Introduction
In premolar extraction cases, root parallelism is recommended to preserve the stability of space closures. The influence of the degree of root parallelism on relapse of tooth extraction spaces has been a controversial topic in the literature. The aim of this study was to compare the angle between the long axes of the canine and the second premolarin patients with and without stability of extraction-space closures.
Methods
A sample of 56 patients, treated with 4 premolar extractions, was divided into 2 groups: group 1, consisting of 25 patients with reopening of extraction spaces; and group 2, consisting of 31 patients without reopening of extraction spaces. Panoramic radiographs of each patient were analyzed at the posttreatment and 1-year posttreatment stages. The data were statistically analyzed by using chi-square tests, t tests, analysis of variance (ANOVA), and Pearson correlation coefficients.
Results
The results showed that the groups did not differ regarding the angle between the canine and the second premolar, and there was no correlation between angular changes and reopening of extraction spaces, showing that dental angular changes are not determining factors for relapse, and other factors should be investigated.
Conclusions
The final angle and the posttreatment changes observed in the angle between the long axes of the canine and the second premolar showed no influence on the relapse of extraction spaces.
Extractions are often required in orthodontic treatment because of crowded teeth, an unesthetic facial profile, and dentoskeletal malocclusions, associated or not with an inadequate functional occlusion. Although stability is 1 goal of orthodontic treatment, reopening of extraction sites has been an unpredictable occurrence. When the first premolars are extracted, space reopening frequently produces esthetic and functional problems, because the absence of interproximal contact between adjacent teeth occurs in an esthetic area and allows food impaction in the cervical embrasure area and consequent damage to the gingival tissues. For this reason, absence of interproximal contacts between adjacent teeth can affect the occlusal force on the area, propitiating additional trauma on the periodontium.
There are many suggestions in the literature to avoid relapse of extraction spaces. Trying to prevent reopening of closed extraction sites, Edwards recommended surgical gingivoplasty associated with early and tight closure of the extraction site, adequate positions of the roots of the adjacent teeth, elimination of occlusal forces tending to separate the teeth, and appreciation for any tooth-size discrepancy in the extraction areas. This variety of procedures reflects the many factors related to relapse of extraction sites.
Some factors were cited as responsible for reopening the extraction sites: angulation of the adjacent teeth to the extraction area, without root parallelism ; unsatisfactory tooth interdigitation ; abnormal muscle function ; no bone maturation in the remodeling area due to immediate orthodontic appliance removal after obtaining the contact point ; and reaction of compressed gingival fibers.
However, the literature is conflicting regarding the prevalence and the modus operandi of these factors on extraction-site relapse. Surgical gingivoplasty and root parallelism were for a long time frequently cited procedures to eliminate or, at least, to minimize the relapse of extraction-space reopening. Currently, few studies are dedicated to this topic.
Because root parallelism is cited as a possible factor for relapse of extraction spaces, in this study, we aimed to evaluate the influence of tooth angulation on the stability of extraction-site closures in orthodontic patients treated with 4 first premolar extractions. Therefore, the following null hypothesis was investigated: there is no difference in root angulation at the end of orthodontic treatment between patients with and without relapse of extraction spaces.
Material and methods
The sample was retrospectively selected from the files of the Department of Orthodontics at Bauru Dental School, University of São Paulo, in Brazil. The inclusion criteria were patients treated with 4 first premolar extractions, all extraction sites completely closed, Class I or Class II malocclusion, complete permanent dentition, standard edgewise appliances, no dental anomalies of number (agenesis or supernumerary teeth), no periodontal surgery in the extraction area, no occlusal adjustment at the end of the treatment, satisfactory occlusal results, and the same retention protocol. According to these inclusion criteria, 56 patients between 12 and 22 years of age were selected and divided into 2 groups with the following characteristics ( Table I ).
| Measurement 1 | Measurement 2 | n | P | Dahlberg | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||||
| Tooth angulation | 0.16 | 8.05 | 0.36 | 8.05 | 80 | 0.485 | 1.797 |
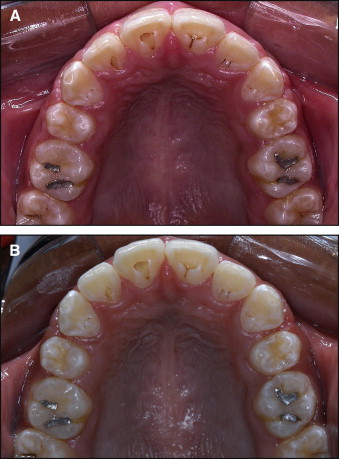
Group 1 included 25 patients (8 male, 17 female) who had relapse of extraction spaces in 62 quadrants (29 in the maxillary arch, 33 in the mandibular arch), as shown in Figure 1 , with the maxillary spaces reopening. Eight patients had Class I and 17 had Class II malocclusions at the pretreatment stage. The mean age at the end of treatment was 16.56 ± 2.16 years (range, 12.58-22.77 years). The posttreatment observation time was 1.61 ± 0.87 years.
