Robert P. Scholz: You have an interesting educational and work background. Where did you get started, and how did you end up with SureSmile?
Rohit C. L. Sachdeva: I was born in Kenya and completed my dental education at the University of Nairobi in the mid 1970s. I took a position as a registrar in orthodontics at the Royal Dental Hospital, University of London, under Dr Bill Houston. There, I was exposed to many orthodontic philosophies, including both functional and Begg. I moved to the United States in the early 1980s and completed my orthodontic residency at the University of Connecticut Health Sciences Center under Dr Charles Burstone. I learned the segmental approach to orthodontics and also developed an interest in the bioengineering aspects of orthodontics. I joined the University of Connecticut faculty and then moved to Canada and joined the faculty at the University of Manitoba, which also had a strong focus on bioengineering research in orthodontics.
In the late 1980s, I joined the faculty at Baylor College of Dentistry, Texas A and M University, in Dallas. This was a unique opportunity, since the entire department was being transformed after Dr Moody Alexander resigned. The environment was rich in clinical faculty participation and was strongly influenced by the Alexander discipline. The segmental approach to orthodontics was the polar opposite of the Alexander method in terms of philosophy of care; with time, I recognized the value of both, driven by the patient’s needs. So, in many ways, I was fortunate to be groomed by the best in terms of my clinical background. While in Connecticut, through sheer serendipity, friends introduced me to Professor Marv Wayman of the University of Illinois at Urbana; he was the world authority in shape-memory alloys and took it upon himself to mentor me in his field of research. I would travel frequently to his research laboratories, where I met his prize postdoctoral fellow Dr Shuichi Miyazaki from the University of Tsukuba in Japan, and we struck up a wonderful research collaboration—Shuichi from the scientific area and me from the clinical area. Just before moving to Baylor, Shuichi and I recognized the potential of adding copper to nickel-titanium alloys to produce low-hysteresis alloys. This invention resulted in my first patent, and we exclusively licensed it to Ormco.
In the mid 1990s, I met Professor Reggie Miethke from the Free University in Berlin on a lecture tour in India and was introduced to the first generation of robotic archwire-bending technology. With my background in telemedicine and material sciences and keen interest in clinical applications, I recognized that technology had developed to a point of convergence so that a new model of orthodontic care delivery through mass customization was possible.
Upon my return from India, I began searching for partners to help me realize this vision. I developed a relationship with a German company, Bending Art Medicine, the developer of the first generation robot and convinced it to support my work in the United States. The 2 principals, Rudger Rubbert and Fritz Riemeier, who are both engineers, recognized the potential of my vision and offered complete support. Again serendipitously, I was introduced to the first startup incubator in North Dallas called STARTech, which decided to seed the project.
By this time, I was a full professor with tenure. However, the desire to do something different was compelling. I resigned from Baylor in the late 1990s to reawaken my interest in the entrepreneurial world. I raised $8 million to start the foundation to realize my vision. We began as 2 people in Richardson, Texas, in 1 room and joined forces with the German company under the banner of OraMetrix. Today, we have more than 130 employees in our Berlin and US operations. We have excellent support from our venture partners, who have helped us raise close to $130 million. We have a great team and a visionary CEO in Chuck Abraham. He has led OraMetrix through exponential growth. In 2008 and 2009, we were recognized as one of the fastest growing privately held companies in Inc. Magazine’s annual Inc. 500 list (numbers 141 and 159, respectively). Today, we have over 70 patents issued and many more in the pipeline, and have made technologic breakthroughs in imaging and robotics that are considered industry-wide firsts.
Over 350 orthodontists are using our technologies and services. We have expanded into Canada and more recently into Australia, and have beta sites established in Germany. We are proud of our flagship client base, many of whom are board certified. Over the last 10 years of my journey with OraMetrix, I have been acculturated in business practices but, more importantly, have enjoyed visiting over 400 practices in the United States and have gained a deep understanding of the practice of orthodontics at both the clinical and operational levels. My family at OraMetrix and the extended family of practices continue to be sources of inspiration to me, and I owe a great gratitude to them for making me a better person.
RPS: You once said that the overall goal of SureSmile was to increase the time the orthodontist could spend on diagnosis by allowing technology to take over much of the required clinical time.
RCLS: Our goal is not to increase the doctor’s time, but to enable him or her to deliver better care through a proactive care model enabled by technology and processes. Charles Burstone said the practice of conventional orthodontics is “appliance driven.” The doctor is conditioned to approach care with minimal up-front diagnosis, relying substantially on a standard prescription designed into the bracket for the first half of the care cycle. In the second half, the doctor focuses on overcoming errors resulting from improper diagnosis, limitations of the standard bracket prescription and placement, and so on. This phase of treatment is highly reactive. The frequency of patient visits increases substantially, and the demands on doctor time increase. In some ways, the patient is moved from the “orthodontic general ward” to the “orthodontic intensive care unit.” SureSmile is designed to facilitate a proactive care delivery model. It enables the orthodontist to provide personalized and targeted therapeutics using robotically fabricated prescription archwires. The robot is driven by input from the doctor. This entails careful diagnosis and a well-designed treatment plan. The earlier in the care cycle the doctor engages in customization, the greater his ability to control variations. Yes, providing design input parameters on the front end of the care cycle takes a little more time. But this investment is repaid by avoiding the challenges of the reactive care model. With SureSmile technology, diagnosis drives therapeutics—ie, diagnopeutics.
