The approach to orthodontic diagnosis has changed gradually but steadily over the past 2 decades. The shift away from diagnosis based entirely on hard tissue evaluations has been a result of a broadened recognition of the importance of facial and smile appearance to our patients, and how they change over time. The purpose of this article is to describe and illustrate the integration of the new soft tissue paradigm into long-term treatment planning, with a focus on the esthetic goals of treatment.
Highlights
- •
Good data on soft tissue maturation and aging in the perioral area are available.
- •
Both hard and soft tissues should be considered in treatment planning.
- •
Each patient’s posttreatement soft tissue profile should be age appropriate.

The changes in approach to orthodontic diagnosis have been gradual but steady over the past 2 decades. The shift from diagnosis based entirely on hard tissue–based evaluations has been a result of a broadened recognition of facial and smile appearance by our patients, and thus by the orthodontic specialty. The current popularity of the “selfie” illustrates this point. Last year, I had the experience of riding a gondola to the top of a Colorado mountain—a 30-minute trip. In the gondola was a young lady whom I became fascinated in watching because, from the bottom of the mountain to the top, I counted that she took no less than 28 selfies! Different poses, some smiling (smiles are important!), some not (so is resting lip posture), but frontal pictures nonetheless. She might have suffered from a slightly excessive amount of narcissism, but many occupants of this large gondola documented their experience in similar fashion.
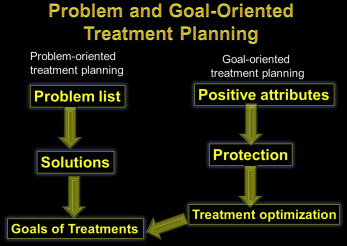
Orthodontics has evolved in many intellectual and practical steps. What develops intellectually naturally is challenged, tested, and then eventually incorporated into clinical practice as “what works.” Let’s start with a look at the evolution of hard tissue diagnosis and how it became so centered in cephalometrics. Cephalometric radiography was originally introduced to gain understanding of patterns of growth, development, and maturation. By the 1950s and 1960s, the combination naturally led to a focus on hard tissue elements and treatment plans based on study models and “normative” cephalometric measurements, and clinicians drifted away from the clinical examination of patients. Evaluation of the patient’s soft tissues is now a critical step in orthodontic treatment planning. In problem-oriented treatment planning, the orthodontist identifies and quantifies functional and esthetic abnormalities that need correction or improvement. Further evolution of the concept of problem-oriented diagnosis and treatment planning should now entail identification of both the normal and the positive elements of a patient’s appearance or smile that should be maintained or enhanced. This is termed “problem- and goal-oriented treatment planning” ( Fig 1 ). When clinicians focus solely on correcting the problems they see, they sometimes overlook the patient’s positive attributes and in doing so run the risk of unfavorably affecting the patient’s esthetics. The classic illustration concerns the Class II patient with a normal midface and a deficient mandible treated with maxillary premolar extractions and maxillary incisor retraction, resulting in flattening of the upper lip and an unflattering profile. In this approach to treatment, the problem was identified as a dental Class II malocclusion, and the extraction sequence was quite adequate to treat that problem. However, the facial esthetic appearance was ignored and deleteriously affected. In a more contemporary illustration, standard approaches to orthodontic treatment result in flattening the smile arc in about a third of patients, probably because it was not a factor considered in the treatment plan. During the clinical examination, we should document not only problems but also the positive elements that need protection. It is difficult to clearly illustrate this approach to treatment verbally or in writing only, so I have chosen to illustrate the integration of the new soft tissue paradigm into long-term treatment planning. The focus will be on the esthetic goals of treatment.
If our only goal is a Class I occlusion, treatment can often be efficient and even easy. On the other hand, patients and parents are inclined to focus primarily on the enhancement of appearance. If our only goal is aimed at the “social 6,” then this treatment can also be efficient and even easy. Contemporary treatment, of course, should have a broader scope, looking at both occlusion and appearance. Attainment of both excellent occlusion and excellent esthetics can indeed be quite difficult, but with the patient’s approval, it is the goal that we should all strive to achieve. To treat only the occlusion treats only half of the patient. If the same effort we have placed almost entirely on occlusion for decades is now put into enhancing appearance, we begin to be able to offer our patients treatment that promotes well-being on many levels, both functionally and esthetically. We will emphasize in this paper the importance of the clinical examination of the soft and hard tissues, their resting and dynamic (smiling) relationships, and the knowledge of how they change over time.