Group 2 consisted of 31 patients (19 male, 12 female) with no relapse of extraction spaces. Eleven patients had Class I and 20 had Class II malocclusions at the pretreatment stage. The mean age at the end of treatment was 15.28 ± 1.38 years (range, 12.32-17.89 years). The posttreatment observation time was 1.49 ± 1.11 years.
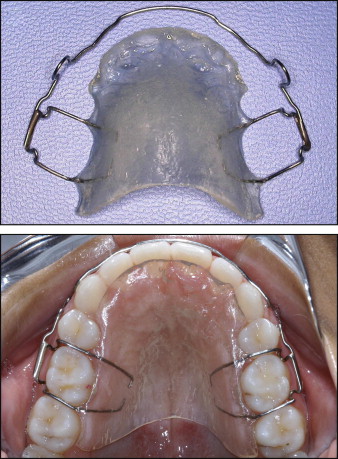
Orthodontic mechanics included 0.022 × 0.028-in fixed standard edgewise appliances and extraction of 4 first premolars. Patients with severe initial anterior tooth crowding required canine retractions, followed by leveling and alignment with the usual wire sequence characterized by an initial 0.015-in twist-flex or a 0.016-in Nitinol, followed by 0.016-, 0.018-, 0.020-, and 0.019 × 0.025-in stainless steel archwires (3M Unitek, Monrovia, Calif). Deepbite was corrected with accentuated and reversed curve of Spee. The extraction spaces were closed with en-masse retraction of the anterior teeth, with elastic chains on a rectangular archwire. At the end of treatment, the canines and the second premolars were in contact. Also, a Class I molar relationship and satisfactory overbite and overjet relationships were obtained. A modified Hawley retainer was used in the maxillary arch, and a canine-to-canine retainer was bonded in the mandibular arch. The Hawley retainer had its labial arch welded to the horizontal bar of the Adams clasp, without auxiliary clasps or occlusal interference between the canine and the premolar ( Fig 2 ). The Hawley retainer was recommended to be used full-time for 6 months, followed by nights-only use for 6 months. The mandibular canine-to-canine bonded fixed retainer was used for a mean period of 3 years. Twenty patients of group 1 (80%) and 24 (77.4%) of group 2 were still using their Hawley retainers at the time of evaluation.
Panoramic radiographs from each patient were evaluated at the final and the 1-year posttreatment stages. The maxillary and mandibular teeth up to the first molars were delimited by 1 operator (C.T.A.) in a dark room. Then, the long axes of the maxillary and mandibular canines and second premolars were traced following the root canal path, without considering apical dilacerations ( Fig 3 ). Angulations between those teeth were measured, by using positive values for long axes that converged occlusally and negative values for long axes that converged toward the apex.
Tooth angulation was classified according to the angulation between the long axes of the canines and the second premolars at the end of treatment ( Table II ): satisfactory parallelism from −6° to +6°, apical convergence of less than −7°, or apical divergence of more than +7°.
| Characteristics | Group 1 (n = 25) | Group 2 (n = 31) | P |
|---|---|---|---|
| Malocclusion type | |||
| Class I | 8 (32%) | 11 (35%) | P = 0.784 |
| Class II | 17 (68%) | 20 (65%) | χ 2 = 0.75 |
| Final age (y) | 16.56 ± 2.16 | 15.28 ± 1.38 | P = 0.009 ∗ ( t test) |
| Posttreatment observation time (y) | 1.61 ± 0.87 | 1.49 ± 1.11 | P = 0.663 ( t test) |
The relapse amount was measured as the distance between the distal surface of the canines to the mesial surface of the second premolars on dental casts at the 1-year posttreatment stage.
Twenty randomly selected panoramic radiographs were retraced and remeasured to verify the error of the method. Casual errors were calculated according to Dahlberg’s formula (S = Σ d 2 /2n), and systematic errors were evaluated with dependent t tests at P <0.05.
Statistical analysis
Intergroup malocclusion type distributions were compared with chi-square tests, and posttreatment ages and observation times were compared with t tests.
To compare the final tooth angulations between groups 1 and 2, t tests were used. The chi-square test was used to compare the root-angulation categories between the groups. To compare the amount of relapse between the 3 angulation categories in group 1, 1-way analysis of variance (ANOVA) was used.
To investigate any significant correlation between angular changes and the amount of relapse of the extraction spaces in group 1, the Pearson correlation coefficient was used.
Results
There were no statistically significant systematic errors ( P = 0.485), and the casual error was within acceptable limits, as shown in Table I .
The groups were similar regarding the distribution of malocclusion types and follow-up periods, but group 1 had a greater final mean age than group 2 ( Table II ). There was no statistically significant difference between the groups regarding the angle between the canine and the second premolar and regarding the percentages of the root-angulation categories at the end of treatment ( Tables III and IV ). There was no statistically significant difference in the amount of relapsed space between the parallel, convergent, and divergent roots in group 1 ( Table V ). There was no significant correlation between the posttreatment angulation changes and the amount of space relapse ( Table VI ).



