This article reports the successful treatment using miniscrew anchorage of an adult patient with a severe deep overbite and a unilateral scissors-bite. A 23-year-old woman had chief complaints of maxillary incisal crowding and difficulty chewing. She was diagnosed with a severe Class II Division 2 malocclusion with anterior crowding and a unilateral scissors-bite caused by buccal elongation of the maxillary left second molar. The maxillary first premolars were extracted, and 3 miniscrews were implanted as skeletal anchorage to resolve the functional and esthetic problems. The total active treatment period was 41 months. As a result of the implant-anchored orthodontic treatment, both the patient’s facial profile and occlusion significantly improved. The asymmetric movements of the incisor paths and bilateral condyles during lateral excursions disappeared. The satisfactory facial profile and resultant occlusion were maintained throughout a 49-month retention period. The patient was satisfied with the treatment results.
Successfully treating a severe deep overbite remains a major challenge for orthodontists. Many aspects must be factored in during deep overbite correction, including esthetics, lip competence, vertical skeletal dimensions, and long-term stability of the final occlusion. Deep overbite correction can be achieved with molar extrusion, incisor intrusion, or a combination of both, depending on the diagnosis and treatment objectives. However, molar extrusion is not recommended in adult patients because the masticatory muscles and altered occlusion might move the extruded molars back to their original positions. Therefore, incisor intrusion is generally the preferred treatment in adults with an excessive overbite, which often requires strict anchorage control.
Scissors-bite is a common dental feature of Class II Division 2 patients with a broad and forward maxilla relative to the mandible. Conventional treatment mechanics cannot offer a solution to correct severe transverse discrepancies, especially in adult patients, due to their limitations. Consequently, patients with a severe scissors-bite are sometimes managed with surgical orthodontic correction. Several treatment procedures have also been proposed as nonsurgical options for correcting a simple posterior scissors-bite, including intermaxillary cross-elastic appliances, edgewise appliances, transpalatal arch appliances with intramaxillary elastics, and lingual arch appliances with intramaxillary elastics. However, these elastic methods generate extrusive forces on the anchorage teeth in both jaws and possibly induce undesirable decreases in the overbite, clockwise rotation of the mandible, and premature contact. In addition, obtaining good treatment results with intermaxillary elastics also depends on the patient’s cooperation.
In the past decade, implant-anchored orthodontics has been generalized, and various types of tooth movement can now be achieved without active patient cooperation, indicating that effective correction can be obtained without undesirable side effects. Most importantly, implant anchorage is effective for achieving absolute intrusion of both incisors and molars, which cannot be completed with traditional orthodontic mechanics. This suggests the possible usefulness of implant anchorage for correcting deep overbites and posterior scissors-bites. However, the long-term stability of implant-anchored orthodontics in adults with Class II Division 2 malocclusion and molar scissors-bite remains unknown.
Furthermore, some investigators have suggested that 3-dimensional occlusal disharmonies, such as a Class II Division 2 and scissors-bite malocclusion, might result in functional disturbances of the temporomandibular joint. Nonetheless, the longitudinal assessments of the jaw function described in some reports have demonstrated that the comprehensive effects of orthodontic treatment on the stomatognathic function remain unclear.
Here, we report the successful treatment of an adult patient with a Class II Division 2 malocclusion and a unilateral scissors-bite caused by buccal inclination and overeruption of the maxillary left second molar using miniscrew anchorage. Additionally, this case report provides a functional assessment of the outcome of the orthodontic treatment. We assessed the patient’s stomatognathic function, condylar motion, and jaw movement to evaluate the gnathologic changes after orthodontic treatment.