Now, if you permit, I would like to share a broader perspective. Today, we are witnessing revolutionary developments in imaging and visualization technology available to us through 3-dimensional (3D) technologies such as the SureSmile OraScanner and cone-beam computed tomography (CBCT). Reading these images requires more cognitive effort on the front end to help us make better treatment decisions for our patients. On the other hand, robotic technology has helped to overcome the limitations of precision accuracy and reliability associated with manual and repetitive tasks performed at chair-side, such as archwire bending. This new dynamic challenges us to reconsider where our true value resides as orthodontists. Is it mental or manual dexterity?
I believe that our professional evolution will require integration of both high-value cognitive clinical skills applied on the front end with appropriate enabling technologies to drive personalized and targeted therapeutics.
RPS: SureSmile has changed direction several times. I remember visiting a large tent exhibit in Chicago where indirect bonding was the big topic. What was the SureSmile technique doing then?
RCLS: No, we have not changed directions. Our goal has always been to develop innovative technology and service solutions to help our customer—the orthodontist—provide better care for patients. Our platform technologies are the 3D imaging scanner, OraScanner, Decision Support Software, and Robotically Assisted Archwire Bending. We have the capability in our software to design bonding trays. But we know that indirect bonding, with or without customized brackets, is designed on the principle of a deterministic system. In other words, the design premise is that we can plan in advance exactly where the teeth will end up. Well, this is far from the truth. The biologic system we deal with is a complex adaptive one. More often, we as clinicians modify our treatment goals to accommodate an unexpected patient response. Take the example of poor patient compliance with Class II elastics or a patient who unexpectedly grows into a Class III relationship or has anchorage loss during space closure. You cannot plan for this in advance in your bracket placement or prescription. I don’t believe any doctor would in midtreatment remove all brackets and reconsider his or her indirect bonding or bracket prescription strategy. Appliance systems designed on the basis of deterministic systems are ill suited to allow the clinician to accommodate changing biologic conditions. The only practical solution to this problem is to build systems that provide control around the ability to affect the prescription of an archwire. This I call the “principle of adaptive therapeutics,” and the imperative need for this functionality is the driving force that gives the clinician unparalleled therapeutic control. This is why we do not offer indirect bonding trays as a part of our core service. SureSmile accounts for actual bracket placement when designing an archwire. So, practices are free to choose the bonding approach that best suits their work flow. Close to 10% of our practices use indirect bonding and find it more cost effective to make their own trays. Our doctors who use indirect bonding and who have considerable experience in its use have yet to finish patients with a straight wire. Also, several studies have shown that bracket placement with indirect bonding might not be substantially more accurate than with direct bonding. In the right hands, indirect bonding adds to operational efficiencies at chair-side during bonding.
RPS: Sometime later, the indirect bonding start disappeared, and the intraoral scan occurred at a later milestone during treatment. Why did that happen?
RCLS: This is called the intraoral therapeutic scan, which helps capture both the tooth and the bracket positions in 3 dimensions. It is an in-vivo scan and can be taken with CBCT or the OraScanner. The choice of the imaging technology is driven by the doctor’s and patient’s needs. The scan is generally taken between 3 and 6 months after the start of treatment, but it can be done at any time after bonding as determined by the doctor. Achieving some alignment and leveling with straight wire allows the doctor to better envision the treatment goals and design a prescriptive archwire with fewer conflicts. Additionally, this step substitutes for the bracket repositioning appointment and does not disrupt the operational schedule of the practice.
RPS: Briefly describe what the treatment-planning feature of SureSmile does for improving treatment outcomes.
RCLS: The treatment-planning software has many functional components: 3D visualization, measurement, communication, decision making with simulation, bracket placement, setup and archwire design, quality and outcome assessment, and SureSmile patient management. Each of these utilities used either singularly or in combination enables the doctor to make better informed decisions and design the targeted prescription archwire. For the sake of brevity, I will focus on a few of the tools.
The visualization software allows 3D views of multiple projections of the arches and the dentition. One can simultaneously assess the spatial position of any tooth and its unique morphology to better understand how it might affect the occlusal scheme. The tooth widths and Bolton analysis are automatically measured. Also, contact relationships between opposing teeth can be discerned. The decision support simulation software allows the orthodontist to simulate and visualize various treatment possibilities. Many setups can be done in 5 to 10 minutes to help the doctor compare different strategies and choose the optimal approach to treatment.
