We successfully treated a patient with achondroplasia with conventional orthodontic techniques. It was followed by long-term retention. The patient, a 12-year-old boy, had chief complaints of occlusal disturbance and mandibular protrusion. He had been diagnosed with achondroplasia and had growth hormone treatment in his early teenage years. His facial profile was concave with a bulging forehead and a retrognathic maxilla. It was characterized by a skeletal Class III jaw-base relationship with a retropositioned maxilla. At the age of 12 years 9 months, maxillary protraction was initiated with a reverse headgear; for 2 years 6 months, the maxillomandibular growth was controlled. After the growth spurt, at the age of 15 years 6 months, leveling and alignment of both dental arches were started with preadjusted edgewise appliances. After 83 months of multibracket treatment, an acceptable occlusion with a Class I molar relationship and an adequate interincisal relationship was achieved, despite the simultaneous marked vertical growth of the mandible. The resultant occlusion was stable during a 6-year retention period, although considerable forward-downward mandibular growth was observed. Conclusively, our results indicated the necessity of long-term observation in this patient with achondroplasia, especially because of the persistent mandibular growth.
Highlights
- •
We successfully treated a patient with achondroplasia.
- •
Conventional orthodontic techniques produced an acceptable occlusion.
- •
Forward-downward mandibular growth was observed during retention.
- •
Results were stable at 6 years posttreatment.
- •
Long-term observation is needed in achondroplasia patients due to mandibular growth.
Achondroplasia is the most common form of dwarfism. The disease is inherited as an autosomal dominant trait that occurs in about 1 in 26,000 persons. About 90% of the cases are caused by new mutations. Previous genetic investigations have indicated that the congenital defect factor receptor FGFR3 is responsible for the abnormal membranous ossification in achondroplasia. It is known that recurrent mutations of 1 amino acid in the transmembrane domain of the FGFR3 protein are the culprits. The mutations have been reported to cause aberrant proliferation and differentiation of chondrocytes, resulting in inhibition of endochondral ossification in growth plates. Manifestations of achondroplasia include short stature caused by rhizomelic shortening of the limbs, exaggerated lumbar lordosis, and craniofacial malformations. The latter include a short cranial base with early spheno-occipital closure and megalocephaly. Failure of normal cartilage proliferation leads not only to the characteristically short arms and legs, but also to underdevelopment of the midface because the maxilla is not translated forward by normal lengthening of the cranial base. The resulting orofacial characteristics include maxillary skeletal retrognathia and malformed teeth. The cephalometric characteristics of achondroplasia are an enlarged calvaria with hydrocephaly and frontal bossing, a short posterior cranial base, a retrognathic maxilla, a normal mandible, and protrusive maxillary incisors.
A few patients with achondroplasia have been treated with conventional orthodontics and orthognathic surgery if necessary. However, there are few detailed reports of long-term observations during the complete orthodontic treatment of these patients. Therefore, the prognosis of conventional orthodontic treatment performed in their pubertal growth period is still unclear.
The purpose of this article was to present a patient with achondroplasia and an Angle Class III malocclusion, and a skeletal Class III jaw-base relationship with deficient growth of the maxilla treated with conventional orthodontic techniques and followed for long-term retention.
Diagnosis and etiology
The patient, a 12-year-old boy, had chief complaints of occlusal disturbance and mandibular protrusion. At birth, he had been diagnosed with achondroplasia and accordingly had been receiving growth hormone treatment for 5 years at the Department of Pediatrics, Tokushima University Hospital in Tokushima, Japan. At his first visit to the orthodontic clinic, he was 115 cm tall, which was less than −5 SD of Japanese male standards.
The patient’s facial profile was concave with a bulging forehead and a retrognathic maxilla. His nose was saddle-shaped because of underdevelopment of the nasomaxillary complex. Anterior crossbites were observed at the maxillary right central and lateral incisors and left lateral incisor and canine, and the molar relationship was bilaterally Angle Class III. Overbite was −1.5 mm, indicating an anterior open bite. The maxillary dental midline was deviated 6.5 mm to the left toward the facial midline ( Figs 1 and 2 ). No signs and symptoms of temporomandibular joint disorders were observed. The patient exhibited a tongue-thrust swallowing pattern.

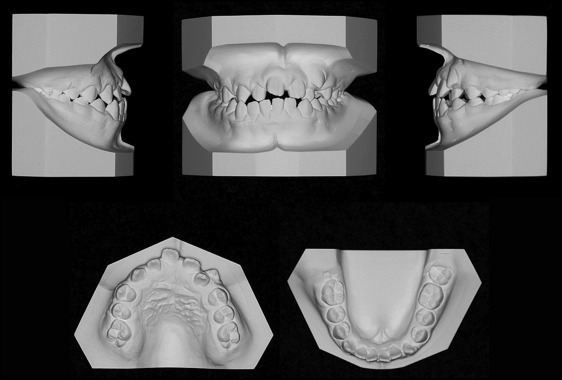
Model analysis showed a larger maxillary coronal arch length and a smaller maxillary basal arch length compared with Japanese male norms.