Diagnosis and etiology
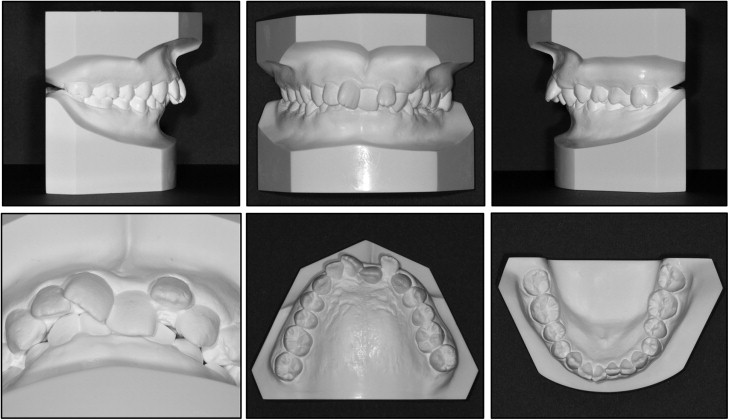
A woman, age 23 years 0 months, came to the outpatient dental clinic of Okayama University Hospital in Japan. Her chief complaints were crooked teeth and difficulty chewing ( Figs 1-3 ). Facial photographs showed a symmetrical face, a convex profile, an acute nasolabial angle, and a proportionally short lower anterior facial height ( Fig 1 ). Severe crowding was observed in the maxillary incisors, and the maxillary left central incisor was significantly retroclined with a reduced overjet (1.9 mm). Deep overbite (7.2 mm) and Angle Class II molar relationships on both sides were also observed, and the edges of the mandibular incisor palatally occluded with the cingulum plateau of the maxillary incisors. In addition, an excessive curve of Spee of 4.0 mm was found in the mandibular dentition. The patient also had a scissors-bite on the left side and buccal elongation of the maxillary left second molar ( Figs 1 and 2 ). The maxillary dental midline almost coincided with the facial midline and the mandibular dental midline.

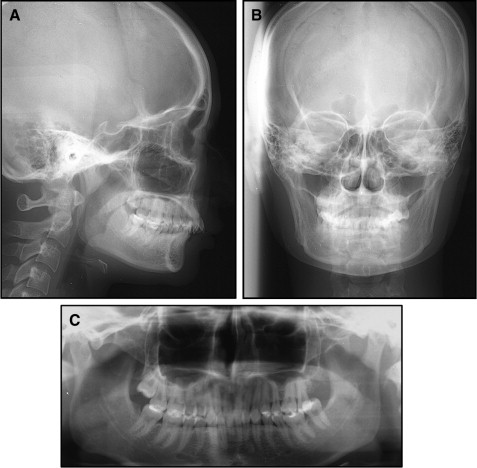
In comparison with Japanese norms, the cephalometric analysis of the patient showed a skeletal Class I jaw relationship (ANB, 3.5°), a low mandibular plane angle (Mp-SN, 17.5°), a decreased gonial angle (106°), and a short anterior lower facial height (Me/PP, 57.0 mm) ( Table I ). The maxillary left central incisor was lingually inclined (U1-SN, 89°), and the maxillary right central incisor was labially inclined (U1-SN, 113.5°).
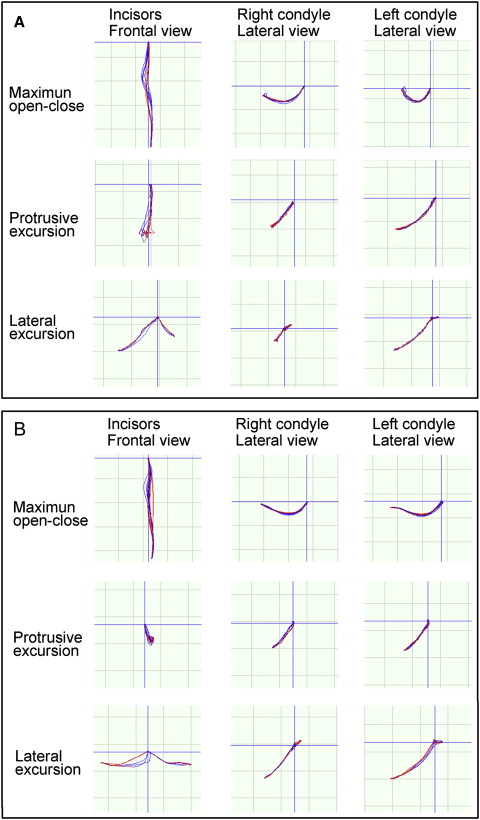
An optoelectronic jaw-tracking system (Gnathohexagraph system, version 1.31; Ono Sokki, Kanagawa, Japan) was used to record the patient’s jaw movements with 6 degrees of freedom. The masticatory jaw-movement pattern showed lopsided chewing on the right side ( Table II ). Asymmetrical movements of the incisal path and the bilateral condyles were observed during lateral excursion jaw movements because of a unilateral scissors-bite ( Fig 4 , A ).
