Patients with a dentofacial skeletal deformity have not only esthetic and morphologic problems related to facial proportions and dentition, but also problems of stomatognathic functions. Therefore, in addition to morphologic analysis, functional analysis is important for the diagnosis and evaluation of treatment in these patients. However, no reports have described longitudinal simultaneous evaluations of stomatognathic functions, and the comprehensive effects of surgical orthodontics on the stomatognathic functions are unclear. A patient was diagnosed as having a skeletal Class III jaw-base relationship, mandibular asymmetry, unilateral crossbite, asymmetric stomatognathic functions, and a temporomandibular disorder. She was treated with a combination of surgery and orthodontic therapy. As a result, facial proportions and occlusion improved; in particular, asymmetric stomatognathic functions, including masticatory muscle activity, condylar movement, and occlusal force, became symmetric between the left and right sides. Moreover, after 2 years of retention, the activity of the masticatory muscles and the values of occlusal force and occlusal contact area exceeded those at pretreatment. These results suggest that improvement of asymmetric stomatognathic functions can be achieved by correction of dentofacial morphology by surgical orthodontic treatment in patients with mandibular asymmetry.
Patients with a dentofacial skeletal deformity have not only esthetic and morphologic problems related to facial proportions and the dentition, but also problems of stomatognathic functions, such as masticatory muscle activity, mandibular and condylar movement, and occlusal force. Therefore, in addition to morphologic analysis, functional analysis is important for the diagnosis and evaluation of treatment results in these patients. Some previous case reports presented findings of stomatognathic function. Maeda et al and Nakajima et al reported improvement of electromyographic activity of the masseter and temporalis muscles in surgical orthodontic cases with maxillary and mandibular prognathism, respectively. Furthermore, orthognathic surgery for patients with unilateral crossbite and occlusal cant resulted in correction of asymmetric incisal and condylar paths using a 6 degrees of freedom jaw movement recording system. However, although masticatory muscle activity, occlusal force, and condylar movement are all important factors for normal stomatognathic function, they were only individually evaluated in previous case reports, and the comprehensive effects of surgical orthodontics on stomatognathic function is unclear.
The prevalence of temporomandibular disorder (TMD) symptoms, such as joint sounds and pain, limited opening of the mouth, and articular disc displacement, was found to be higher in patients with mandibular prognathism and mandibular asymmetry than in those without mandibular asymmetry. In contrast, Goto et al reported that although the temporomandibular joint (TMJ) on the deviated side showed a higher incidence of disc displacement in patients with mandibular asymmetry, clinical TMD symptoms showed no difference between the deviated and nondeviated sides. On the other hand, it has been reported that TMD symptoms can be improved by orthognathic surgery in patients with mandibular prognathism. Therefore, diagnosis and posttreatment evaluation of the TMJ are important for patients with mandibular asymmetry and prognathism treated by orthognathic surgery.
Magnetic resonance imaging is useful to make a diagnosis of the TMJ because of its capacity to evaluate the soft and hard tissues without physical invasion. Anteroposterior and transverse disc displacements are diagnosed by sagittal and coronal magnetic resonance images, respectively. However, the transverse disc position in patients with mandibular asymmetry is not well known.
This case report describes a skeletal Class III patient with mandibular asymmetry and unilateral crossbite treated by a combination of surgery and orthodontic therapy. For the first time, we longitudinally evaluated changes of occlusion, skeletal morphology, and stomatognathic functions such as masticatory muscle activity, occlusal force, condylar movement, and anteroposterior and transverse disc positions. As a result, it was suggested that the improvement of asymmetric stomatognathic functions can be achieved by correction of dentofacial morphology by surgical orthodontics in patients with mandibular asymmetry.
