Introduction
One common negative side effect of orthodontic treatment with fixed appliances is the development of incipient caries lesions around brackets, particularly in patients with poor oral hygiene. Bio-available minerals from cement containing amorphous calcium phosphate (ACP) might facilitate remineralization and inhibit lesion development. Our objective was to compare the potential of ACP-containing resin cement, fluoride varnish, resin sealer, and MI Paste (GC America, Alsip, Ill) under similar in-vitro conditions to prevent incipient caries lesions next to brackets on teeth.
Methods
One hundred extracted premolars were randomly allocated to 5 groups (n = 20). Brackets were bonded with ACP cement (Aegis-Ortho, Bosworth, Skokie, Ill), resin (Transbond XT [3M Unitek, Monrovia, Calif], control), or resin followed by application of fluoride varnish (Vanish, 3M, St Paul, Minn), resin sealer (Pro-seal, Reliance Orthodontic Products, Itasca, Ill), or casein phosphopeptide-ACP paste (MI Paste). All groups were cycled for 15 days in demineralization solution for 8 hours a day, rinsed, placed in artificial saliva (30 minutes), brushed, and stored overnight in artificial saliva. The extent of demineralization in each group was assessed by using quantitative light-induced fluorescence and confocal laser scanning microscopy.
Results
Only the Pro-seal and Vanish groups showed significantly smaller lesions than the controls (Kruskal-Wallis test, P <0.05) for both quantitative light-induced fluorescence and confocal laser scanning microscopy measurements. Fluorescence loss of Aegis-Ortho was similar to Vanish; Aegis-Ortho, MI Paste, and the controls were not different from each other.
Conclusions
Both light-cured filled resin (Pro-seal) and fluoride varnish (Vanish) might prevent enamel demineralization next to orthodontic brackets exposed to cariogenic conditions, but the observed positive effects of Aegis-Ortho and MI Paste were not significant.
One of the most common negative side effects of orthodontic treatment with fixed appliances is the development of incipient caries lesions around brackets and bands, particularly in patients with poor oral hygiene. Incipient caries lesions (white spots) are characterized by their opacity and mineral loss compared with healthy enamel. Studies have shown that white spot lesions (WSL) can take only 1 month to develop. A clinical study reported the prevalence at 50%, although recent investigations put the incidence of WSL during orthodontic treatment with fixed appliances at 73% to 95%.
Orthodontists have turned to various products and preventive measures to reduce this problem. Dental professionals have used fluoride for years to prevent caries and remineralize enamel in patients. A significant reduction in enamel lesions can be achieved during orthodontic therapy through the daily use of neutral 0.05% sodium fluoride rinse, although typical patient compliance rates with this protocol have been relatively low. Professional fluoride varnish application by orthodontic auxiliaries at routine appointments addresses the compliance issue. Although fluoride varnish does not totally prevent formation of WSL, their incidence can be significantly reduced. In a prospective clinical study, 44.3% fewer caries lesions were noted for teeth that had been treated with fluoride varnish during orthodontic treatment.
Just as sealants prevent caries in molars with deep fissures, resin sealers have been applied on the facial surfaces of bracketed teeth to prevent enamel demineralization. Early generations of resin sealers showed low wear resistance. A more recently developed product, Pro-seal (Reliance Orthodontic Products, Itasca, Ill), has been marketed as a fluoride-releasing sealer that is more resistant to toothbrush abrasion than earlier generations, since it is a highly filled resin. An in-vitro study found that demineralization was significantly less with Pro-seal treatment, compared with the controls. It was also found that Pro-seal can stand up to acid challenges and toothbrush abrasion in a laboratory environment. In a second in-vitro study, it was found that Pro-seal provided significantly more protection than either fluoride varnish or an unfilled resin sealer, with a 92% reduction in lesion depth compared with the controls.
Recently, there has been increased interest in calcium phosphate-based remineralization technology. One of the newest modalities in preventive dentistry is the introduction of amorphous calcium phosphate (ACP) into methacrylate composites, gum, pastes, and other dental products. Aegis-Ortho (Bosworth, Skokie, Ill) is a resin bonding cement, with the potential added benefit of caries prevention. The manufacturer claims that the acidic challenge to the surrounding bracket area triggers the release of calcium and phosphate from the cement, and a supersaturated calcium phosphate matrix will not only inhibit demineralization, but also remineralize the enamel. Aegis-Ortho has the advantage that it does not require patient compliance or additional chair time in the orthodontic office.
