclusion of at least 1 mm, treated orthodontically and surgically. Additional criteria were (1) no previous orthodontic treatment; (2) positive overbite after treatment; (3) fixed appliances removed at least 1 year after orthognathic surgery; (4) similar retention protocols; (5) no facial trauma that could have altered the growth of the apical bases; (6) no facial deformity due to buccofacial pathology, genetic syndromes, or other congenital deformities; and (7) sequential cephalometric radiographs taken at 3 stages: pretreatment (T1), posttreatment (T2), and at the last recall at least 2 years after treatment (T3).
The anteroposterior discrepancy associated with open-bite malocclusion was distributed as follows: Class I (n = 3), Class II (n = 20), and Class III (n = 16). Orthognathic surgery was restricted to the maxilla in 10 patients (6 Class II, 4 Class III) with 1-piece LeFort I osteotomy. The maxillary surgical repositioning comprised impaction only or with advancement and palatal plane rotation according to the patient’s dentoskeletal discrepancy and profile imbalance. In 9 patients (5 Class III, 4 Class II), surgical intervention was limited to the mandible. Bilateral sagittal split osteotomy (BSSO) was performed, and mandibular repositioning followed a counterclockwise rotation with advancement or setback, according to the anteroposterior discrepancy. In 20 patients (3 Class I, 10 Class II, 7 Class III), 1-piece LeFort I osteotomy was combined with BSSO to provide the planned maxillomandibular surgical repositioning. No correction of the transverse relationship was performed during the LeFort osteotomy. Maxillary transverse discrepancy was corrected by rapid maxillary expansion (RME) before the LeFort I osteotomy in 25 patients. Surgical fixation of bone segments was achieved by using intraosseous wire ligatures in 25 patients (64.1%). In 14 patients (35.9%), ostheosynthesis was performed by rigid internal fixation (RIF) by using miniplates and screws at the line of osteotomy. The patients stabilized with intraosseous wire had intermaxillary fixation with intermaxillary elastics attached to fixed appliances during postsurgical phases of 8 weeks.
The presurgical orthodontic treatment comprised leveling and alignment with fixed preadjusted appliances. Treatment planning included premolar extractions in 11 patients to correct crowding, or Class II or Class III dental compensation during the presurgical orthodontic phase. All patients were treated by the same professional team, including 2 surgeons. The mean age of the patients after the combined orthodontic-surgical treatment was 24.07 years (range, 15.3-45.77 years). The retention protocol included only a maxillary Hawley plate retainer during the first posttreatment year, and a bonded mandibular canine-to-canine retainer to stabilize the mandibular incisor alignment for a mean period of 3 years.
Because the sample consisted of patients with Class I, Class II, and Class III malocclusions and specific surgical procedures to correct certain anteroposterior discrepancies can influence the amount of relapse, the patients with Class I and Class II malocclusions became a subgroup (Class I-II), and the Class III malocclusion patients were another subgroup.
Presurgical evaluation showed that 36 patients had asymptomatic temporomandibular joints, and 3 had some symptoms of temporomandibular disorder (TMD). One had Class III, 1 had Class II, and 1 had Class I malocclusion. At T2 and T3, the asymptomatic patients’ presurgical conditions were unchanged, whereas the 3 patients with TMD symptoms had some improvement. Additionally, no patient in this sample had open-bite relapse because of condylar resorption.
The posttreatment follow-up interval began after orthodontic treatment and extended to the last posttreatment patient recall, which had a mean time of 8.22 years (range, 2.01-18.89 years). Cephalometric radiographs of each patient were obtained at T1, T2, and T3. Because of the long time span between patient recalls, the cephalometric radiographs were obtained with several x-ray machines and different magnification factors, varying from 7% to 12.6%.
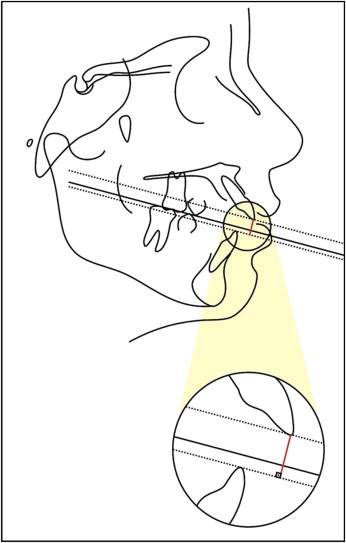
The cephalometric tracings and landmark identifications were performed by 1 investigator (F.A.M.) and then digitized with an Accugrid XNT digitizer (model A30TLF, Numonics, Montgomeryville, PA). These data were analyzed with Dentofacial Planner software (version 7.02, Dentofacial Planner, Toronto, Ontario, Canada), which corrected the magnification factors. All cephalometric measurements are described in Table I , and overbite measurement is shown in the Figure .
| Maxillary component | |
| SNA angle (°) | SN to NA |
| Co-A (mm) | Condylion to A-point |
| A-Nperp (mm) | A-point to nasion-perpendicular |
| Mandibular component | |
| SNB angle (°) | SN to NB |
| Co-Gn (mm) | Condylion to gnathion |
| P-Nperp (mm) | Pogonion to nasion-perpendicular |
| Go-Gn (mm) | Gonion to gnathion |
| Co-Go (mm) | Condylion to gonion |
| Maxillomandibular relationship | |
| ANB angle (°) | NA to NB |
| Wits appraisal (mm) | Distance between perpendicular projections of Points A and B on the functional occlusal plane (plane drawn through points of occlusal contact between the first permanent molars and the first and second premolars) |
| Facial pattern | |
| FMA (°) | Frankfort mandibular plane angle |
| SN.GoGn (°) | SN to GoGn angle |
| SN.PP (°) | SN to palatal plane angle |
| SN.OP (°) | SN to functional occlusal plane angle |
| LAFH (mm) | Lower anterior face height: distance from anterior nasal spine (ANS) to menton |
| Maxillary dentoalveolar component | |
| Mx1.PP (°) | Maxillary incisor long axis to palatal plane angle |
| Mx1-PP (mm) | Perpendicular distance between incisal edge of maxillary central incisor and palatal plane |
| Mx1-ANSperp (mm) | Perpendicular distance between incisal edge of maxillary central incisor and ANSperp (line perpendicular to palatal plane, passing through ANS) |
| Mx6-PP (mm) | Perpendicular distance between mesial cusp of maxillary first molar and palatal plane |
| Mandibular dentoalveolar component | |
| IMPA (°) | Incisor mandibular plane angle |
| Md1-MP (mm) | Perpendicular distance between incisal edge of mandibular incisor and mandibular plane |
| Md1-Pogperp (mm) | Perpendicular distance between incisal edge of mandibular central incisor and Pogperp (line perpendicular to mandibular plane, passing through pogonion) |
| Md6-MP (mm) | Perpendicular distance between mesial cusp of mandibular first molar and mandibular plane |
| Dental relationships | |
| Overbite (mm) | Distance between incisal edges of maxillary and mandibular central incisors, perpendicular to functional occlusal plane (magnified in the Fig) |
| Overjet (mm) | Distance between incisal edges of maxillary and mandibular central incisors, parallel to functional occlusal plane |
Twenty-nine of the 117 cephalometric radiographs were randomly selected, retraced, and redigitized by the same examiner. The first and second cephalometric measurements were used to calculate casual and systematic errors. Casual errors were calculated according to Dahlberg’s formula (Se 2 = Σd 2 /2n). The systematic errors were evaluated with dependent t tests at P <0.05.
Statistical analyses
To compare the whole sample with the subgroups at T1, T2, and T3, dependent ANOVA and Tukey tests were used.
Complementarily, overbite behavior in the long-term posttreatment period was compared in the Class I-II subgroup between the different surgical protocols with ANOVA and Tukey tests; for comparisons between wire fixation and RIF, and between RME and no RME, t tests were used.
In the subgroups, Pearson correlation coefficients were calculated between anterior overbite changes in the long-term posttreatment period and the following variables: initial age, initial severity of the open bite, initial mandibular plane angle, initial facial height, overbite changes immediately after orthodontic-surgical treatment, and long-term posttreatment changes in all cephalometric variables.
A clinically significant open-bite relapse was defined as a negative overbite between the maxillary and mandibular incisors at T3. Therefore, to establish a clinical parameter for the probability of open-bite correction stability, the percentages of patients with and without clinically significant relapses were calculated from the total number of patients and from each subgroup. Statistical analyses were performed with software (version 6.0, Statistica for Windows, Statsoft, Tulsa, Okla). The results were considered statistically significant at P <0.05.
