Fig. 8.1
Example of a BRONJ defect in the lower right jaw with a persistent exposed alveolus (left). The mucosal flap is designed in a trapezoid manner, and the decortication and debridement are performed (middle). After periosteal incision, the mucosal flap is sutured into the defect (right)
Buccal Mucosal Flap
The buccal mucosal flap is also a very versatile axial- or random-pattern flap with a much greater and better flexibility than the palatal flap [22–24]. Palatal bone is exposed in the palatal flap technique which is counterproductive in a patient with MRONJ and BRONJ. Therefore, the palatal flap is not indicated, but the buccal mucosal flap can be useful in small defects [24].
This flap can be based on the anterior or posterior part of the buccal mucosa, incorporating the buccal branch of the facial artery with some parts of the buccinator muscle if necessary [22–24]. The mucosa is incised including underlying glandular tissue, but the parotid duct should be preserved [22]. As mentioned above, parts of the buccinator muscle can be integrated as an axial-pattern flap if necessary [22, 23]. We prefer anteriorly based buccal mucosal flaps for defects in the incisional area of the alveolar crest and posteriorly based flaps for defects in the premolar or molar area.
Buccal Fat Pad Flap
The buccal fat pad flap is one of the most reliable flaps in the management of BRONJ in the upper jaw, as this flap offers additional tissue to cover mucosal defects [25, 26]. The exposed fat rapidly mucosalizes by epithelial seeding. The buccal fat pad is located in the cheek and surrounded by a thin capsule [27, 28]. The fat pad consists of four parts in the buccal, temporal, pterygoidal, and pterygopalatine area. The central and buccal parts are the most reliable and can easily be used for additional coverage especially in the upper but also in the lower jaw if necessary [27, 28]. The vascular supply of this flap is provided by small branches arising from the maxillary, facial, and superficial temporal artery [27, 28] entering the deep surface of the fat pad. This flap can be exposed and mobilized easily by incising the periosteum underlying a buccal mucoperiosteal flap [27, 28]. This flap can be combined with a standard mucosal flap (Fig. 8.2).
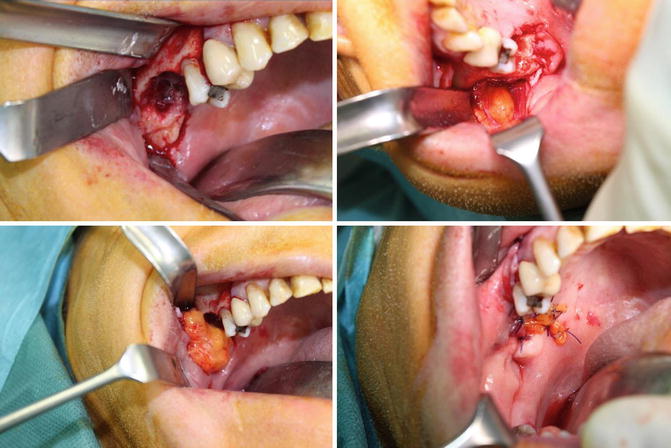
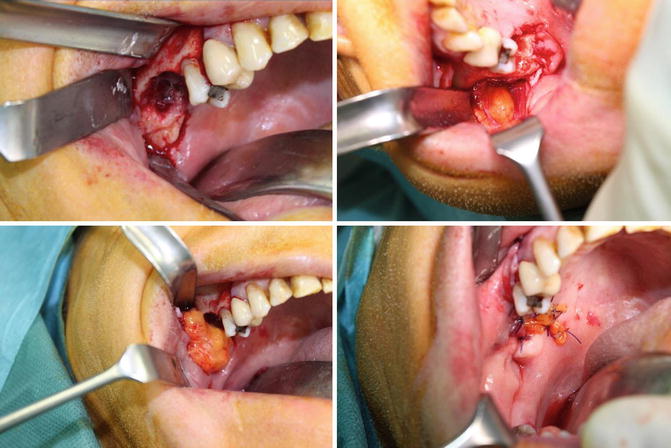
Fig. 8.2
Example of a BRONJ defect in the upper right jaw with exposure of the maxillary sinus (upper left). The buccal fat pad flap can be exposed at the pterygopalatine line (upper right). After careful mobilization (lower left), the buccal fat pad flap is sutured into the defect and covered by an additional mucosal flap (lower right)
Mylohyoid Flap
The mylohyoid flap can be used if the lingual part of the mandible is affected. In such cases mucosal flaps are not best suited due to the tension of the floor of the mouth as well as the alveolar crest and the vestibular mucosa [29]. Especially in cases of relapsing BRONJ at this site, the mylohyoid muscle flap can be used for defect coverage in the same manner as the buccal fat pad flap for additional coverage of the bone [4]. The mylohyoid flap is a myofascial flap which is accessible at the lingual border of the mandible, inserting at the mylohyoid line. The muscle is detached from here, mobilized and placed over the decorticated mandible with interrupted and tensionless sutures [29]. A mucosal flap should also be used, but is not essential due to the capacity of intraoral exposed muscle flaps to rapidly mucosalize albeit with fibrosis and scarring [30] (Fig. 8.3).
