Recent innovations in technology and techniques in both surgical and orthodontic fields can be integrated, especially when treating subjects with facial asymmetry. In this article, we present a treatment method consisting of 3-dimensional computer-aided surgical and orthodontic planning, which was implemented with the orthognathic surgery-first approach. Virtual surgical planning, fabrication of surgical splints using the computer-aided design/computer-aided manufacturing technique, and prediction of final orthodontic occlusion using virtual planning with robotically assisted customized archwires were integrated for this patient. Excellent esthetic and occlusal outcomes were obtained in a short period of 5.5 months.
Highlights
- •
This article discusses management of facial asymmetry due to unilateral condylar hyperplasia with surgery-first approach.
- •
Integration of 3D computer assisted surgical and orthodontic planning was performed.
- •
The orthognathic surgery-first approach in conjunction with 3D surgical and dental planning may minimize treatment duration.
The advent of the digital era has enabled clinicians to use the best available data for evidence-based diagnosis, treatment planning, and execution of treatment. For accurate diagnosis, obtaining precise information from the imaging of the orofacial region in 3 dimensions is absolutely necessary to complement the clinical examination and a thorough medical and dental history, especially when treating complex malocclusions with orthognathic surgery. Traditionally, 2-dimensional (2D) imaging has been the standard for representing the 3-dimensional (3D) craniofacial region However, the most common problems with 2D imaging are image distortion, magnification errors, and landmark identification errors. With conventional treatment planning for orthognathic surgery using 2D imaging, treatment outcomes have been reported to be suboptimal, especially in patients requiring correction of pitch, roll, and yaw (ie, facial asymmetry).
With the introduction of 3D cone-beam computed tomography (CBCT), it has become possible to circumvent the above shortcomings. Image distortion and errors in landmark identification have been minimized, and the actual measurements (linear skeletal measurements, overjet, overbite, spacing, and dental arch widths) can be obtained accurately. Hence, the scope for applying 3D CBCT imaging has widened from image diagnosis to accurate quantification of the dimensions of the orofacial structures. Additionally, it is now possible to visualize the virtual patient by creating an integral fusion model combining the data from all 3 important tissue groups using a CBCT reconstructed bony volume, digital dental models, and a textured facial soft tissue image. This model is highly effective in precisely diagnosing the problem in all 3 spatial planes. Furthermore, the fusion model has enabled clinicians to accurately plan surgical movements in the virtual environment and generate highly accurate surgical splints using the computer-aided design/computer-aided manufacturing (CAD/CAM) technique for effective treatment outcomes. It was recently reported that patients with facial asymmetry requiring maxillary and mandibular yaw (rotation around a vertical axis) correction showed excellent positional and orientation accuracies when computer-aided surgical planning was performed.
In the last decade, significant technologic advancements have been made in computer-aided orthodontic treatment. SureSmile technology (OraMetrix, Richardson, Tex) is a type of computer-assisted orthodontic treatment in which an intraoral dental scanner (OraScanner; OraMetrix) and 3D software generate accurate and reliable 3D digital models from which virtual treatment plans are obtained through a software interface. The planned treatment can be accurately translated to the patient using robotically assisted archwire bending technology, thus possibly improving the overall treatment efficiency and quality.
In a previous case series, we demonstrated that efficient and effective outcomes can be achieved with 3D virtual surgical planning and digital splints for patients with facial asymmetry. In this study, we integrated the 3D virtual dental planning (SureSmile process) with the 3D virtual surgical planning along with fabrication of digital surgical splints using a CAD/CAM technique. The primary intent of this article is to document how the use of 3D digital technology and the surgery-first approach can significantly reduce the treatment time in a patient with facial asymmetry caused by unilateral condylar hyperplasia.