Diagnosis and etiology
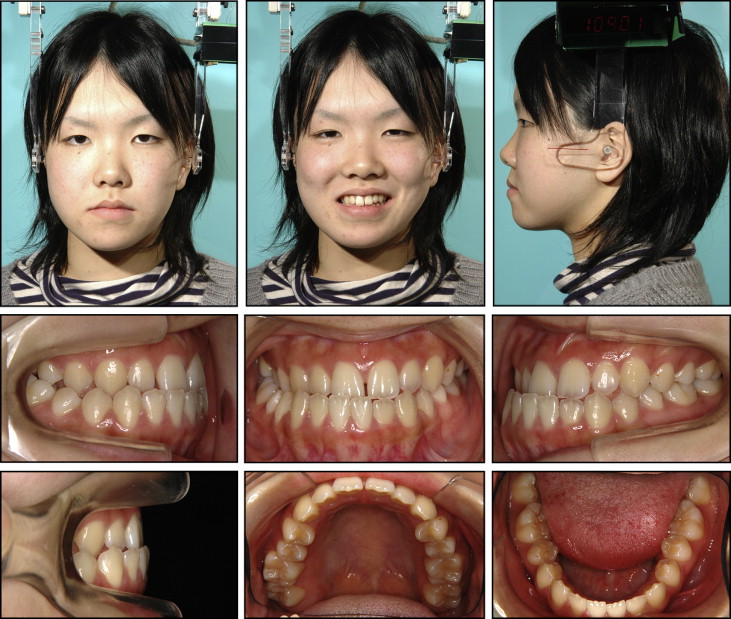
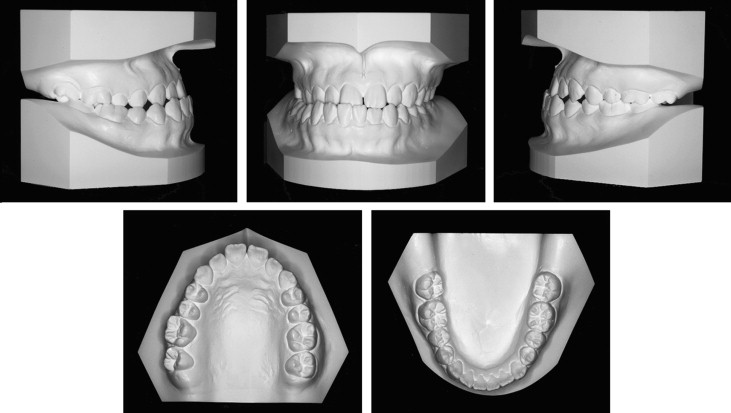
A young woman, age 18 years 8 months, came to the outpatient clinic of Tohoku University Hospital in Japan. Her chief complaints were mandibular protrusion and facial asymmetry. The facial photographs showed a mandibular deviation toward the right and a concave profile ( Fig 1 ). The mandibular dental midline was deviated 3.5 mm toward the right compared with the maxilla, and she had anterior and right posterior crossbites ( Figs 1 and 2 ). The molar relationships were Class III on both sides. Overjet and overbite were –1.5 and 2 mm, respectively ( Figs 1 and 2 ). A panoramic radiograph showed that all third molars were impacted ( Fig 3 ). The cephalometric analysis showed a skeletal Class III jaw-base relationship, an average mandibular plane angle, and normal inclinations of the maxillary and mandibular anterior teeth ( Fig 3 , Table I ). The posteroanterior cephalogram showed a mandibular deviation toward the right of 4 mm.

| Measurement | Japanese norm (adult) | Pretreatment | Posttreatment | Postretention | |
|---|---|---|---|---|---|
| Mean | SD | ||||
| Angular (°) | |||||
| SNA | 80.8 | 3.6 | 82.3 | 82.3 | 82.2 |
| SNB | 77.9 | 4.5 | 82.9 | 80.8 | 80.6 |
| ANB | 2.8 | 2.4 | −0.6 | 1.6 | 1.6 |
| Mp-SN | 37.1 | 4.6 | 34.6 | 37.4 | 37.1 |
| Gonial angle | 122.1 | 5.3 | 130.1 | 132.2 | 132.6 |
| U1-SN | 105.9 | 8.8 | 107.7 | 106.1 | 106.5 |
| L1-FH | 56.0 | 8.1 | 61.3 | 60.0 | 60.0 |
| L1-Mp | 93.4 | 6.8 | 90.4 | 89.2 | 89.0 |
| IIA | 123.6 | 10.6 | 127.3 | 127.3 | 127.4 |
| Linear (mm) | |||||
| S-N | 67.9 | 3.7 | 75.0 | 74.7 | 74.6 |
| N-Me | 125.8 | 5.0 | 130.6 | 129.4 | 129.6 |
| Me/NF | 68.6 | 3.7 | 71.8 | 70.8 | 70.7 |
| Ans-Ptm/NF | 52.1 | 3.0 | 59.3 | 59.6 | 59.7 |
| Go-Me | 71.4 | 4.1 | 78.4 | 76.3 | 76.2 |
| Ar-Go | 47.3 | 3.3 | 49.9 | 47.6 | 47.5 |
| Ar-Me | 106.6 | 5.7 | 118.7 | 115.3 | 115.0 |
| Overjet | 3.1 | 1.1 | −2.6 | 1.7 | 1.5 |
| Overbite | 3.3 | 1.9 | 1.2 | 1.2 | 1.3 |
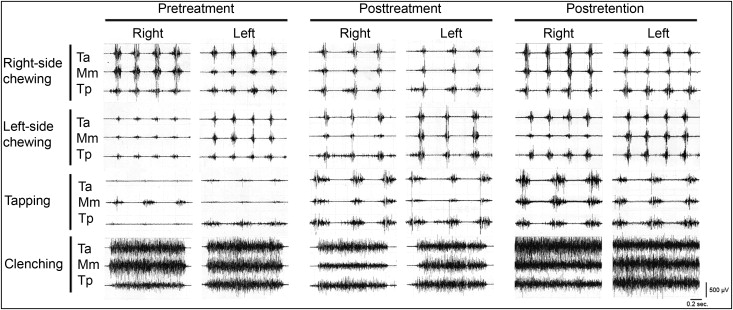
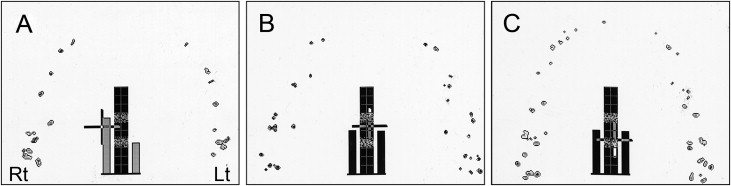
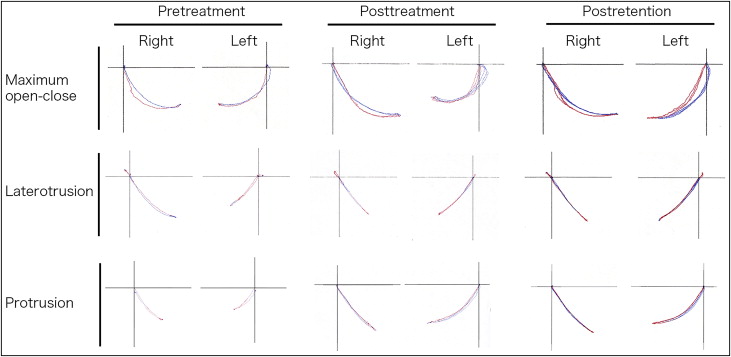