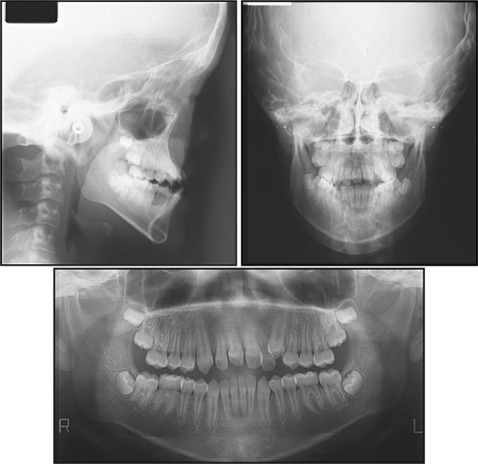
A panoramic radiograph showed the 4 third molar buds. The cephalometric analysis, when compared with the Japanese norms, showed a skeletal Class III jaw-base relationship (ANB, −8.0°) with a retropositioned maxilla (SNA, 62.5°). The length of the anterior cranial base (S-N) was more than 5 SD greater than the norm, indicating enlargement of the head. The mandibular plane angle was within the normal range (FMA, 28.5°). The maxillary incisors were labially inclined (U1-SN, 125.1°), and the mandibular incisors had a lingual inclination (L1-MP, 87.6°) ( Fig 3 ; Table ).
| Variable | Mean for Japanese males ∗ | Pretreatment | After phase 1 | Posttreatment | Postretention | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| 12 y | SD | 14 y | SD | Adult | SD | 12 y 9 mo | 15 y 6 mo | 22 y 4 mo | 28 y 7 mo | |
| Angle (°) | ||||||||||
| ANB | 4.3 | 2.2 | 3.7 | 2.3 | 3.2 | 2.4 | −8.0 | −6.0 | −5.3 | −6.5 |
| SNA | 81.6 | 3.4 | 81.9 | 3.6 | 81.5 | 3.3 | 62.5 | 64.0 | 64.3 | 64.3 |
| SNB | 77.2 | 3.7 | 78.1 | 4.1 | 78.2 | 4.0 | 70.5 | 69.9 | 69.6 | 70.8 |
| FMA | 30.6 | 5.1 | 29.2 | 5.8 | 28.0 | 6.1 | 28.5 | 28.7 | 29.2 | 28.3 |
| Gonial angle | 125.0 | 5.9 | 123.3 | 6.6 | 120.9 | 6.5 | 121.1 | 119.6 | 119.3 | 119.9 |
| U1-SN | 105.0 | 7.1 | 106.6 | 8.5 | 106.0 | 7.5 | 125.1 | 120.8 | 99.2 | 102.8 |
| L1-MP | 95.7 | 5.4 | 96.7 | 6.0 | 95.2 | 6.2 | 87.6 | 83.7 | 75.2 | 76.8 |
| Convexity | 170.3 | 5.1 | 171.9 | 5.3 | 173.2 | 5.5 | 197.2 | 192.5 | 192.0 | 194.0 |
| Interincisal angle | 122.2 | 8.8 | 120.8 | 8.9 | 124.2 | 8.6 | 107.3 | 114.3 | 143.5 | 139.0 |
| Occlusal plane | 17.9 | 3.2 | 16.1 | 3.3 | 15.5 | 4.2 | 15.9 | 13.5 | 13.7 | 12.8 |
| Linear (mm) | ||||||||||
| S-N | 68.5 | 2.8 | 70.8 | 3.2 | 72.2 | 3.3 | 83.4 | 85.1 | 87.7 | 87.7 |
| S-Ar | 18.1 | 2.5 | 19.3 | 3.0 | 20.0 | 2.5 | 8.9 | 9.3 | 10.3 | 10.7 |
| N-Me | 123.4 | 4.7 | 130.5 | 4.7 | 135.7 | 4.0 | 129.9 | 139.8 | 158.1 | 160.0 |
| N/PP | 55.3 | 2.4 | 58.4 | 2.5 | 60.0 | 1.8 | 48.0 | 50.4 | 54.6 | 55.2 |
| Me/PP | 66.6 | 3.3 | 71.0 | 3.4 | 74.6 | 3.0 | 72.9 | 80.0 | 94.2 | 96.2 |
| Ptm-A/PP | 49.0 | 2.9 | 50.6 | 3.2 | 51.7 | 3.8 | 40.2 | 42.7 | 43.6 | 43.6 |
| Ptm-ANS/PP | 53.2 | 2.7 | 55.0 | 3.0 | 56.4 | 3.4 | 42.9 | 45.3 | 45.9 | 45.9 |
| Ar-Go | 44.9 | 3.7 | 49.3 | 4.9 | 53.2 | 5.7 | 47.1 | 52.0 | 65.4 | 67.5 |
| Ar-Me | 103.4 | 5.9 | 110.5 | 6.8 | 115.6 | 6.8 | 101.3 | 109.6 | 123.9 | 126.7 |
| Go-Me | 69.1 | 4.4 | 73.3 | 5.1 | 76.6 | 4.4 | 65.4 | 70.7 | 74.5 | 75.1 |
| Overjet | 3.4 | 1.2 | 3.0 | 1.3 | 3.3 | 1.0 | 3.0 | 4.7 | 1.6 | 1.6 |
| Overbite | 3.5 | 1.5 | 3.0 | 1.6 | 3.3 | 1.7 | −1.5 | −1.5 | 1.8 | 1.5 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