Case report
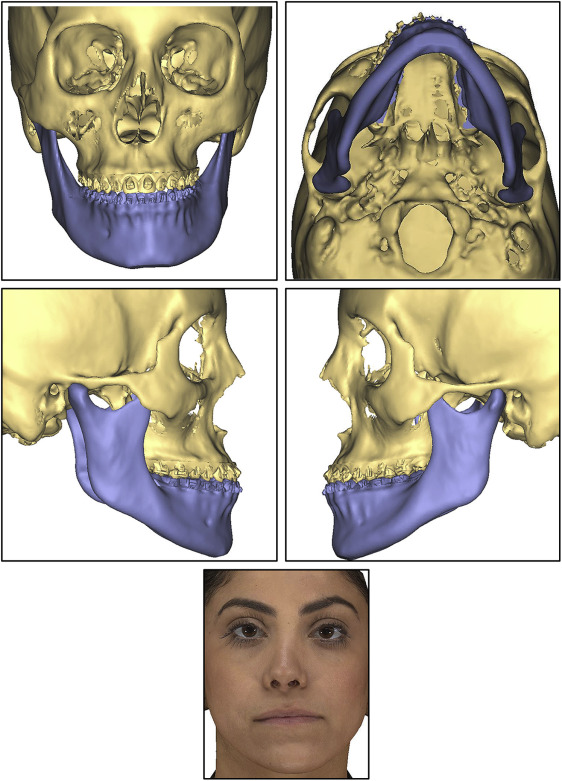
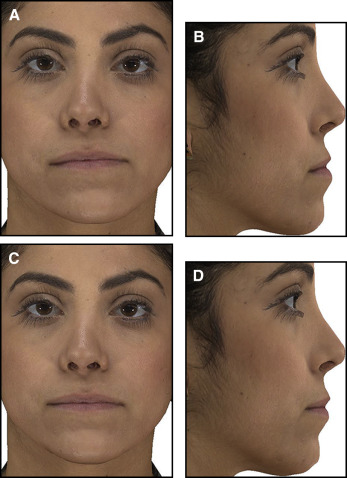
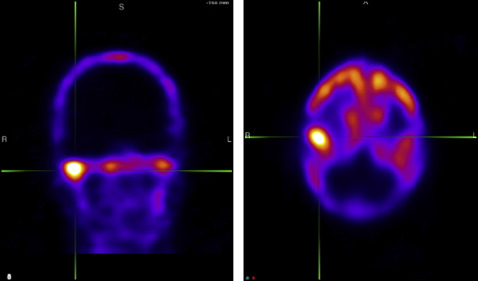
A 23-year-old Middle Eastern woman reported to the orthodontic clinic at the University of Connecticut with the primary complaint that her jaw was shifting to the left side, and she wanted her bite fixed ( Fig 1 ). Her past dental history showed a consultation with an oral surgeon 4 years previously during which a slight facial asymmetry with the chin point deviated toward the left side was documented. A subsequent clinical examination showed that her facial asymmetry had worsened, with the chin point deviated toward the left side of the facial midline by 4 mm. The patient was referred for a Technetium (Tc)-99 single photon emission computed tomography scintigraphy examination, and the radiology report suggested right unilateral condylar hyperplasia. Since condylar hyperactivity is expected to subside during the second and third decades of life, the surgeon recommended reevaluating her 9 to 12 months later. However, a second Tc-99 scan taken 9 months later again showed hyperactivity of the right mandibular condyle ( Fig 2 ).

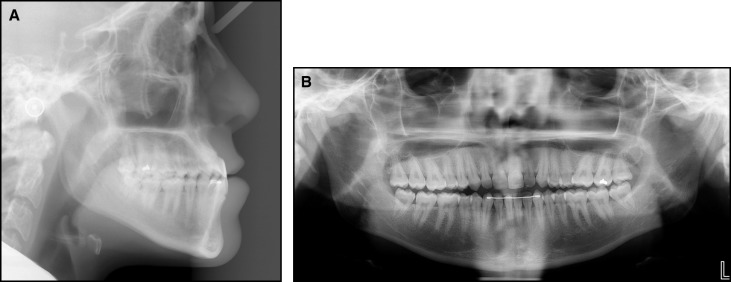
The extraoral examination showed facial asymmetry with the chin point deviated toward the left side of her face by 4 mm. Additionally, a deviated nasal septum toward the right side further accentuated the facial asymmetry. The extraoral frontal examination at rest showed a noticeable intercommissure cant and a paranasal deficiency, and the soft tissue lower border of the mandible was inferior on the right side compared with the left side ( Fig 1 ). A concave profile caused by a combination of maxillary deficiency and a prognathic mandible was observed ( Fig 3 , A ; Table ). Dentally, the patient had a bilateral Class III molar relationship that was more accentuated on the right side with an edge-to-edge bite anteriorly. An occlusal cant was evident, with the left buccal segment more coronal. The mandibular midline was deviated to the left side by 4 mm in reference to the facial midline. She had retroclined mandibular incisors and proclined maxillary incisors, indicating anteroposterior dental compensations for the underlying Class III skeletal relationship. Her smile showed a maxillary cant with a greater gingival display on the right side. The maxillary and mandibular arches were well aligned because she had prior orthodontic treatment. The panoramic x-ray showed different morphologies of the condyles and ramus lengths between the right and left sides ( Fig 3 , B ).