A similar chemical process is expected from MI Paste (GC America, Alsip, Ill). This paste containing casein phosphopeptide-ACP (CPP-ACP) is applied topically to affected areas. The manufacturer not only states that this product prevents lesion formation, but also claims that the patient can expect complete reversal of such lesions when used for 3 months after the brackets are debonded. One laboratory study found a mild decrease in demineralization with the application of CPP-ACP compared with the controls but recommended combining CPP-ACP with fluoride varnish to enhance the treatment effect. A recent systematic literature review found insufficient clinical trial evidence to make a recommendation regarding the long-term effectiveness of casein derivatives, specifically CPP-ACP, in preventing caries in vivo.
With all the treatment modalities flooding the market, orthodontists might find it difficult to sort out what works best and why it is efficacious when oral hygiene deteriorates. The primary objective of this study was to investigate the potential of ACP-containing resin cement and other treatments (fluoride varnish, resin sealer, and MI Paste) under similar in-vitro conditions to prevent incipient caries lesion development next to bracketed teeth.
Material and methods
One hundred premolars were collected from various oral surgery practices in southeast Michigan. Upon collection, the teeth were washed in tap water and stored at 4°C in 0.1% thymol solution. Only carefully selected premolars with a healthy facial enamel surface were included.
The premolars were randomly assigned to 5 groups of 20 each. In the first group, the brackets were bonded with Aegis-Ortho resin cement. In the remaining 4 groups, the brackets were bonded with Transbond XT (3M Unitek, Monrovia, Calif). Of the 4 groups receiving the Transbond XT bonding, 1 served as the control group and 3 as the experimental groups: Vanish fluoride varnish (5% sodium fluoride white varnish [3M, St Paul, Minn]), MI Paste, and Pro-seal.
The roots of the premolars were sectioned and discarded, and the remaining crowns were embedded in acrylic.
The bracket was placed 2 mm gingivally to the buccal cusp tip and in the mesiodistal center of the clinical crown.
To standardize and limit the enamel area exposed to the etching and bonding procedures, the enamel surface was protected by adhesive tape during all adhesive procedures. By using a hole puncher, a window was cut from the adhesive tape, leaving an enamel area the size of the orthodontic bracket base exposed. A metal orthodontic bracket was bonded to each tooth by using a light-cured bonding resin, depending on the group assignment. Universal premolar brackets, Victory Series (3M Unitek) with a 0.022-in slot and 0° of tip and torque, were used in this study.
Each tooth was cleaned with nonfluoridated pumice with a rubber prophy cup on a slow-speed hand piece. Remaining residue was washed away with tap water, and each tooth was thoroughly dried for 15 seconds. For all groups, the enamel window in the tape was etched for 30 seconds with 35% phosphoric acid gel (Bosworth), rinsed with water for the same amount of time, and dried with compressed air.
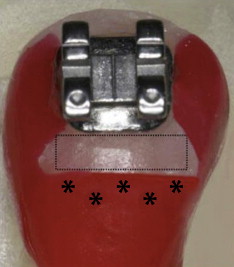
For the Aegis-Ortho group, Aqua bond (Bosworth) was used as the primer. For the remaining groups having Transbond XT adhesive cement, Transbond XT primer (3M Unitek) was selected as the bonding agent. Immediately after the adhesive was applied, each bracket was placed onto its tooth surface, and excess adhesive was removed. The resin was light-cured with an Ortholux LED curing light (3M Unitek) for 10 seconds. The adhesive tape was removed from each tooth. To avoid interference of general tissue demineralization of the crown, the entire tooth was covered by varnish except for the area of interest. All teeth were painted with a thin coat of acid-resistant nail varnish (Revlon, New York, NY) on all surfaces except the 1.0 to 1.5 mm area gingival to the bracket, leaving a small rectangular box exposed for demineralization ( Fig 1 ). For quantitative light-induced fluorescence (QLF) measurements, this exposed enamel was compared with the nail varnish-covered area of unexposed enamel just gingival to the box.