From a communications perspective, SureSmile visualization and interactive simulation tools provide a total immersive experience for the patients to understand their problems and become active participants in their own care. For patients requiring integrated care, treatment decisions can be effectively made through virtual consults with all doctors participating in real time at different locations. In addition to convenience, this approach to consults minimizes miscommunication between providers and allows better patient care. Many of our doctors also perform virtual consults with their patients. This allows for all decision makers to be present rather than the doctor hearing this response: “I will need to talk to my spouse and let you know.”
I have developed strategic design principles to help me use the tools more effectively in my decision making. Let me describe these.
Principle of Smart Orthodontics: I optimize the spatial position of the dentition by planning minimal tooth displacement and concurrently designing the effect of the therapeutic appliance into the treatment plan.
Principle of Risk Analysis: I can better visualize whether my care plan challenges the biologic boundaries and limitations in my treatment plan.
Principle of Image-guided Smart Bracket Placement: I use software to understand how I can optimize the coupling of prescription archwires with better bracket placement to control tooth movement and also develop a visual guide to bracket placement.
Principle of Constraint Management: I use simulations to try to understand where teeth will collide during alignment and leveling, and then I can plan strategically where I need to perform interproximal reduction or use other creative means to prevent or minimize tooth collision.
Principle of Anticipatory Orthodontics: With the aid of simulations, I try to predict treatment response at each appointment. These simulations are made available to both patients and staff at the beginning of treatment. They provide a visual map for the patient to follow care progress and substantially increase their adherence to elastic wear, for example. For the practice team, they provide a shared goal to achieve. The team is able to take a first-line diagnostic and communication role at the chair-side in assessing the patient’s response rather than being trapped in the doing vs the thinking and trying to envision the next steps in the doctor’s treatment plan. Finally, I believe an orthodontist should evaluate the treatment outcome for every patient. In other words, a clinician always needs to ask: did I achieve what I planned for the patient? SureSmile software tools allow the doctor not only to plan care but also to visualize and measure the outcome using automatic grading tools such as the discrepancy index and the ABO’s objective grading system.
The clinical application of simulation tools is a required skill for a diagnostically driven orthodontist today and is acquired through deliberate practice. There is a difference between a study model and what I call a diagnostic decision support simulation model, where each tooth is cut as a separate object to allow for simulation.
RPS: If SureSmile is intended to provide that excellent result with a shorter than usual treatment time, could not a doctor highly skilled in repositioning and wire bending achieve the same result in the same time?
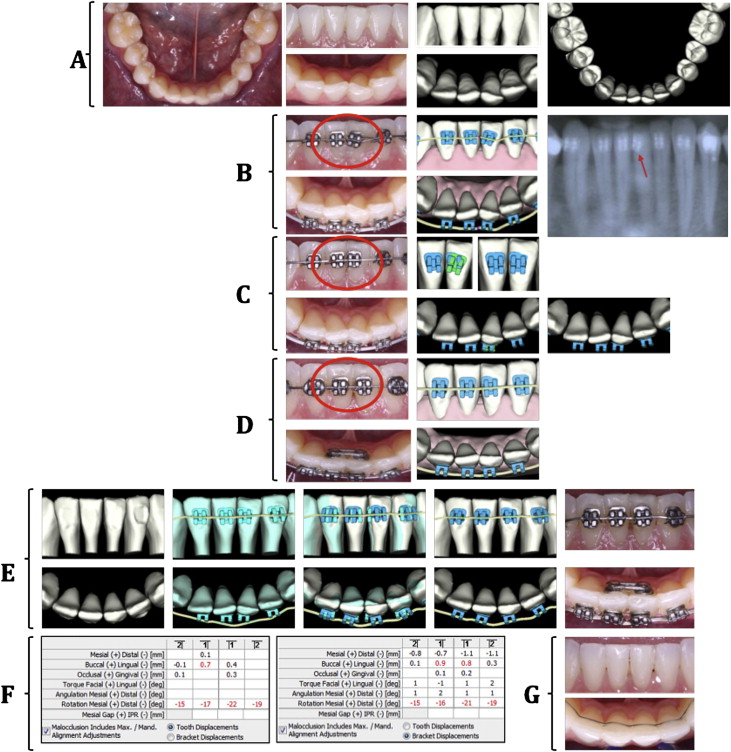
RCLS: No, I do not believe it is possible. You have just described to me a reactive care process. The effectiveness of those corrective measures is driven by a number of factors. These include (1) when during the care cycle was the error recognized? (2) was the root cause correctly diagnosed? (3) how often was the patient seen? and (4) what was the rate of tooth movement? Additionally, the assumption is that the orthodontist will be able to apply the bracket correctly the second time around in 3D space. Currently, we must wait for the archwire to work out before we know whether the bonding correction was right. The reactive process depends on iterations to achieve control. This is just not an effective approach to care. The same vagaries apply to archwire bending. How does the doctor know that the archwire is bent correctly—by measuring it? That is eyeballing, at best. The whole reactive process is fraught by a wait-and-see attitude and is best shown by the example shown in Figure 1 . SureSmile archwires provide a level of control in tooth movement that human hands cannot achieve.