| Variable | Japanese norms (women) | SD | Pretreatment | Posttreatment | Postretention |
|---|---|---|---|---|---|
| Angular (°) | |||||
| ANB | 2.8 | 2.44 | 3.5 | 3.5 | 3.5 |
| SNA | 80.8 | 3.61 | 83.0 | 83.0 | 83.0 |
| SNB | 77.9 | 4.54 | 79.5 | 79.5 | 79.5 |
| FMA | 30.5 | 3.60 | 11.0 | 11.0 | 11.0 |
| Mp-SN | 37.1 | 4.64 | 17.5 | 17.5 | 17.5 |
| U1-SN | 105.9 | 8.79 | 89.0 (113.5) | 107.0 | 105.5 |
| L1-Mp | 93.4 | 6.77 | 99.0 | 108.0 | 107.5 |
| Interincisal angle | 123.6 | 10.64 | 154.0 (130.0) | 127.0 | 129.0 |
| Occlusal plane to SN | 18.0 | 3.50 | 8.0 | 10.0 | 10.0 |
| Gonial angle | 122.2 | 5.29 | 106.0 | 106.0 | 106.0 |
| Linear (mm) | |||||
| S-N | 67.9 | 3.65 | 69.5 | 69.5 | 69.5 |
| N-Me | 125.8 | 5.04 | 111.0 | 111.0 | 111.0 |
| Me/PP | 68.6 | 3.71 | 57.0 | 57.0 | 57.0 |
| Overjet | 3.1 | 1.07 | 1.9 (7.8) | 2.5 | 2.3 |
| Overbite | 3.3 | 1.89 | 7.2 | 1.5 | 2.8 |
| U1/PP | 31.0 | 2.34 | 26.0 (24.0) | 23.0 | 24.0 |
| U6/PP | 24.6 | 2.00 | 21.5 | 21.0 | 21.0 |
| L1/Mp | 44.2 | 2.68 | 41.0 | 37.0 | 37.0 |
| L6/Mp | 32.9 | 2.50 | 31.5 | 32.5 | 32.5 |
| L1/AP | 5.5 | 3.00 | −2.0 | 0.0 | 0.0 |
| E-line to upper lip | −2.5 | 1.90 | 3.5 | 0.0 | 0.0 |
| E-line to lower lip | 0.9 | 1.90 | 0.5 | −3.5 | −3.5 |
| Occlusal force (N) | Occlusal contact area (mm 2 ) | Free mastication (%) | |
|---|---|---|---|
| Pretreatment | 989 | 31.6 | Rt, 89.9 Lt, 10.1 |
| Posttreatment | 1037 | 25.3 | Rt, 68.7 Lt, 31.3 |
| Posttretention | 1121 | 27.8 | — |
Treatment objectives
Based on these findings, the patient was diagnosed with an Angle Class II Division 2 malocclusion, a skeletal Class I jaw-base relationship, lip protrusion, moderate anterior tooth crowding, and a unilateral scissors-bite on the left side. The treatment objectives were to correct the lip protrusion and incisor crowding, obtain a good facial profile, create more ideal overbite and overjet relationships with good functional Class I canine and Class II molar relationships, and eliminate the scissors-bite. We planned to extract the maxillary first premolars and use miniscrews for skeletal anchorage to achieve the treatment objectives. Simultaneously, the overerupted maxillary left second molar was moved lingually with the intrusive force of a miniscrew.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