Teeth in the varnish group were dried, and the exposed enamel box was painted with Vanish. The varnish was allowed to dry for 5 minutes. Teeth in the CPP-ACP group were also dried, and the exposed enamel in the box was painted with a pea-size amount of MI Paste with a cotton swab. It was left undisturbed for 3 minutes. The MI Paste on each tooth was removed with a cotton roll and allowed to sit for another 2 minutes. Finally, the remaining residue was washed away with tap water. Following the manufacturer’s instructions, we applied the MI Paste daily during the experiment. The teeth in the resin sealer group were acid-etched in the exposed enamel box, and a layer of Pro-seal resin was applied. The Pro-seal was cured for 20 seconds with the curing light.
The groups were cycled in a demineralization solution for 8 hours per day. The demineralization solution was based on lactic acid and Carbopol C907 (Lubrizol, Wickliffe, OH) (pH 5.0), 50% saturated with hydroxyapatite. The solution was refreshed daily during the experimental period of 15 days.
After 8 hours of exposure to the caries-like challenge, all teeth in each group were rinsed with water and placed in artificial saliva for 30 minutes. The teeth were cleaned in no particular order with a Sonicare FlexCare power toothbrush (Philips Electronics North America Corp, Andover, MA). The brush bristles were rinsed with water, and a pea-size amount of Crest Cavity Protection toothpaste (1,100 ppm sodium fluoride, Procter & Gamble, Cincinnati, Ohio) was applied to the brush. The brush was lightly applied to the exposed enamel box for 2 seconds per tooth. After the 5 groups were separately brushed and rinsed with tap water, they were placed once again in the artificial saliva solution for approximately 15 hours until the cycle was repeated. With the MI Paste group only, the teeth were removed from the artificial saliva solution 10 minutes before the next demineralization period started to receive an MI Paste application.
On day 15, all teeth were removed from the saliva solution, rinsed under tap water, and stored in 100% humidity. The remaining fluoride varnish residue on the teeth from the Vanish group was removed with a plastic scaler.
To assess demineralization, QLF and confocal laser scanning microscopy (CLSM) were used. Both procedures were carried out at the Oral Health Research Institute, Indiana University, Indianapolis, Ind. The use of QLF as a quantitative measurement tool has the advantage of being noninvasive, and it can be applied clinically. CLSM, on the other hand, using sections of teeth, allows for a more accurate, quantitative analysis of surface and subsurface areas, providing enamel lesion depth data in larger tissue sections. These methods are complementary.
QLF images were taken of all teeth. To calculate fluorescence loss, a computer-generated rectangle (approximately 1.5 × 4.0 mm 2 ) captured the enamel gingival to the bracket region. The fluorescence values of the pixels in the rectangle exposed to the treatments and cycling were compared with the fluorescence values of a control area of a similar size: a relevant enamel area that was previously covered by nail varnish during the cycling. The value obtained was the average change in fluorescence (fluorescence loss:ΔF) of the pixels under the threshold.
For CLSM, a casting resin (Meyers Plastics, Indianapolis, Ind) was applied on top of each specimen and allowed to polymerize overnight. An approximately 1-mm thick section was obtained from each specimen by using a Silverstone-Taylor hard-tissue microtome (Scientific Fabrications Laboratory, Lafayette, Colo). Each section was stained overnight with a 0.1-mmol/L solution of Rhodamine B (Aldrich Chemical, Milwaukee, Wis). The stained surfaces of each specimen’s section were allowed to air dry before being analyzed with a confocal microscope (LSM510-META, Carl Zeiss Microimaging, Thornwood, NY) to determine the extent of the lesions. The images were examined with Metamorph software (version 4.1.6, Universal Images, West Chester, Pa). After being brought into focus (by using a 10-times Plan Neofluar objective, N.A. 0.3, Carl Zeiss Microimaging), the specimens were illuminated with an argon laser with a 543-nm excitation wavelength. Confocal slits were set at 82 μm with a 580 to 633 nm filter, and the argon laser intensity was set at 20%. Areas were scanned planoparallel to the transversal cut surface of the specimen and perpendicular to the natural surface of the tooth. The value obtained was the lesion depth in the area of exposed enamel.
Statistical analysis
Descriptive statistics were calculated. All 5 groups of 20 teeth were statistically compared with a Kruskal-Wallis rank test to detect any differences with respect to QLF and CLSM. Post-hoc Tukey comparison tests were performed to identify significant between-group differences for average fluorescence changes for QLF and lesion depth for CLSM.
The results were considered significant at P <0.05. The statistical analysis was performed by using SPSS software (version 12.0.1, SPSS, Chicago, Ill).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


