Introduction
The aim of this study was to assess the incidence of white spot lesions (WSLs) in subjects treated with customized lingual multibracket appliances—separately for maxillary anterior teeth 12 to 22 (according to the Fédération Dentaire Internationale numbering system) as well as for tooth groups 15 to 45, 16 to 46, and 17 to 47—and to determine the impact of patient-related and treatment-related variables on the frequencies of new WSLs.
Methods
Of 214 subjects comprehensively treated between June 1, 2011, and May 31, 2014, in 1 orthodontic center (Bad Essen, Germany) with a completely customized lingual appliance (WIN; DW Lingual Systems, Bad Essen, Germany), 174 (47% boys, 53% girls; mean age, 14.35 ± 1.23 years [minimum, 11.35 years; maximum, 17.91 years]) were recruited with inclusion criteria of completed lingual multibracket treatment of their maxillary and mandibular permanent teeth 17 to 47 (4582 teeth in the study), and age less than 18 years at the initial appointment. WSL assessment was accomplished using standardized digital high-resolution maxillary and mandibular occlusal photographs taken before bracketing and after debonding. Nonparametric analysis of variance was performed, taking into account the subjects’ grouped ages (≤16 or >16 years), sexes, and treatment durations.
Results
Of the total population of subjects, 41.95% developed at least 1 new WSL when all teeth, 17 to 47, were considered, and this incidence was 27.01% for tooth group 16 to 46, or 10.59% of subjects and 4.74% of the maxillary incisors (12 to 22). Of all teeth under consideration, 3.19% developed a WSL during treatment. The frequencies of decalcification were not significantly increased in preadolescents (≤16 years) compared with adolescents (>16 years). Treatment duration had a significant adverse impact on WSL formation in tooth groups 15 to 45 and 16 to 46, and in complete dental arches (teeth 17 to 47).
Conclusions
Subject-related and tooth-related WSL incidences of both single tooth groups and complete dental arches in subjects treated with the lingual WIN appliance were distinctly reduced when compared with previous reports of enamel decalcification after conventional labial multibracket treatment.
Highlights
- •
Preventing enamel demineralization and incipient caries is critical in orthodontics.
- •
White spot lesions (WSLs) occur in up to 73% of labial multibracket treatments.
- •
We assessed WSLs in 174 subjects treated with customized lingual multibrackets.
- •
Patients with the lingual brackets had distinctively fewer WSLs than patients with labial brackets.
Multibracket (MB) treatment is a routine and frequent procedure used currently in orthodontics because it is the only noncompliance treatment approach for 3-dimensional dental arch adjustments. However, its downside is the increase in the risks of white spot lesion (WSL) formation and incipient caries. Despite the general tendency of WSL surfaces to remineralize and harden after debonding, the esthetic aspect in maxillary anterior teeth affected by WSLs and decalcifications remains highly problematic, even 12 years after treatment. Therefore, prevention and treatment of WSLs have become matters of concern among orthodontists, and a health care market has emerged in recent decades to respond to this situation, including new microinvasive approaches for WSL infiltration and camouflage. Nonetheless, it is undeniable that even thorough oral hygiene is not sufficient for preventing WSLs in many patients. Moreover, further preventive strategies, such as the application of fluoride-releasing sealants and bonding materials, daily rinsing with sodium fluoride mouth rinse, or chlorhexidine applications, have failed to prevent WSL formation. An additional source of frustration is the finding from previous research of increased WSL susceptibility in preadolescents, who are also a major age group for MB interventions.
Intensive clinical studies of WSL formation on maxillary incisors and canines as a side effect of buccal MB treatment have found subject-related incidences of at least 1 new WSL of 46% within 12 months, or 36% for maxillary and mandibular incisors, whereas other authors have even reported 60.9% for maxillary incisors considered alone. For all maxillary and mandibular anterior and posterior teeth, including the first molars, 16 to 46 (according to the Fédération Dentaire Internationale numbering system), WSL incidences up to 72.9% can be expected during MB interventions.
As a totally different approach to preventing WSL formation during orthodontic treatment, the use of lingual MB appliances has recently been reconsidered as a method that is potentially superior to conventional labial fixed orthodontic treatment because of the reduced occurrence of decalcifications on lingual enamel surfaces. However, detailed information derived from clinical studies is limited. Although there are many studies or systematic reviews available regarding the incidence of WSL formation during labial bracket treatment as a function of location, subject age and sex, and even as an iatrogenic side effect of surplus orthodontic etching, there is not enough equivalent information concerning lingual-bracket induced WSLs that would enable us to support or reject the hypothesis of improving WSL prevention during comprehensive orthodontic treatment simply by choosing lingual appliances instead of conventional fixed labial approaches.
A potential disadvantage of lingual orthodontic treatment is that additional costs compared with conventional MB treatment may be incurred initially. However, if the hypothesis of a decreased incidence of WSLs is valid, these costs may be balanced against the costs of preventive measures against WSLs, such as the use of enamel sealants, as needed when using conventional MB appliances, or potential costs that may be incurred for treatment of labial WSLs, such as microabrasion or resin infiltration.
The objective of this study was to assess the incidence of WSL formation in subjects treated with completely customized lingual MB appliances (WIN; DW Lingual Systems, Bad Essen, Germany), separately for the maxillary incisors (12-22; Table I ), as well as for tooth groups 15 to 45, 16 to 46, and 17 to 47, to allow comparisons with existing data on labial WSL formation and consider the impact of patient variables (age, ≤16 or >16 years; and sex) and treatment duration on WSL formation.
| Tooth group | Maximum number of teeth per subject | Definition by FDI numbering system (universal numbering system) |
|---|---|---|
| 12-22 | 4 | Maxillary incisors: 22, 21, 11, 12 (UNS: teeth 7, 8, 9, 10) |
| 15-45 | 20 | Maxillary and mandibular incisors, canines, first and second premolars: 11-15, 21-25, 31-35, 41-45 (UNS: teeth 4-13 and 20-29) |
| 16-46 | 24 | Maxillary and mandibular incisors, canines, first and second premolars, and first molars: 11-16, 21-26, 31-36, 41-46 (UNS: teeth 3-14 and 19-30) |
| 17-47 | 28 | Maxillary and mandibular incisors, canines, first and second premolars, and first and second molars: 11-17, 21-27, 31-37, 41-47 (UNS: teeth 2-15 and 18-31) |
Material and methods
Our report is based on a single-center retrospective study of the incidence of WSL induced by lingual MB appliances.
Of 214 patients comprehensively treated from June 1, 2011, to May 31, 2014, in 1 orthodontic center (Bad Essen, Germany) with completely customized lingual WIN appliances, 174 participants (82 boys [47%], 92 girls [53%]; mean age, 14.36 ± 1.23 years [minimum, 11.35 years; maximum, 17.91 years]) were recruited. We adopted the following inclusion criteria: (1) lingual MB treatment of the maxillary and mandibular permanent teeth (from central incisor to second molar) with the WIN appliance; (2) age less than 18 years at the initial appointment; (3) debonding completed; and (4) high-quality initial and final intraoral top-view photographs. The exclusion criterion was missing or low-quality photographs.
Accordingly, of the 214 potentially eligible subjects, 40 (18.69%) were excluded from analysis because they were 18 years of age or older. None was excluded because of missing or low-quality photographs.
Single deciduous teeth and teeth with restorations in the area of the palatal or lingual bracket bases were excluded from the analysis, as were teeth whose lingual surfaces were not clearly visible or could not be judged on either photograph—eg, because of labiolingual inclination. Thus, a total of 279 teeth (5.7%), including 40 maxillary incisors (12-22), 46 mandibular incisors (32-42), 88 maxillary canines and posterior teeth (13-17 and 23-27, respectively), and 105 mandibular canines and posterior teeth (33-37 and 43-47, respectively), were excluded because they could not be judged from either of the photographs, taken before treatment or at debracketing. The final number of trial teeth was 4582.
The records included each subject’s age, sex, and time points of bracketing and debracketing. After subjects aged 18 or more years were excluded, the sample was further divided into 2 age groups: 16 years of age and less, and more than 16 years. Ninety percent (n = 156) of the subjects were 16 years old or less, and 10% (n = 18) were older than 16 years.
They received identical, standardized oral hygiene instructions, including the advice to brush their teeth at least 3 times daily with typical commercially available 1400 to 1450 ppm fluoridated dentifrices; otherwise, oral hygiene was not considered as a cofactor in our analysis.
To be able to compare our findings with previous research on WSL incidence after labial bracket treatment, analyses were performed separately for specific tooth groups ( Table I ).
This study received full ethical approval from the ethics committee of Hannover Medical School in Germany (number 1189/2011), and all patients or their guardians gave informed consent before the study.
For the WSL and enamel cavitation assessments, standardized high-resolution intraoral maxillary and mandibular occlusal photographs were taken of the dental arches before bracketing and directly after debracketing by the same operator (D.W.) using a digital camera (D-200, AF Mikro Nikkor 105 mm 1:2.8D, Makro Speedlight SB-29s; Nikon, Tokyo, Japan) and intraoral mirrors. Before the WSL screenings, the mirrored images were swiveled back to their true sides for an unambiguous assignment of quadrants and teeth. Screenings of the lingual enamel surfaces were performed in a darkened room by an assessor (E.K.) on a high-resolution screen (VP950 b; screen diameter, 19 in; maximum resolution, 1280 × 1024; ViewSonic, Walnut, Calif) and by another assessor (M.K.) (MacBook Pro Retina 2013; Apple, Cupertino, Calif) by enlarging each enamel surface to full-screen size ( Fig 1 ).
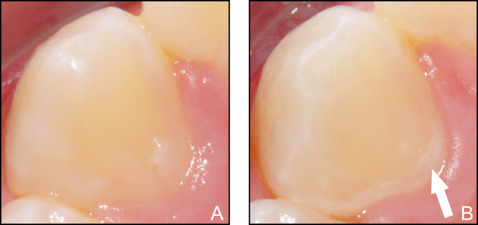
One assessor (E.K.) was trained and calibrated in assessing lingual WSLs. The primary outcome measures were sound enamel and the numbers of WSLs. A WSL was defined as the “first sign of a caries lesion on enamel detected with the naked eye” : ie, demineralized, slightly rough or chalky enamel opacities on smooth surfaces at or near the area of the former orthodontic brackets. To differentiate between these and other white discolorations of enamel, such as dental fluorosis, the latter was defined as a white to yellowish lesion blending with normal enamel and without well-defined margins or with blurred outlines, in contrast to WSLs, which have more defined outlines and are well differentiated from the surrounding enamel. As an additional aid in distinguishing between WSLs and fluorosis, we checked whether there was a symmetrical distribution of those opacities when considering the complete dental arches as is typical for fluoride opacities, or whether they were randomly distributed as is typical for WSLs.
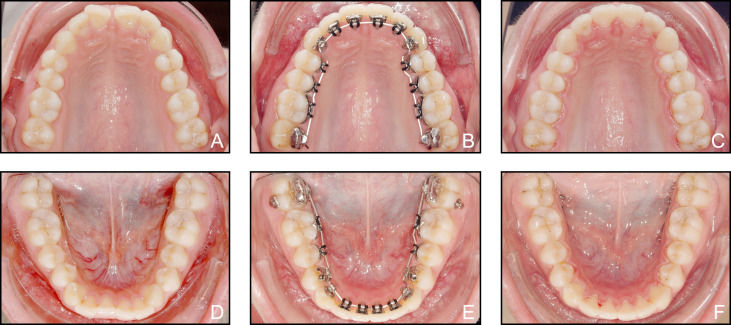
All lingual orthodontic MB treatments were carried out at the same orthodontic center (Bad Essen, Germany) with a standardized indirect bonding routine and the WIN appliance ( Fig 2 ). For indirect bracket bonding, the chemically cured resin Maximum Cure (Reliance Orthodontic Products, Itasca, Ill) was applied to both bracket bases and lingual enamel surfaces, after the application of a thin layer of a fluoride-releasing dual-cure, single-component bonding agent to the enamel (ExciTE F DSC; Ivoclar Vivadent, Ellwangen, Germany).
Statistical analysis
The features of the 174 subjects (4582 teeth) such as treatment time and age distribution were descriptively analyzed (means and standard deviations). Nonparametric, multifactorial analysis of covariance (ANCOVA) was used to assess the impact of the factors “sex” (female, 0; male, 1) and “age group” (≤16, 0; >16, 1), adjusted by the covariable “treatment duration” on the incidence of WSLs for the specific tooth groups. Both tooth-related and subject-related incidences of WSLs were calculated for each tooth group shown in Table I . The significance level was set at α = 5%. Statistical software packages (SAS version 9.3; SAS Institute; Cary, NC; and STATISTICA version 10; StatSoft, Tulsa, Okla) were used for the statistical analyses.
Four weeks after the trial assessments, both intraoperator and interoperator method errors were calculated on the basis of reassessments of a random sequence of 40 participants in the study (80 assessments; 2071 teeth; random sequence generator, www.random.org ) by 2 raters (E.K. and M.K.) for both assessments. This was done to assess the validity of the method as well as possible. Both operators were calibrated and trained in assessing WSLs. The intraoperator assessment deviation in WSL classification was 2.8%. Table II gives the detailed method error assessment results.
| Time point | Subjects (n) | Frequencies of unequal WSL classifications/valid teeth, n (%) | |
|---|---|---|---|
| Interoperator error (assessors M.K. vs E.K.) | Intraoperator error (assessor E.K.1 vs E.K.2) | ||
| Before treatment | 40 | 25/1035 (2.42) | 9/1039 (0.87) |
| After treatment | 40 | 86/1036 (8.3) | 49/1032 (4.75) |
| Total | 80 | 111/2071 (5.36) | 58/2071 (2.80) |
Results
Mean lingual MB treatment duration was 19.02 ± 4.63 months (minimum, 7.67 months; maximum, 29.47 months). The global incidence of new WSLs was 3.19% for all teeth (17-47); 41.95% of the subjects were affected by at least 1 new WSL. The subject-related incidence was 27.01% for tooth group 16 to 46, or 10.59% when considering the maxillary incisors separately. Further details about subject-related incidence and percentages of affected teeth for specific tooth groups are given in Table III .
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