At some point in my orthodontic experience, it began to puzzle me that we would attempt to base our orthodontic treatment on a 2-dimensional lateral headfilm, taken in 1/60th of a second, and make the complex decisions of orthodontic treatment that are expected to endure decades of change. As a result of his research into craniofacial development, AJO-DO Editor-in-Chief Dr Rolf Behrents stated that “It is clear [that] the ability of cells, tissues, and organs to produce change in the craniofacial complex ceases perhaps only at death and not at some developmental event along the way.” This is the world of the contemporary orthodontist, dealing with a continuously changing substrate in both the adolescent and the adult, thinking far in advance of the outcome.
Systematic evaluation and treatment goal setting
Soft tissue changes occur over time, and it is usually the orthodontist who best understands the comprehensive principles of dental and skeletal development, maturation, and aging in addition to the many other facets of dental practice.
The 12-year-old girl in Figures 2 and 3 came with a chief complaint of “the dentist said I needed braces” because of her Class II deepbite malocclusion. Although correction of her malocclusion was the reason for seeking treatment, she obviously exhibited an excessive amount of gingivae on smiling, and this was thoroughly discussed with her parents as an esthetic objective of treatment. Gummy smiles like this patient’s often have multifactorial etiologies, and diagnosis is often dictated by the background of the person making the diagnosis—“diagnosis by procedure.”


Let me illustrate with this patient. If she was initially seen by an oral surgeon, the recommendation might lean toward surgery and maxillary impaction when of age; if she was seen initially by a periodontist, crown lengthening likely would be the treatment of choice; and if a cosmetic dentist was consulted, crown lengthening with the possibility of porcelain veneers would most likely be recommended. The purpose of this article is to illustrate a more globally oriented diagnostic regimen that requires a thorough knowledge of both craniofacial and soft tissue changes to better equip the diagnostician to direct appropriate treatment. This comprehensive knowledge is essential in a global diagnostic approach that includes both the functional and esthetic demands of today’s orthodontic environment. In our diagnostic regimen, we have carefully attempted to document all possible etiologies of, for example in this case, the excessive gingival display on smile. These include the following.
- 1.
Vertical maxillary excess: the clinical characteristics include excessive incisor display at rest, lips apart posture, lip strain, and excessive lower facial height.
- 2.
Short crown height: short crown height has 2 basic etiologies—gingival encroachment and incisor attrition. Gingival encroachment in an adolescent can include delayed active eruption or delayed passive eruption, and in both an adult and an adolescent, gingival hypertrophy.
- 3.
Short philtrum height: depending on the patient’s age, the ideal philtrum position is 2 to 3 mm shorter than the commissure height. As we will demonstrate later, this is highly variable with age.
- 4.
Hypermobile smile: elevation of the upper lip on smiling varies between persons. How do we tell when someone has a hypermobile smile? Empirically, if the patient does not have an excessive incisor display at rest and has normal crown height and facial height, then excessive gingival display would be attributable to excessive elevation of the upper lip on smiling. Recent studies have demonstrated that the average upper lip elevation is around 23% of its resting length.
- 5.
Retroclined or supererupted maxillary incisors: these are most often seen with dentoalveolar compensation for a Class II skeletal relationship.
The patient’s initial referral was prompted by the dentist’s suggestion that an orthodontic consultation was indicated because of her Class II deepbite—the functional reason for orthodontic treatment. Her esthetic evaluation began with the global approach of macro-, mini-, and microesthetic evaluations; we start from the outside in. This must be done in order, and the reason will be illustrated later. With her lips in repose and then in smiling, the systematic clinical examination for this patient was quantified as follows.
Macro-esthetic evaluation
- 1.
Short lower facial height. Having thirds of equal height is typically accepted as the most desirable vertical facial proportionality. However, an important key for orthodontists is the lower facial third, because this is the area over which we have the most influence and control.
- 2.
Lip incompetence of 5 mm.
- 3.
Convex profile with mandibular deficiency. It is the etiology of the Class II malocclusion.
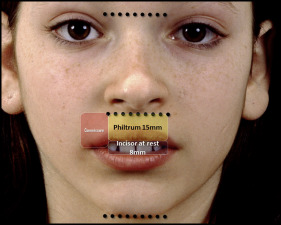
Mini-esthetic examination ( Figs 4 and 5 )
- 1.
Philtrum height of 15 mm. The philtrum height is measured in millimeters from subspinale (the base of the nose at the midline) to the most inferior portion of the upper lip on the midline. The absolute linear measurement is not particularly important, but what is significant is its relationship to the maxillary incisor and the commissures of the mouth. This relationship changes significantly over time. In an adolescent, it is common to find the philtrum height to be shorter than the commissure height. This difference can be explained by the differential and vertical lip growth over the long term ( Fig 6 ), because over the patient’s lifetime, the philtrum’s vertical length increases at a greater rate than the commissure, contributing to the flattening and aging of the upper lip in repose and contributing to decreased incisor display at rest ( Fig 7 ) and decreased gingival display on smiling ( Fig 8 ).