Oral and maxillofacial surgeons will always be involved with the evaluation and treatment of trauma to the mandibular condylar and subcondylar regions. These seemingly simple injuries can have devastating effects on mandibular form and function. If managed improperly, patients can be left with malocclusions, facial asymmetry, limited joint mobility, and chronic pain. Treatment recommendations continue to vary. Some feel that the majority of condylar and subcondylar fractures can, and should, be managed closed with a short period of maxillomandibular fixation followed by aggressive physical therapy aimed at regaining normal mobility and range of motion. Others feel that normal form and function can only be regained by an open procedure to establish an anatomic reduction and fixation of the fracture segments. All would agree that the focus should be on patient outcome. Normal joint function and occlusion can be restored in most cases. Evaluation and treatment planning of injuries to the condylar region should be based upon an understanding of the complex anatomy and physiology of this region. This chapter will review the anatomy and pathophysiology of mandibular condylar and subcondylar injuries. Etiologies and classification of injuries will be described. Key findings on the initial clinical and radiographic evaluation will be highlighted. Treatment options and surgical techniques will be discussed. The chapter will conclude with a review of the literature with an emphasis on outcome studies.
ANATOMY
A thorough understanding of the normal skeletal and soft tissue anatomy of the temporomandibular joint (TMJ) is a critical starting point before one can evaluate this region in the injured state. The temporomandibular joint is unique in structure and function. It is stabilized by a complex ligamentous system and its motion is orchestrated by a number of muscles. There are also a number of arteries, veins, and nerves in this region that need to be recognized and unharmed if an open procedure is considered. It has been said, “anatomy is destiny.” When the normal anatomy and function of the temporomandibular joint and surrounding structures are understood it becomes easier to predict and manage the effects of trauma.
JOINT
The temporomandibular joint is classified as a ginglymoarthrodial joint, allowing for both rotation (ginglymoid) and translational (arthrodial) movements. The mandibular condyle articulates at the cranial base with the squamous portion of the temporal bone. This concave portion of the temporal bone is termed the mandibular or glenoid fossa. The skeletal surfaces of the joint space are lined with specialized endothelial cells. These cells along with synovial tissue in the retrodiscal region produce synovial fluid. This fluid lubricates the joint during function and provides nutrients to this relatively avascular space. The articular disk separates the condylar head from the glenoid fossa, forming superior and inferior joint spaces. The disk is composed of dense fibrous connective tissue and is attached to both the condylar head and the temporal bone by the capsular ligament.
LIGAMENTS
The collateral discal ligaments tightly attach the articular disk to the condylar head both medially and laterally. This attachment allows for passive movement of the disk with the condylar head during translational movements.
The entire temporomandibular joint complex is surrounded by a dense fibrous connective tissue, the capsular ligament, on both the medial and lateral surfaces. The capsule attaches superiorly to the temporal bone along the borders of the articular surface and inferiorly to the condylar neck. This ligament functions to resist forces that would dislocate the articular surfaces. The capsule is thicker and stronger laterally. The lateral capsule is reinforced by thick bands of fibrous connective tissue and extends from the articular eminence to the condylar head and neck. These bands guide rotational movement and resist inferior displacement.
There are two additional ligaments, often termed accessory ligaments, that support the temporomandibular joint. The sphenomandibular and stylomandibular ligaments resist protrusive dislocation. The sphenomandibular ligament extends from the spine of the sphenoid bone to the lingual on the medial surface of the mandibular ramus. The stylomandibular ligament extends from the styloid process to the posterior border of the mandible.
MUSCLES
Several muscles act upon the mandibular condyle, ramus, and body. When the patient is healthy, these muscles generate the full range of motion of the temporomandibular joint and with trauma they are responsible for predictable patterns of injury.
The masseter muscle originates from the lateral aspect of the zygomatic arch and extends to the lateral aspect of the mandibular ramus and body. It extends inferiorly to the mandibular angle and inferior border of the mandibular body. This muscle elevates and protrudes the mandible. The temporalis muscle originates from the temporal fossa and its tendon inserts on the coronoid process and anterior border of the mandible. This muscle elevates and retrudes the mandible. The medial pterygoid muscle originates from the medial aspect of the lateral pterygoid plate and inserts on the medial aspects of the mandibular angle and ramus. The medial pterygoid muscle elevates and laterally protrudes the mandible. The medial pterygoid and masseter muscles form the pterygomasseteric sling, which supports the mandibular angle and ramus. The lateral pterygoid muscle is often described as having a superior and inferior portion. The superior lateral pterygoid muscle originates from the infratemporal surface of the greater wing of the sphenoid and inserts on the temporomandibular joint capsule and disk and the neck of the mandibular condyle. The insertion is primarily on the medial aspect of these structures. The superior portion of the lateral pterygoid muscle functions when the mandible is elevated against resistance. The inferior portion of the lateral pterygoid muscle originates from the lateral surface of the lateral pterygoid plate and inserts on the condylar neck. These muscles function during protrusion and lateral excursive movements of the mandible.
BLOOD VESSELS
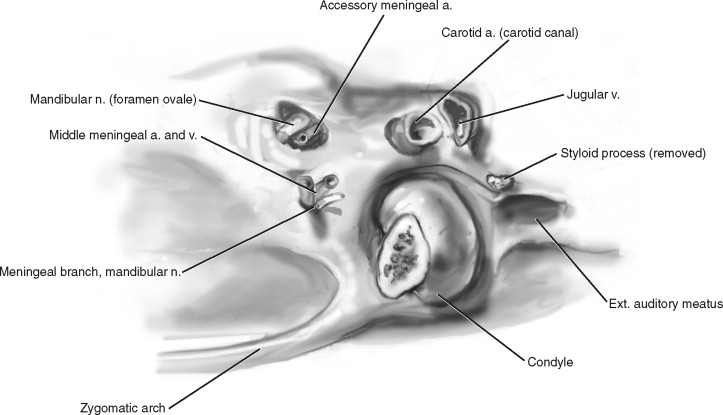
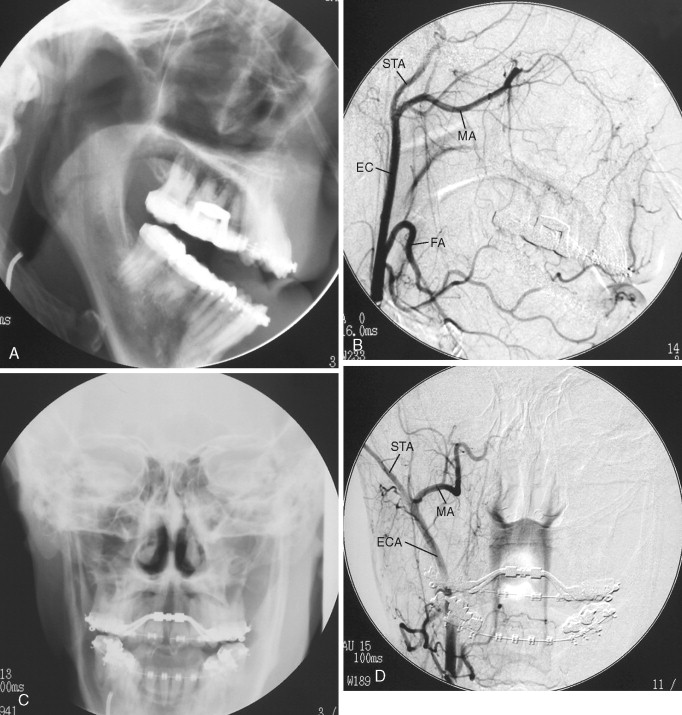
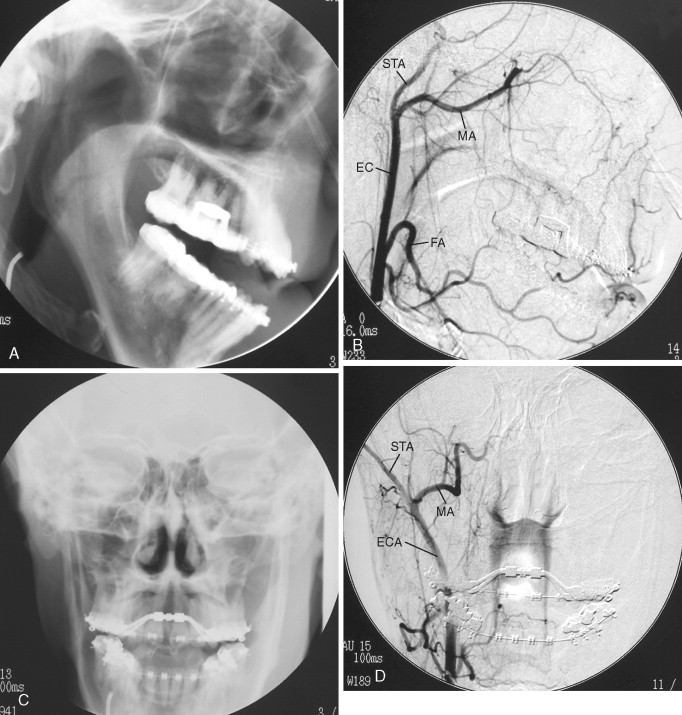
Although the temporomandibular joint itself is relatively avascular the soft tissue surrounding the mandibular condyle and subcondylar region is highly vascular. End branches of the external carotid artery travel on both the medial (maxillary artery) and lateral (superficial temporal artery) aspects of the condylar head and neck. The external carotid artery bifurcates in the region of the parotid gland, developing into the maxillary artery and superficial temporal arteries. Talebzadeh and Pogrel documented the close proximity of vascular structures to the medial aspect of the temporomandibular joint. In their cadaver study they found that the middle meningeal artery was as close as 2.3 mm from the medial aspect of the glenoid fossa ( Figure 11-1 ).
SUPERFICIAL TEMPORAL ARTERY
The superficial temporal artery in the pre-auricular region runs in the temporoparietal fascia just beneath the subcutaneous fat layer. The superficial temporal artery crosses lateral to the zygomatic arch and forms a single branch, the transverse facial artery. After crossing over the zygomatic arch the superficial temporal artery divides into the frontal and parietal branches.
MAXILLARY ARTERY
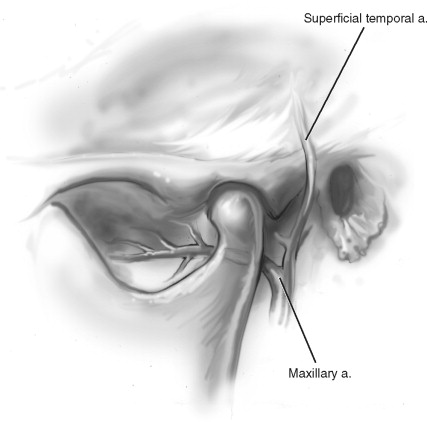
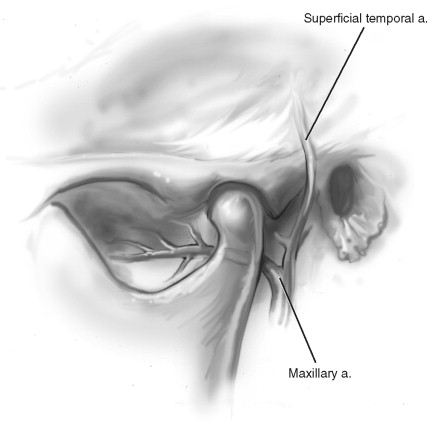
The maxillary artery is the largest terminal branch of the external carotid artery. It originates from the external carotid medial to the condylar neck at the level of the sigmoid notch. It first travels through the parotid gland posterior and medial to the condylar neck and then runs along the inferior portion of the lateral pterygoid muscle. The first portion of the maxillary artery, termed the mandibular portion, travels through the infratemporal fossa in close proximity to the medial aspect of the mandibular condyle and neck. In this region the maxillary artery divides into several branches, including the deep auricular, anterior tympanic, middle meningeal, accessory meningeal, and inferior alveolar arteries. The second portion of the maxillary artery also partitions into several branches. The masseteric artery detaches from the maxillary artery and travels through the sigmoid notch before entering the medial surface of the masseter muscle ( Figures 11-2 and 11-3 ).
RETROMANDIBULAR VEIN
The superficial temporal vein and the maxillary vein unite, forming the retromandibular vein, within the body of the parotid gland medial to the mandibular condylar neck. The retromandibular vein descends through the parotid gland superficial to the external carotid artery and deep to the facial nerve. It travels just posterior to the ramus of the mandible and divides into an anterior and a posterior portion. The anterior portion joins the facial vein and then empties into the internal jugular. The posterior portion joins the posterior auricular vein and then empties into the external jugular vein.
SUPERFICIAL TEMPORAL ARTERY
The superficial temporal artery in the pre-auricular region runs in the temporoparietal fascia just beneath the subcutaneous fat layer. The superficial temporal artery crosses lateral to the zygomatic arch and forms a single branch, the transverse facial artery. After crossing over the zygomatic arch the superficial temporal artery divides into the frontal and parietal branches.
MAXILLARY ARTERY
The maxillary artery is the largest terminal branch of the external carotid artery. It originates from the external carotid medial to the condylar neck at the level of the sigmoid notch. It first travels through the parotid gland posterior and medial to the condylar neck and then runs along the inferior portion of the lateral pterygoid muscle. The first portion of the maxillary artery, termed the mandibular portion, travels through the infratemporal fossa in close proximity to the medial aspect of the mandibular condyle and neck. In this region the maxillary artery divides into several branches, including the deep auricular, anterior tympanic, middle meningeal, accessory meningeal, and inferior alveolar arteries. The second portion of the maxillary artery also partitions into several branches. The masseteric artery detaches from the maxillary artery and travels through the sigmoid notch before entering the medial surface of the masseter muscle ( Figures 11-2 and 11-3 ).
RETROMANDIBULAR VEIN
The superficial temporal vein and the maxillary vein unite, forming the retromandibular vein, within the body of the parotid gland medial to the mandibular condylar neck. The retromandibular vein descends through the parotid gland superficial to the external carotid artery and deep to the facial nerve. It travels just posterior to the ramus of the mandible and divides into an anterior and a posterior portion. The anterior portion joins the facial vein and then empties into the internal jugular. The posterior portion joins the posterior auricular vein and then empties into the external jugular vein.
NERVES
Much of the controversy surrounding the treatment of mandibular condylar and subcondylar injuries centers on the risk of injury to motor components of the facial nerve with an open procedure. The anatomy of the facial nerve has been described in exquisite detail by many surgeons. Perhaps the most referenced is the work by Al-Kayat and Bramley. There are also sensory nerves in close proximity to both the medial and lateral aspects of the condylar head and neck that require consideration.
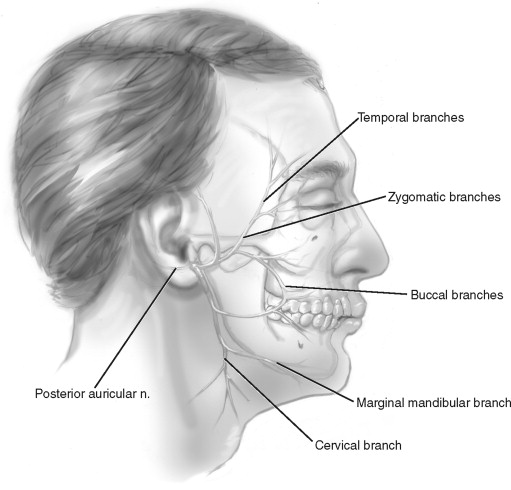
FACIAL NERVE
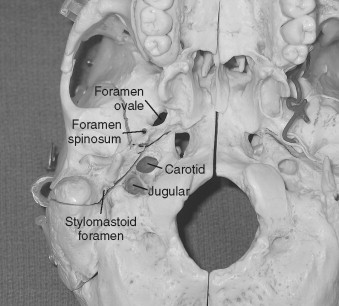
The facial nerve emerges from the brainstem and enters the internal auditory meatus. It travels through the petrous portion of the temporal bone in the facial canal and exits the skull base at the stylomastoid foramen. The main trunk of the facial nerve is 2 cm deep to the skin surface at the middle of the anterior border of the mastoid process. The posterior auricular nerve and branches to the posterior digastric and stylohyoid muscle arise from the facial nerve as it exits the skull base. The nerve then courses forward toward the parotid gland. It crosses over the styloid process, retromandibular vein, and external carotid artery before entering the parotid gland and dividing into the temporal facial and cervical facial branches. Al-Kayat and Bramley defined several anatomic landmarks that may be used to estimate the location of the facial nerve and its branches in this area. The mean distance from the lowest portion of the bony external auditory canal to the bifurcation of the facial nerve was 2.3 cm and that from the post-glenoid tubercle was 3 cm. They also found that distances from the most anterior portion of the bony external auditory canal to where the upper trunk crossed the zygomatic arch ranged from 0.8 cm to 3.5 cm. This defined the 8-mm “safe zone” for pre-auricular incisions. In the body of the parotid gland the temporal facial and cervical facial branches further divide into the nerve’s terminal branches (temporal, zygomatic, buccal, mandibular, and cervical) ( Figure 11-4 ). The temporal branch travels in, or just deep to, the temporal parietal fascia. It innervates the frontalis, corrugator, and orbicularis oculi muscles.
TRIGEMINAL NERVE
The third division of the trigeminal nerve exits the skull base through the foramen ovale. At this point the nerve is 4 cm from the skin surface and just anterior and deep to the condylar neck. After exiting the foramen ovale the third division of the trigeminal nerve consists of a large sensory root and a small motor root. The motor root supplies motor innervation to the muscles of mastication. The auricular temporal nerve is the first branch off the third division of the trigeminal nerve. It courses laterally behind the neck of the condyle and supplies sensation to the skin in the temporal and pre-auricular region, the external auditory meatus, and the tympanic membrane. The lingual nerve is the next branch. It travels in an anterior direction deep to the lateral pterygoid muscle. The nerve continues laterally, emerges from under the lateral pterygoid, and runs between the mandibular ramus and medial pterygoid muscle. The inferior alveolar nerve is initially deep to the lateral pterygoid muscle. It emerges below the inferior surface of the muscle, crosses the sphenomandibular ligament, and enters the mandibular foramen ( Figure 11-5 ).
INJURIES TO THE CONDYLAR REGION
Mandibular trauma represents a large percentage of all facial injuries. Ellis, in 1985, reported on over 2000 cases of facial trauma and found that mandibular fractures represented 45% of all facial fractures. Common causes of mandibular trauma include motor vehicle accidents, interpersonal violence, falls, and sports-related injuries. When the mandible is injured a large force is transmitted to the condyles. This transmission of force allows for a relatively high incidence of skeletal and soft tissue injuries in the condylar and subcondylar regions.
SOFT TISSUE INJURIES
Injuries to the soft tissues of the temporomandibular joint do occur with blunt trauma to the mandible but may also occur when the mandible does not appear to be directly involved in the injury. There have been many reports of disk displacement associated with rapid acceleration/deceleration or “whiplash” type injuries. It has long been recognized that damage to the soft tissue in the temporomandibular joint that occurs with trauma predisposes these joints to chronic dysfunction. Several investigators have documented radiographic and arthroscopic acute and chronic changes in the temporomandibular joints associated with mandibular trauma. Gos and Bosanquet reported acute findings on arthroscopic examination of 40 temporomandibular joints in 20 patients after mandibular trauma. They found evidence of intra-articular damage in both joints. Intra-articular damage included hyperemia of the capsule, hemarthrosis, and shredding of the disk and articular surfaces. They found that when the condyle or subcondylar region was not fractured there was more evidence of articular surface damage and in the presence of a fracture there was more evidence of disk damage. This study found no evidence of disk displacement. Jones and Van Sickels evaluated 14 TMJs arthroscopically after mandibular trauma and had similar findings. There was evidence of intra-articular damage with hemarthrosis, synovial ecchymosis, and shredding of the articular surface. They also found no evidence of disk displacement. Merrill reported his findings on 1151 arthroscopic TMJ examinations in patients with a diagnosis of internal derangement. A large subgroup (60%) of these patients had a history of mandibular trauma. At the time of examination this group was at least 1 year post trauma. In this subgroup there was evidence of damage to the disk and eminence with synovitis, adhesions, and distorted joint space anatomy. Similar to prior studies, those patients with the most severe articular surface damage had sustained mandibular trauma without a fracture in the mandibular condyle or subcondylar regions. In contrast to prior studies, 100% of these patients showed anterior/medial disk displacement. Sullivan, Bangart, and Quentin reported on the acute MRI findings of 13 condylar process fractures. Ten cases showed disk avulsion with anterior/medial displacement. There was also evidence of capsular tear and hemarthrosis involving the superior and inferior joint spaces.
SKELETAL INJURIES
In the study by Ellis, condylar and subcondylar fractures represented 29% of all mandibular fractures. In 1992 Silvennoinen reported on 382 condylar process fractures. In this study 46% of condylar process fractures were associated with other mandibular fractures. Of the condylar process fractures, 84% were unilateral (9% intracapsular, 19% condylar neck, and 72% subcondylar). Ninety percent of the condylar process fractures showed lateral override of the proximal (condylar) segment. When the anatomy of the mandibular condylar and subcondylar region is understood, the pathophysiology of injury can be predicted. When a force strikes the mandible, either directly over the condylar region or anteriorly, the condylar neck and subcondylar regions represent weak points. If the force is great enough to cause a fracture, several events occur spontaneously. The weaker medial capsule and the pull of the lateral pterygoid muscle allow the condylar head to tip medially. The pterygomasseteric sling will contract, shortening the condylar/ramus height. As the muscle contracts and the condylar head tips medially, the distal end of the condylar segment is forced laterally ( Figure 11-6 ). This is a simplified view of the most common fracture pattern. Fractures can occur at any level (condylar head, neck, or subcondylar region). Unilateral fractures are more common but fractures can occur bilaterally. To some degree the exact location and pattern of fracture are a random event. Several clinicians have developed classification schemes to describe condylar process fractures. Spiessl and Schroll, in 1972, published one of the first classifications of condylar process fractures.

SPIESSL AND SCHROLL CLASSIFICATION OF CONDYLAR PROCESS FRACTURES
The Spiessl and Schroll classification scheme used to describe condylar process fractures is as follows:
-
Type I—fracture without displacement
-
Type II—low fracture with displacement
-
Type III—high fracture with displacement
-
Type IV—low fracture with dislocation
-
Type V—high fracture with dislocation
-
Type VI—intracapsular (diacapitular)
Lindahl, in 1977, described a classification based upon three key anatomic components of the fracture. Each component is critical in the planning the treatment of condylar process injuries ( Box 11-1 ).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