| Variable | Norm | Pretreatment | Posttreatment | Change |
|---|---|---|---|---|
| SNA (°) | 82 | 81.5 | 85.5 | 4 |
| SNB (°) | 80 | 85 | 85.5 | 0.5 |
| ANB (°) | 2 | −3.5 | 0 | 3.5 |
| SN-GoGn (°) | 32 | 29 | 31 | 2 |
| IMPA (°) | 90 | 82 | 82 | 0 |
| U1-SN (°) | 102 | 119 | 122 | 3 |
| U1-NA (mm) | 4 | 10 | 7 | −3 |
| L1-NB (mm) | 4 | 5 | 4.5 | −0.5 |
| Interincisal angle (°) | 131 | 126 | 122 | −4 |
| Upper lip to E-line (mm) | −4 | −3.8 | −2.2 | 1.6 |
| Lower lip to E-line (mm) | −2 | 1 | −1 | −2 |
The main treatment objectives were to prevent further worsening of the asymmetry caused by the active unilateral condylar hyperplasia, improve her facial esthetics and occlusion, and minimize the overall treatment time. Based on the guidelines of Wolford et al, treatment options of either high condylectomy and orthognathic surgery or orthognathic surgery when the hyperactivity of the condyle subsides were offered to the patient. She accepted the high condylectomy and orthognathic surgery-first approach for the correction of her facial asymmetry. The treatment goals consisted of preventing the worsening of facial asymmetry; improving her soft tissue profile; correlating her dental, skeletal, and soft tissue midlines to the facial midline; leveling her frontal occlusal plane; and improving her smile esthetics.
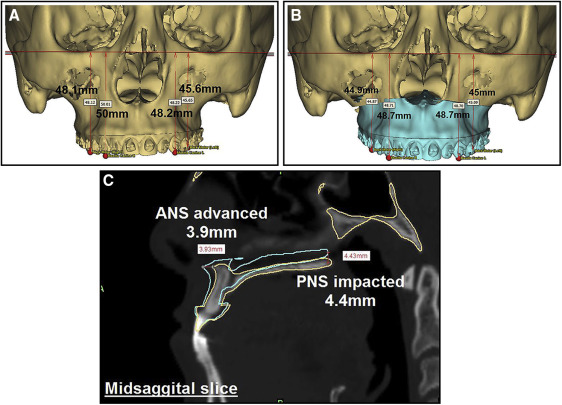
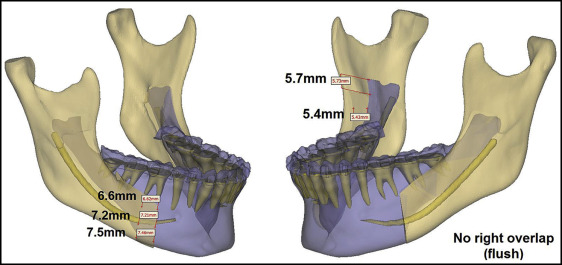
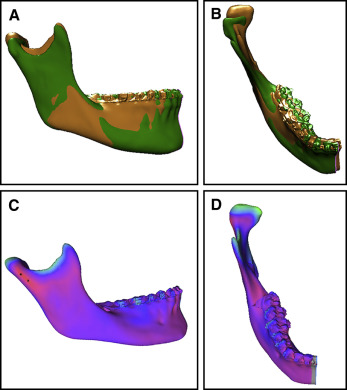
In this patient, both the surgical and orthodontic corrections were planned virtually. For the surgical plan, 3 weeks before the surgery, after indirect bonding of the orthodontic appliances (0.022-in preadjusted edgewise brackets), a CBCT scan (exposure time, 14 seconds; field of view, 12-in; voxel size, 1.25 mm) was taken for the construction of a fusion/composite model of the skull as described by Xia et al with Synthes PROPLAN CMF software (Materialise, Plymouth, Mich). The scan was oriented using the interorbital plane as the horizontal reference line. The midline was determined with a line perpendicular to and bisecting the horizontal reference line connecting the left and right orbitales. The patient’s 3D photographs (Vectra; Canfield Imaging Systems, Fairfield, NJ) were integrated with the CBCT scan to obtain a textured facial soft tissue image ( Fig 4 ). To achieve the treatment goals, the virtual surgical plan consisted of clockwise rotation of the maxillomandibular complex, a LeFort I osteotomy with advancement and asymmetric impaction of the maxilla ( Fig 5 ), and an asymmetric bilateral sagittal split osteotomy for mandibular setback ( Fig 6 ). A high condylectomy of the right mandibular condyle was planned by mirroring the normal contralateral condyle ( Fig 7 ). Soft tissue simulation was also performed based on the virtual surgical plan ( Fig 8 ) with an algorithm proprietary to the orthognathic surgical planning software company. Then the virtual plan was exported to the CAD/CAM software for digital construction of the surgical splints ( Fig 9 ). The intermediate and final digital splints, made of hybrid epoxy-acrylate polymer, were physically generated using the rapid prototyping additive manufacturing process (SLA-3500 machine; 3D Systems, Rock Hill, SC).