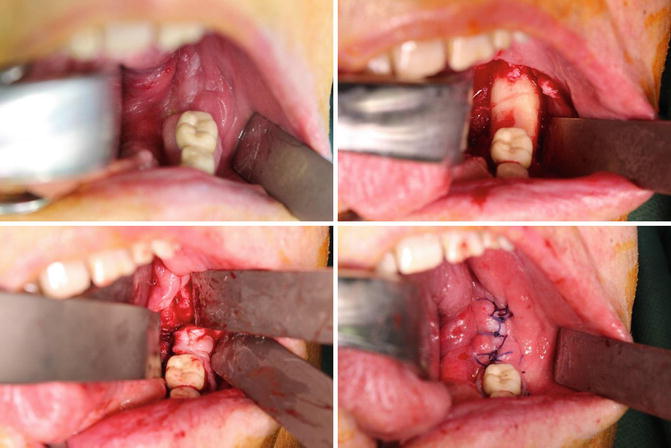
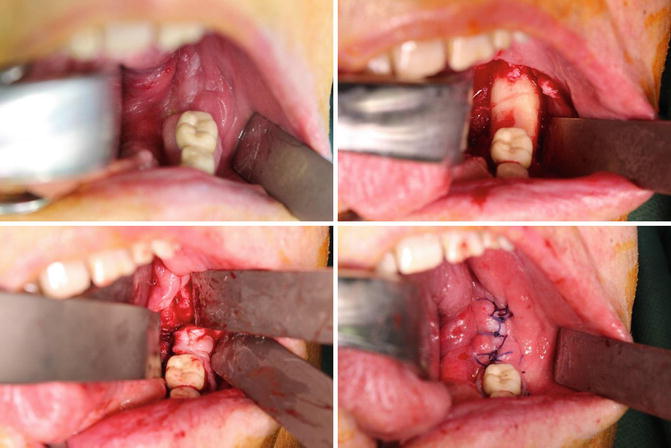
Fig. 8.3
Example of a BRONJ defect in the lower left jaw with exposure of the lingual part of the mandible (upper left). The mylohyoid muscle flap can be exposed at the mylohyoid line and mobilized (upper right). After careful fixation over the debrided mandible (lower left), this flap is covered by an additional mucosal flap (lower right)
Nasolabial Flap
The nasolabial flap is a random-pattern flap relying on the subdermal plexus of vessels arising from small branches of the facial artery and accompanying veins. While it can be raised on the facial vessels, this by definition disrupts the muscles of facial expression and is entirely unnecessary. This flap can be based on a cranial or caudal pedicle, although the caudally based type of this flap is more valuable for intraoral reconstruction [31]. The incision is outlined in the nasolabial fold and as far lateral as needed. The incision is through skin and subcutaneous fat [31, 32]. The distal part of the flap includes thin lower eyelid skin and the proximal thicker subcutaneous flap. The facial vessels are often seen in the deeper fat of the face and are not included in the flap itself. A tunnel is created just above this point through into the mouth. This is widened by blunt dissection and the distal end of the flap passed into the mouth for inset. Parrafin gauze is wrapped around the base of the pedicle to prevent it healing into the tunnel [31, 32]. The flap is limited by its axis of rotation and is not a good choice in the dentate patient. The donor site defect in the nasolabial fold is surprisingly easily closed directly in two layers [31, 32]. The singular disadvantage to this technique is the need to divide and inset the pedicle at 3 weeks necessitating a second operation, although the second stage can be performed under local anesthesia. With this type of flap, both defects of the upper and lower jaw can be covered [32, 33] (Fig. 8.4).


Fig. 8.4
Example of a nasolabial flap after planning (left). The flap is prepared (middle). After intraoral transposition, the flap is sutured into the defect (right)
Microvascular Free Flaps
Radial Forearm Flap
This reliable, common flap provides thin, pliable, and reliable skin from the forearm. The skin is hair bearing in many men. The flap design was first described in 1981 [34]. Before this flap can be raised, an Allen test should be performed to ensure the perfusion of the hand [35]. The flap raising is straightforward, but the microvascular anastomoses of the accompanying venae comitans might be more challenging in some patients due to their small diameter. Flap harvesting normally starts at the ulnar site of the forearm, raising a fasciocutaneous portion of the forearm being careful to leave the paratenon which creates a donor site of muscle and paratenon which readily accepts a split- or full-thickness skin graft. The radial artery and accompanying venae are identified at the most distal point of the flap, usually 2 cm proximal to the flexor crease (minimizing the tension on the repairing skin graft). These vessels should be ligated and then dissected after identifying the superficial branch of the radial nerve, which should be preserved. The flap can be raised with the cephalic vein and the lateral antebrachial cutaneous nerve of the forearm [34]. Neither is essential for success of the flap. The vascular pedicle lies between the flexor carpi radialis muscle and the brachioradialis muscle. The vascular bundle should be dissected from the deep septum (which carries perforating vessels to the radius in 40 % of which can be included creating an osteocutaneous flap) followed by ligation or even bipolar coagulation of the muscular perforators arising from the radial artery and its concomitant veins. The pedicle length can be dissected to the length dictated by the site of reconstruction and microvascular anastomosis. If necessary, the microanastomoses can also be performed at the contralateral neck of reconstruction if needed. The donor site should be closed by a full-thickness skin graft or a split-thickness skin graft [36].
Osteocutaneous Fibular Flap
Reconstruction with the fibular bone flap was first described by Taylor et al. in 1975 [37] and was modified by Chen and coworkers with an integrated skin paddle [38]. The skin paddle allows good defect coverage of the affected mucosa and makes this type of flap suitable in patients with extensive MRONJ. This flap is especially beneficial in cases with pathological fractures of the mandible requiring continuity resections and additional mucosal reconstruction [14, 15, 21].
The vessels of the lower leg should be assessed by magnetic resonance imaging or computed tomography combined with an angiographic visualization [39]. While it is extremely unlikely that the fibula will be a site of metastases of the primary disease, this should be excluded. It may be helpful to assess the perforator inserted into the skin paddle by a Doppler examination. The dissection starts with an incision along the fibular bone on the peroneus longus muscle 2 cm anterior to the intermuscular lateral septum. In the area of the anticipated perforator, the incision should be curved anterior to the line of the fibula. The subcutaneous tissue is dissected down to the muscular fascia and intermuscular septum to the peroneal muscles. The perforator vessels become visible in most cases. The lateral part of the fibular bone should be dissected, and the flexor hallucis muscle is dissected from the soleus muscle. The peroneal artery can be palpated behind the fibular bone and is carefully dissected. The distal osteotomy of the fibular bone should be performed 6–8 cm above the lateral malleolus. The proximal osteotomy should preserve a similar amount of fibular bone below the fibular head. The fibular bone is then mobilized by dissection of the intermuscular fascia and interosseous membrane. The guide to this part of the preparation is the tibialis posterior muscle with its v-shaped muscle bundles. The pedicle should be cut after ligation at the most distal part of the fibular bone. The skin paddle is then incised, but the intermuscular septum should be left intact as the perforators are located in this area. The pedicle is further dissected and the flap raised completely, then either detached and shaped on a side table or osteotomized to a preformed template on the leg while still perfused to allow reconstruction of the mandible and the soft tissue defect. The anastomosis can be performed to the standard vessels of the neck as they are of good diameter and the pedicle length is long.
The shaping of the fibula is one of the advantages described in the literature but also prolongs overall operation time [40, 41]. The flexibility of the skin paddle is another advantage of the fibular free flap but also is time consuming due to the handling of the skin paddles containing small perforators [42]. The cutaneous component of the flap provides additional soft tissue for reconstruction of resected fistulas as in the presented cases and helps to establish tension-free wounds in the oral cavity as well [14].
The fibula flap is associated with significantly fewer complications such as infections at the recipient site and free flap loss compared to the iliac crest flap [41]. Debate continues as to whether the ileum or the fibula leave the more significant donor site defect although a majority would agree the ileum is more morbid. The DCIA composite flap has an unreliable skin component although the bulky internal oblique muscle can be used as a well-vascularized space filler which subsequently scars down into fibrous neomucosa.
Although bisphosphonates are also integrated into the transferred fibular flap, as they are systemic and present in all bones, the evidence to date is that this kind of bone with a direct blood supply and minimal demand on osteoclasts in integrating into the neomandible by internal fixation and prevention of contamination by a watertight mucosal seal has little risk of developing osteonecrosis related to bisphosphonates [14, 15, 21
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


