4. Proceeding deeper into the cavity preparation, upon moving from ablating enamel to ablating dentin, the clinician must adjust the settings from higher energy to lower energy for two reasons:
a. Because enamel is not innervated, but dentin is composed of dentinal tubules, which have nerve tissue, as the enamel is ablated to expose the dentinoenamel junction, the settings must be decreased. Most hard tissue lasers have preset power levels, which are lower for dentin than for enamel. As the laser ablates the decayed enamel, and the dentin becomes exposed, the nerve tissue within the exposed dentinal tubules may be affected by the air or water from the laser, which the patient will perceive as pain. With lowering of parameters as the laser nears the dentinoenamel junction, the patient may have no sensation at all.
b. Upon moving from a more calcified (healthy) tissue to a less calcified (higher water content) tissue, parameters must be lowered. Dentin has a higher water content than enamel, so the laser will ablate dentin more quickly than enamel, possibly cutting through the dentin too quickly and leading to excessive tooth structure removal.
5. Knowledge of spot size and power density allows selection of the proper sapphire or quartz tip for the procedure (see Chapter 2). As with selecting a #1 or a #6 round bur based on amount of decay, selection of the correct size of laser tip will affect procedural efficiency. Class V preparations generally are wide yet shallow; accordingly, a large spot size is needed for these preparations, with selection of a wide tip recommended. A small occlusal pit may be narrow buccolingually or mesiodistally but extend deep into the tooth. A small spot size would be more effective for this procedure, so a small-diameter laser tip would be appropriate. Other cavity preparations will require different size tips, depending on the width and depth of the decay. Because an inverse relationship exists between power density and spot size, a change in tip diameter during the procedure will require a change in laser parameters.
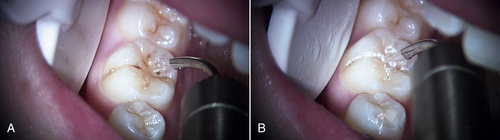
• Figure 11-2 A, Class II caries. Matrix band is placed on adjacent tooth to prevent accidental removal of its structure. B, Class II caries removal with erbium laser.
6. With class V preparations that extend subgingivally, it may be impossible to complete the procedure without performing an access gingivectomy. When changing from hard tissue treatment to soft tissue treatment, the water spray should be shut off. Use of the water spray during ablation of soft tissue with an erbium laser will not allow for adequate hemostasis of the soft tissue. Once the soft tissue ablation is completed, the water spray should be turned on to complete the hard tissue procedure. The power parameters also must be adjusted.
Figures 11-1 to 11-5 show erbium laser removal of class I to V caries. Figure 11-6 shows the result of conventional instrumentation for caries removal using local anesthesia in a pediatric patient.
Soft Tissue Procedures
A wide array of soft tissue procedures may be performed with lasers in the pediatric dental office.25–31 Erbium lasers may be used to accomplish many soft tissue procedures with little or no bleeding when used at lower energy settings than for hard tissue procedures, and without water spray. In some cases, however, a diode, CO2, or Nd:YAG laser may be better suited to the procedure. Patients with bleeding disorders (e.g., von Willebrand disease, hemophilia) or those receiving anticoagulants (e.g., aspirin, warfarin) will benefit from the superior hemostatic ability of these lasers.
Pediatric soft tissue laser procedures include the following:
• Maxillary frenum revisions
• Mandibular frenum revisions
• Lingual frenum revisions
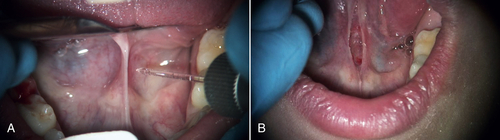
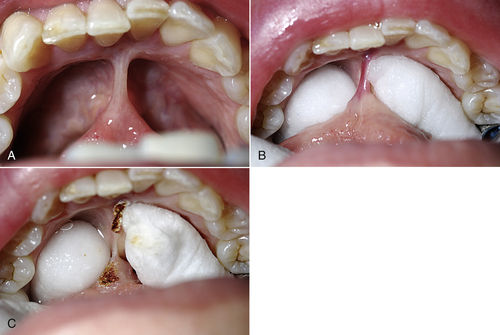
• Figure 11-4 A, Class V caries removal combined with access gingivectomy. Both procedures were completed using an erbium laser. B, Immediate postoperative view of restoration.
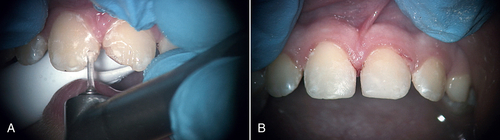
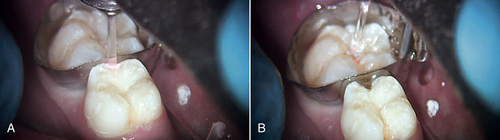
• Figure 11-5 A, Class IV erbium laser preparations on maxillary central incisors fractured as a consequence of trauma. B, Fractures repaired and tooth structure restored.