Electromyographic monitoring showed that activities of the masseter and anterior and posterior temporalis muscles were lower during unilateral chewing on the left side than on the right side ( Fig 4 ). During tapping, the masseter muscle was mainly activated on the right side; in contrast, the posterior temporalis muscle was mainly activated on the left side. An occlusal-force recording system showed higher values of occlusal force and occlusal contact area on the right side than on the left ( Fig 5 , A ; Table II ). A 6 degrees of freedom jaw movement recording system showed that condylar path length was shorter on the left side than on the right during lateral and protrusive jaw movements ( Fig 6 , Table III ). Manipulation of the TMJ elicited clicking sounds on the left side. The sagittal magnetic resonance images showed anterior articular disc displacement with reduction on the right TMJ ( Fig 7 , A and C ). In contrast, a normal disc position was shown on the left side ( Fig 7 , B and D ). The coronal magnetic resonance images did not show a transverse displacement of the disc on the right side ( Fig 7 , E and G ). On the left side, lateral displacement of the anterior band of the disc was shown in the closed-mouth position, but not in the open-mouth position ( Fig 7 , F and H ).
| Pretreatment | Posttreatment | Postretention | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Total | Right | Left | Total | Right | Left | Total | Right | Left | |
| Occlusal force (N) | 735.2 | 475.7 | 259.5 | 518.2 | 263.4 | 254.8 | 837.3 | 422.0 | 415.3 |
| % | 100 | 64.7 | 35.3 | 100 | 50.8 | 49.2 | 100 | 50.4 | 49.6 |
| Occlusal contact area (mm 2 ) | 17.1 | 10.6 | 6.5 | 11.3 | 5.9 | 5.4 | 23.4 | 12.4 | 11.0 |
| % | 100 | 62.0 | 38.0 | 100 | 51.9 | 48.1 | 100 | 52.9 | 47.1 |
| Condylar path length (mm) | Pretreatment | Posttreatment | Postretention |
|---|---|---|---|
| Maximum open-close | |||
| Right | 12.8 | 16.4 | 17.2 |
| Left | 11.5 | 11.2 | 15.6 |
| Laterotrusion | |||
| Right | 11.2 | 8.5 | 9.8 |
| Left | 6.9 | 9.0 | 9.7 |
| Protrusion | |||
| Right | 7.2 | 10.6 | 11.0 |
| Left | 5.9 | 12.1 | 11.8 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