Results
Only 1 (MS-PP) of the 25 cephalometric variables had a statistically significant systematic error. Ten variables had casual errors less than 1 mm or 1°, and 12 had errors less than 2 mm or 2°. Only 3 variables had casual errors greater than 2 mm or 2°.
The results are shown in Tables II through VII. Overbite relapse in the long-term posttreatment period was statistically significant in the whole sample and the Class I-II subgroup, but not in the Class III subgroup ( Tables II-IV ).
| Variable | Initial (T1) n = 39 Mean DP |
Final (T2) n = 39 Mean DP |
Follow-up (T3) n = 39 Mean DP |
P |
|---|---|---|---|---|
| Maxillary component | ||||
| SNA (°) | 80.84 (3.88) A | 82.44 (4.58) B | 83.78 (4.59) B | 0.000 ∗ |
| Co-A (mm) | 84.46 (4.02) A | 87.51 (5.30) B | 89.39 (6.11) C | 0.000 ∗ |
| A-Nperp (mm) | −1.81 (4.25) A | −0.19 (4.51) B | 0.55 (4.25) B | 0.001 ∗ |
| Mandibular component | ||||
| SNB (°) | 78.25 (5.43) A | 79.58 (4.92) B | 79.89 (5.08) B | 0.000 ∗ |
| Co-Gn (mm) | 114.93 (8.46) A | 119.05 (8.57) B | 120.81 (8.87) B | 0.000 ∗ |
| P-Nperp (mm) | −7.95 (10.88) A | −3.41 (9.43) B | −3.98 (10.54) B | 0.000 ∗ |
| Go-Gn (mm) | 73.43 (6.20) A | 76.59 (6.11) B | 77.57 (5.52) B | 0.000 ∗ |
| Co-Go (mm) | 52.52 (4.98) A | 53.46 (5.90) A | 54.30 (7.50) A | 0.069 |
| Maxillomandibular relationship | ||||
| ANB (°) | 2.59 (5.30) A | 2.87 (4.04) A,B | 3.89 (4.79) B | 0.028 ∗ |
| Wits appraisal (mm) | −0.51 (7.47) A | −0.90 (4.12) A | 0.15 (4.90) A | 0.411 |
| Facial pattern | ||||
| FMA (°) | 33.52 (5.70) A | 31.73 (5.47) B | 32.32 (6.64) A,B | 0.042 ∗ |
| SN.GoGn (°) | 38.63 (5.65) A | 36.92 (5.91) B | 36.76 (7.02) B | 0.006 ∗ |
| SN.PP (°) | 9.21 (3.39) A | 10.00 (4.53) A | 9.00 (3.99) A | 0.143 |
| SN.OP (°) | 15.73 (16.98) A | 20.04 (11.47) A | 20.69 (7.66) A | 0.085 |
| LAFH (mm) | 71.13 (7.50) A,B | 70.45 (7.91) A | 72.75 (8.59) B | 0.009 ∗ |
| Maxillary dentoalveolar component | ||||
| Mx1.PP (°) | 118.29 (6.92) A | 114.69 (8.22) B | 115.61 (9.13) B | 0.002 ∗ |
| Mx1-PP (mm) | 27.08 (3.84) A | 28.65 (3.83) B | 29.15 (4.83) B | 0.000 ∗ |
| Mx1-ANSperp (mm) | 0.26 (3.68) A | −0.64 (3.84) A,B | −1.19 (3.67) B | 0.047 ∗ |
| Mx6-PP (mm) | 25.33 (2.88) A | 25.53 (2.79) A,B | 26.24 (3.18) B | 0.039 ∗ |
| Mandibular dentoalveolar component | ||||
| IMPA (°) | 86.41 (8.96) A | 84.24 (8.90) A | 86.07 (8.31) A | 0.107 |
| Md1-MP (mm) | 39.54 (4.33) A | 41.35 (4.65) B | 42.10 (4.68) B | 0.000 ∗ |