• Figure 11-6 Lip bite in child resulting from use of local anesthetic. The ability to perform operative dentistry without injection of local anesthetic makes this a relic of twentieth-century dentistry.
• Removal of hyperplastic tissue caused by drugs or suboptimal oral care in orthodontic patients
• Biopsies
• Treatment of aphthous ulcers and herpes labialis
• Pulpotomies
• Pulp capping
• Exposure of unerupted teeth
Frenum Revisions
Indications for frenum revision in the infant, child, or adolescent patient range from an inability to nurse in newborns to speech pathology in children to orthodontic problems in preadolescent and adolescent patients. The correction of an aberrant frenum, whether by blade, electrosurgical unit, or laser, is basically the same: removal of the fibers causing the problem. For the purposes of frenectomy, the three types of frena are lingual, maxillary anterior, and mandibular anterior.
Correction of Nursing Problems
Parents have many concerns when a minor surgical treatment for infants and young children is recommended. A common scenario involves a preadmission physical examination and blood work; early-morning surgery with nothing to eat for the previous 6 h; general anesthesia in the operating room; and postoperative discomfort for a few days. The clinician may have heard the following questions and concerns regarding pediatric treatment:
• Is this an elective procedure?
• Does the child really need to be placed under general anesthesia? Is the child too young to have frenectomy performed as a general anesthetic procedure?
• Should the procedure be delayed until the child is older (and the operating room “safer”)?
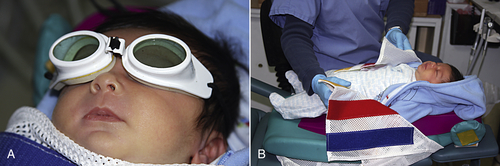
• Figure 11-7 Preparation of a 1-day-old infant for laser surgery. This newborn required lingual frenum revision because of inability to nurse. A, Use of wavelength-specific protective eye goggles. B, The child is placed in a protective patient stabilizer.
• “Why can’t we wait to see if the problem corrects itself as our child matures?”
• “I do not want to put my child through the procedure because I had horrible pain when I had it done as a child.”
Although these objections may have been raised before the introduction of lasers to dentistry, their persistence as encountered in clinical practice reflects how some parents, friends, relatives, and physicians react when a child is born with a dental anomaly such as an abnormal lingual frenum or maxillary anterior frenum attachment that must be corrected. New mothers look forward to comforting and nurturing their newborn by nursing, which they view as the best way to ensure that the child receives the safest and best nourishment. When problems occur and the mother consults with a lactation specialist, the diagnosis of a short or tight lingual frenum with or without a tight maxillary frenum may be the major cause of the nursing problem.32–37
One of the most satisfying procedures in my own clinical practice is correcting a neonate’s inability to nurse. A short lingual frenum, which occurs in approximately 3% to 4% of infants, may prevent the baby from properly latching on to the mother’s nipple. This impaired function may result in failure of the infant to gain appropriate weight despite nursing every 2 h and, for the mother, painful nursing periods, followed by development of sore and flattened nipples and painful mastitis, and eventually the need to replace nursing at the breast with bottle feedings.27,38–42
Laser frenum correction is a safe, simple, and quick procedure that is a significantly less expensive option than conventional surgery. Any dental laser currently available (Nd:YAG, diode, CO2, erbium) can complete this procedure literally in seconds, with no need for an operating room or general anesthesia, in a quick office visit, often with less pain than that from a local anesthetic injection, allowing the mother to begin nursing efficiently and painlessly.
The procedure is completed by placing the infant in a stabilization device or wrapping the infant in a small receiving blanket. The tongue is elevated using a grooved tongue director and a small amount of topical anesthetic placed. If the erbium wavelength is selected, no water is used. No sutures are required. The infant is seen in 5 to 6 days for a follow-up examination (Figures 11-7 and 11-8).
Maxillary and Mandibular Frenectomy
Although all laser wavelengths can be used successfully to perform maxillary and mandibular frenectomies, in patients with bleeding disorders who require hemostasis during soft tissue surgery, diode, CO2, or Nd:YAG lasers are the safest choice. These three lasers are much better than erbium lasers at creating excellent hemostasis immediately after frenum revision. Patients with bleeding or clotting disorders may be treated with these lasers without medical intervention, avoiding potential hospitalization to prevent or treat postsurgical bleeding complications as well as medication costs. Figure 11-9 illustrates a maxillary anterior laser frenectomy in a child with von Willebrand disease. In cases such as these involving medically compromised patients, a consultative telephone conversation with the primary care physician is always strongly recommended.