| Md1-Pogperp (mm) | −12.05 (4.78) A | −14.36 (4.54) B | −13.66 (4.69) B | 0.000 ∗ |
| Md6-MP (mm) | 31.28 (3.91) A | 31.57 (4.36) A,B | 32.52 (4.68) B | 0.038 ∗ |
| Dental relationships | ||||
| Overbite (mm) | −4.25 (2.03) A | 1.10 (0.82) B | −0.04 (1.81) C | 0.000 ∗ |
| Overjet (mm) | 3.71 (4.84) A | 2.51 (0.65) A | 2.72 (1.96) A | 0.137 |
| Variable | Initial (T1) n = 23 Mean DP |
Final (T2) n = 23 Mean DP |
Follow-up (T3) n = 23 Mean DP |
P |
|---|---|---|---|---|
| Maxillary component | ||||
| SNA (°) | 81.29 (3.11) A | 82.21 (4.49) A | 84.11 (4.59) B | 0.000 ∗ |
| Co-A (mm) | 84.97 (4.91) A | 87.78 (6.28) B | 90.67 (7.22) C | 0.000 ∗ |
| A-Nperp (mm) | −1.05 (3.75) A | −0.18 (4.14) A,B | 1.12 (4.26) B | 0.026 ∗ |
| Mandibular component | ||||
| SNB (°) | 75.24 (3.94) A | 77.27 (4.19) B | 77.40 (4.44) B | 0.000 ∗ |
| Co-Gn (mm) | 111.04 (7.71) A | 117.08 (9.45) B | 119.17 (9.58) B | 0.000 ∗ |
| P-Nperp (mm) | −13.69 (9.21) A | −8.03 (8.23) B | −9.33 (9.83) B | 0.000 ∗ |
| Go-Gn (mm) | 70.86 (5.26) A | 75.42 (5.97) B | 77.59 (5.37) C | 0.000 ∗ |
| Co-Go (mm) | 51.23 (5.05) A | 52.43 (6.97) A | 52.24 (8.37) A | 0.506 |
| Maxillomandibular relationship | ||||
| ANB (°) | 6.06 (3.03) A,B | 4.95 (3.27) A | 6.73 (3.48) B | 0.024 ∗ |
| Wits appraisal (mm) | 4.84 (3.78) A | 1.26 (3.25) B | 2.85 (4.16) A,B | 0.000 ∗ |
| Facial pattern | ||||
| FMA (°) | 35.42 (5.71) A | 33.91 (5.43) A | 35.41 (6.27) A | 0.276 |
| SN.GoGn (°) | 40.83 (5.25) A | 39.37 (5.59) A | 40.03 (6.57) A | 0.329 |
| SN.PP (°) | 9.07 (2.96) A | 10.81 (4.53) B | 9.33 (4.77) A,B | 0.028 ∗ |
| SN.OP (°) | 22.83 (11.69) A | 20.65 (12.49) A | 21.87 (8.93) A | 0.711 |
| LAFH (mm) | 72.82 (7.79) A | 72.71 (7.42) A | 76.02 (7.51) B | 0.004 ∗ |
| Maxillary dentoalveolar component | ||||
| Mx1.PP (°) | 116.78 (5.42) A | 111.97 (7.44) B | 112.67 (8.86) B | 0.000 ∗ |
| Mx1-PP (mm) | 27.95 (3.71) A | 29.94 (3.58) B | 30.78 (4.73) B | 0.001 ∗ |
| Mx1-ANSperp (mm) | 0.69 (3.59) A | −0.82 (3.93) A,B | −2.07 (3.40) B | 0.002 ∗ |
| Mx6-PP (mm) | 26.07 (3.14) A | 26.26 (3.02) A | 26.98 (3.15) A | 0.232 |
| Mandibular dentoalveolar component | ||||
| IMPA (°) | 91.10 (6.45) A | 89.53 (6.22) A | 90.86 (5.70) A | 0.558 |
| Md1-MP (mm) | 41.07 (4.29) A | 43.31 (4.07) B | 44.18 (4.17) B | 0.008 ∗ |
| Md1-Pogperp (mm) | −10.10 (4.09) A | −12.18 (2.87) B | −11.58 (3.69) B | 0.008 ∗ |
| Md6-MP (mm) | 32.25 (4.51) A | 33.33 (3.79) A,B | 34.53 (4.37) B | 0.005 ∗ |
| Dental relationships | ||||
| Overbite (mm) | −4.59 (2.29) A | 1.08 (0.87) B | −0.60 (2.12) C | 0.000 ∗ |
| Overjet (mm) | 5.90 (3.00) A | 2.49 (0.59) B | 3.20 (2.41) B | 0.000 ∗ |
| Variable | Initial (T1) n = 16 Mean DP |
Final (T2) n = 16 Mean DP |
Follow-up (T3) n = 16 Mean DP |
P |
|---|---|---|---|---|
| Maxillary component | ||||
| SNA (°) | 80.19 (4.81) A | 82.76 (4.83) B | 83.29 (4.69) B | 0.004 ∗ |
| Co-A (mm) | 83.71 (2.17) A | 87.11 (3.62) B | 87.56 (3.48) B | 0.001 ∗ |
| A-Nperp (mm) | −2.90 (4.79) A | −0.21 (5.13) B | −0.26 (4.24) A,B | 0.028 ∗ |
| Mandibular component | ||||
| SNB (°) | 82.59 (4.25) A | 82.90 (3.95) A | 83.48 (3.62) A | 0.297 |
| Co-Gn (mm) | 120.52 (6.13) A | 121.88 (6.34) A | 123.17 (7.37) A | 0.074 |
| P-Nperp (mm) | 0.30 (7.22) A | 3.24 (6.81) A,B | 3.71 (5.73) B | 0.032 ∗ |
| Go-Gn (mm) | 77.12 (5.65) A | 78.27 (6.10) A | 77.56 (5.89) A | 0.546 |
| Co-Go (mm) | 54.38 (4.37) A | 54.94 (3.59) A | 57.27 (4.90) B | 0.009 ∗ |
| Maxillomandibular relationship | ||||
| ANB (°) | −2.39 (3.57) A | −0.13 (3.06) B | −0.18 (3.21) B | 0.004 ∗ |
| Wits appraisal (mm) | −8.20 (3.68) A | −3.99 (3.19) B | −3.72 (2.87) B | 0.000 ∗ |
| Facial pattern | ||||
| FMA (°) | 30.78 (4.57) A | 28.59 (3.84) B | 27.86 (4.26) B | 0.001 ∗ |
| SN.GoGn (°) | 35.48 (4.76) A | 33.40 (4.48) B | 32.04 (4.62) B | 0.000 ∗ |
| SN.PP (°) | 9.42 (4.03) A | 8.82 (4.39) A | 8.52 (2.53) A | 0.528 |
| SN.OP (°) | 5.53 (18.49) A | 19.17 (10.15) B | 18.98 (5.13) B | 0.001 ∗ |
| LAFH (mm) | 68.69 (6.55) A | 67.20 (7.66) A | 68.06 (8.04) A | 0.277 |
| Maxillary dentoalveolar component | ||||
| Mx1.PP (°) | 120.46 (8.35) A | 118.60 (7.88) A | 119.84 (7.98) A | 0.528 |
| Mx1-PP (mm) | 25.82 (3.79) A | 26.78 (3.46) A | 26.80 (4.04) A | 0.192 |
| Mx1-ANSperp (mm) | −0.35 (3.83) A | −0.38 (3.81) A | 0.06 (3.79) A | 0.847 |
| Mx6-PP (mm) | 24.27 (2.11) A | 24.47 (2.08) A | 25.16 (2.99) A | 0.112 |
| Mandibular dentoalveolar component | ||||
| IMPA (°) | 79.67 (7.76) A | 76.62 (6.23) A | 79.19 (6.44) A | 0.106 |
| Md1-MP (mm) | 37.34 (3.41) A | 38.54 (4.01) B | 39.11 (3.70) B | 0.003 ∗ |
| Md1-Pogperp (mm) | −14.86 (4.38) A | −17.51 (4.73) B | −16.64 (4.43) A,B | 0.010 ∗ |
| Md6-MP (mm) | 29.89 (2.31) A | 29.03 (3.93) A | 29.62 (3.53) A | 0.439 |
| Dental relationships | ||||
| Overbite (mm) | −3.76 (1.51) A | 1.13 (0.79) B | 0.77 (0.74) B | 0.000 ∗ |
| Overjet (mm) | −0.91 (2.36) A | 2.53 (0.74) B | 2.04 (0.64) B | 0.000 ∗ |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