Lingual Frenum Revisions
To assist in the diagnosis and treatment of lingual frenum abnormalities, the author created the following classification system based on the distance from the origin of the frenum at the tip of the tongue to the insertion of the frenum on the mandible: Normal frenum attachment length is more than 16 mm from tongue tip to frenum insertion.25 Class I frenum length is 12 to 16 mm; class II, 8 to 12 mm; class III, 4 to 8 mm; and class IV, 0 to 4 mm.
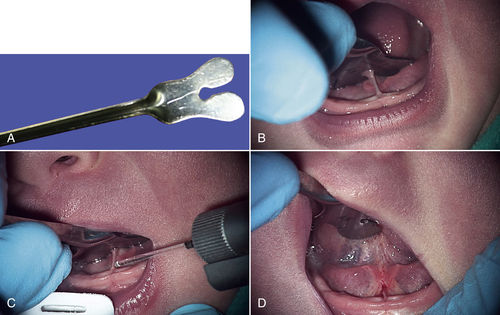
• Figure 11-8 Lingual frenum revision procedure in the infant shown in Figure 11-7. A, Grooved tongue director is used to stabilize the tongue. B, Preoperative view of lingual frenum. C, Intraoperative view of lingual frenectomy. No local anesthetic was used. D, Immediate postoperative view.
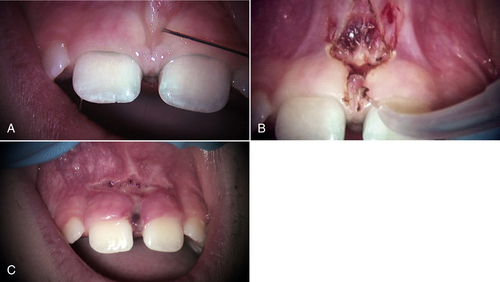
• Figure 11-9 Maxillary frenum revision for a pediatric patient with a bleeding disorder (von Willebrand disease). A, Preoperative view. B, Immediate postoperative view. C, Six-day postoperative view. This procedure was performed with a 980-nm diode laser.
When the frenum insertion length is less than 8 mm, the author usually recommend a frenum revision. Whether the patient is a few days old or in the teenage years, the revision of the lingual frenum is easily completed using any laser wavelength in 15 to 30 sec. Postoperative care includes over-the-counter pain medications if discomfort occurs. To prevent reattachment, the parent is instructed to have the child exercise the tongue and to stretch the area daily. A follow-up appointment is scheduled for 6 to 7 days later (Figures 11-11 and 11-12).
Diode and Nd:YAG laser wavelengths are absorbed by pigmented chromophores such as hemoglobin, which is abundant in vascular areas such as the floor of the mouth. CO2 and erbium laser energies are absorbed by water, which is abundant in the mouth floor mucosa. The beginner laser clinician should place wet cotton rolls or gauze on the floor of the mouth to protect the delicate tissue from stray laser energy. Also, application of the laser significantly inferior to the lingual surface of the lower incisors should be avoided because of the proximity of the sublingual glands.
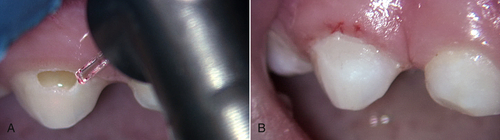
Hyperplastic Gingival Tissue
When the final result of orthodontic repositioning of the front teeth results in gingival hypertrophy, or orthodontic therapy itself causes gingival hypertrophy from poor oral hygiene, the laser can be a useful tool to increase crown length, to give the patient a more esthetic-appearing smile. Depending on the wavelength used and the amount of tissue revision needed, this procedure may be accomplished without local anesthesia. Patients who have drug-induced hyperplastic tissue, as from phenytoin (Dilantin) administration, as well as organ transplant recipients taking cyclosporine, also can have this tissue reduced and reshaped with lasers43,44 (Figures 11-13 to 11-15).
Lesion Removal and Biopsy
Fibrotic lesions, gingival growths, mucoceles, and other types of lesions can be quickly and safely removed using lasers. Lesion removal usually requires use of a local anesthetic (Figures 11-16 and 11-17). This topic is discussed in detail in Chapter 8.
Herpes Labialis and Aphthous Ulcer
Two of the most debilitating oral lesions that may arise in children are recurrent herpes labialis and aphthous ulcers. Dental lasers can immediately relieve the pain of aphthous ulcer lesions45,46 and often stop or reduce pain associated with herpes labialis lesions. Treatment of these lesions usually is performed at low power settings in a defocused mode. The purpose is not to ablate the tissue but to modify the surface epithelium of the lesion (Figures 11-18 and 11-19).
• Figure 11-12 A, Frenum and floor of mouth before placement of cotton rolls. B, After placement of cotton rolls. C, After beginning of laser ablation of frenum. (Courtesy Dr. Robert Convissar.)
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses